(UroToday.com) The 2024 Southeastern Section of the AUA (SESAUA) annual meeting featured a kidney cancer session and a presentation by Dr. Edouard Nicaise discussing the safety and efficacy of surgery in metastatic and non-metastatic renal cell carcinoma (RCC) with supradiaphragmatic tumor thrombus involving cardiac procedures. Invasion of the inferior vena cava (IVC) is a unique feature of RCC, and tumor thrombus extension into the supradiaphragmatic IVC carries high morbidity and mortality attributable to surgical complexity. However, it is unclear whether safety and efficacy have been shown to warrant cytoreductive surgery for metastatic RCC with concomitant thrombus. At SESAUA 2024, Dr. Nicaise and colleagues presented outcomes of cytoreductive and non-cytoreductive radical nephrectomy with supradiaphragmatic tumor thrombectomy involving cardiac surgery.
The authors reviewed the nephrectomy database at Emory University for patients with supradiaphragmatic thrombus and confirmed RCC. Radical nephrectomy with caval thrombectomy was performed by a single team involving urology, surgical oncology, and cardiothoracic surgery. Rank Sum for numerical variables and chi-square for categorical variables were used to test for differences between cytoreductive and non-cytoreductive radical nephrectomy. Kaplan Meier curves estimated cancer-specific survival and overall survival.
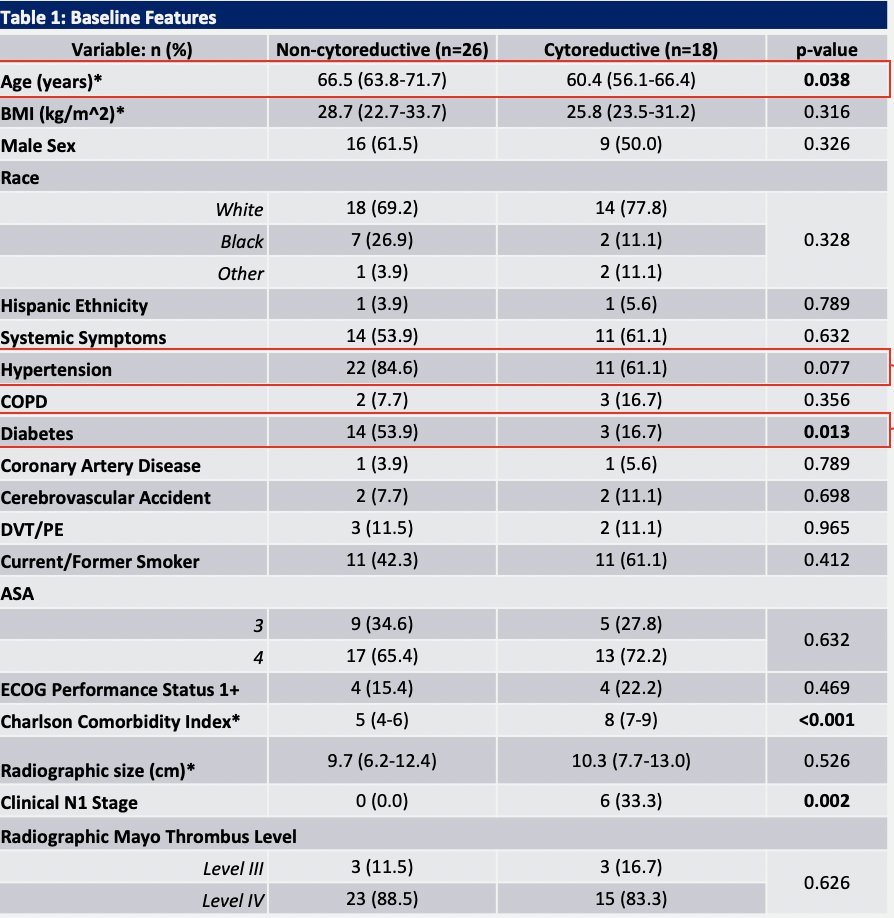
From 2006-2023, 44 patients fit the inclusion criteria for this study and underwent radical nephrectomy, of which 18 (40.9%) were cytoreductive. Cytoreductive patients were younger (61 vs. 67, p = 0.038), and had lower rates of hypertension (61% vs. 85%, p = 0.077) and diabetes (17% vs. 54%, p = 0.013):
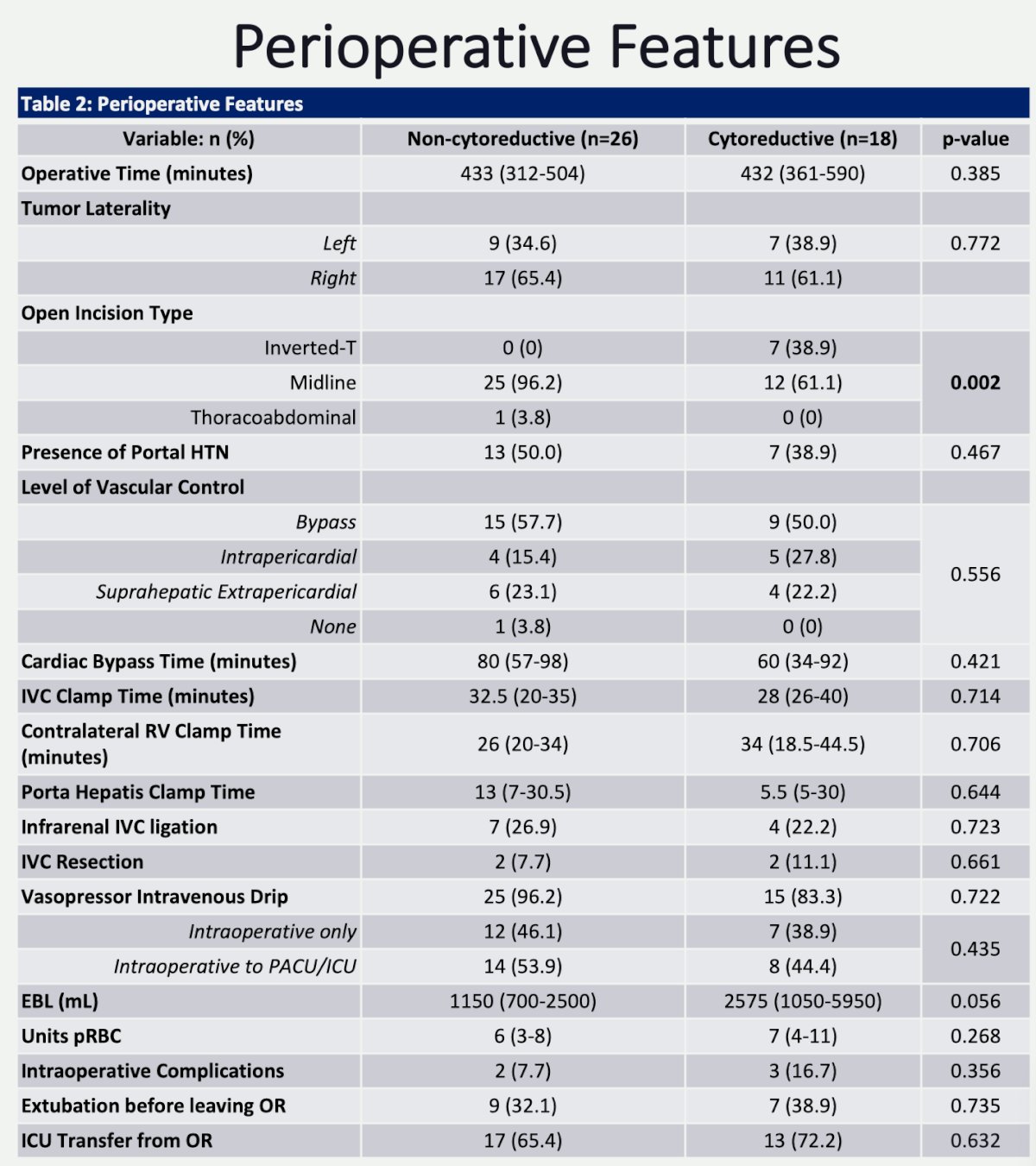
With regards to perioperative features, operative time (432 vs. 433 min, p=0.385), IVC clamp time (28 vs. 32.5 min, p=0.714), contralateral renal vein clamp time (34 vs. 26 min, p=0.706), and cardiac bypass time (60 vs. 80 minutes, p=0.421) were similar between cytoreductive vs non-cytoreductive approaches. However, there was increased blood loss with the cytoreductive approach (2.6 L vs 1.2 L, p = 0.056):
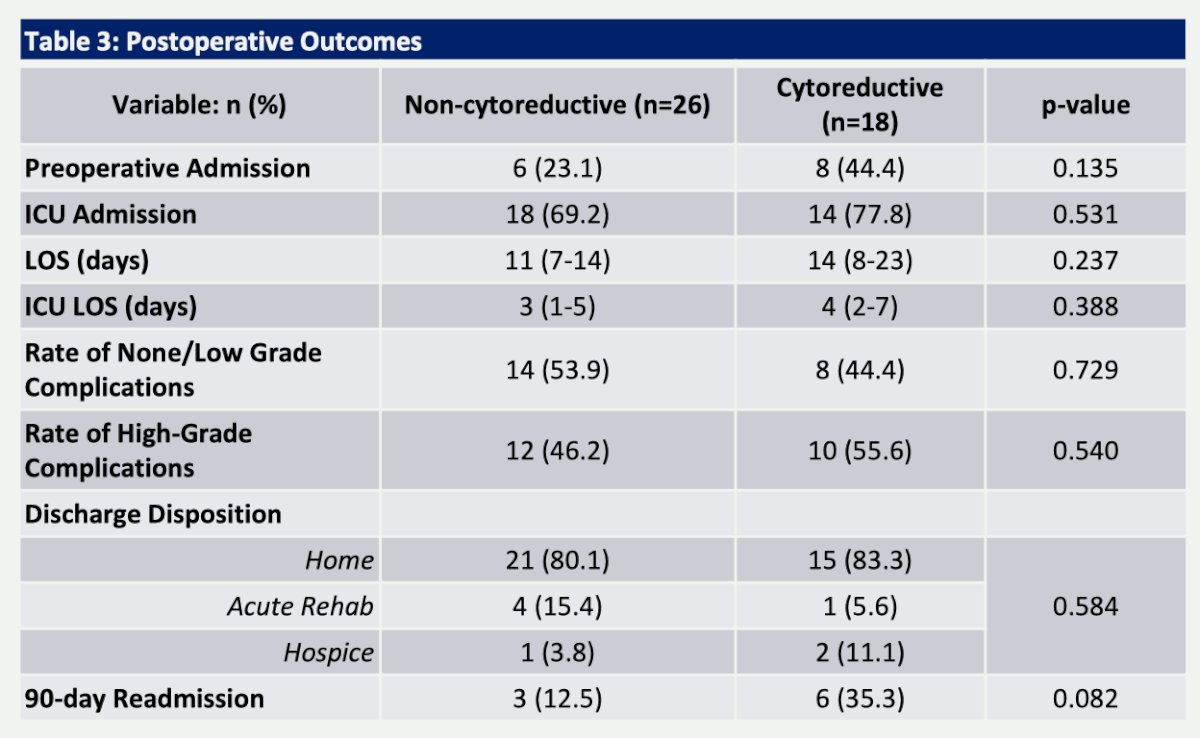
ICU admission was common, between 70-78%, but no major differences in ICU or hospital length of stay were noted between the groups. However, patients and families should be counseled to expect a 1-2 week hospitalization. Rate of high-grade complications was nearly 50%, albeit some of this was precautionary given the need to transfer or monitor in the ICU. Of the complications, the most common were anemia requiring transfusion (58-67%), ileus (11-27%), and atrial fibrillation (17-19%):
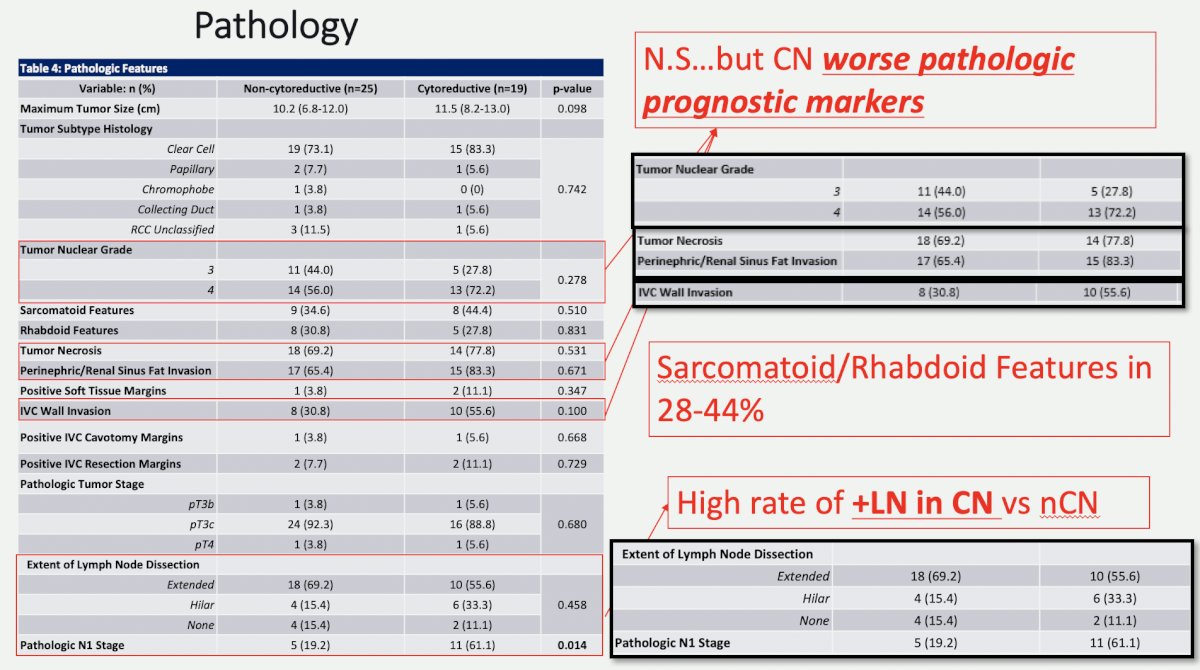
Cytoreductive nephrectomy patients had worse pathologic prognostic markers: 16% absolute increase in G4 disease, 9% more tumor necrosis, 20% more perinephric/renal sinus fat invasion, and 25% more IVC wall invasion. Additionally, both cavotomy and resection margins were slightly higher in the cytoreductive nephrectomy group. Overall, 85-90% of patients had a lymph node dissection, with node positivity rate ranging from 20 to 61%:
Of note, neoadjuvant therapy was not commonly used, with only 3 non-metastatic patients and 1 metastatic patient receiving therapy. With a median follow-up of 22 months, patients with non-metastatic RCC had a 5-year overall survival of 56.2% and 5-year cancer specific survival of 80.1%. However, for metastatic patients, 5-year survival rates were poor at 11-12%:
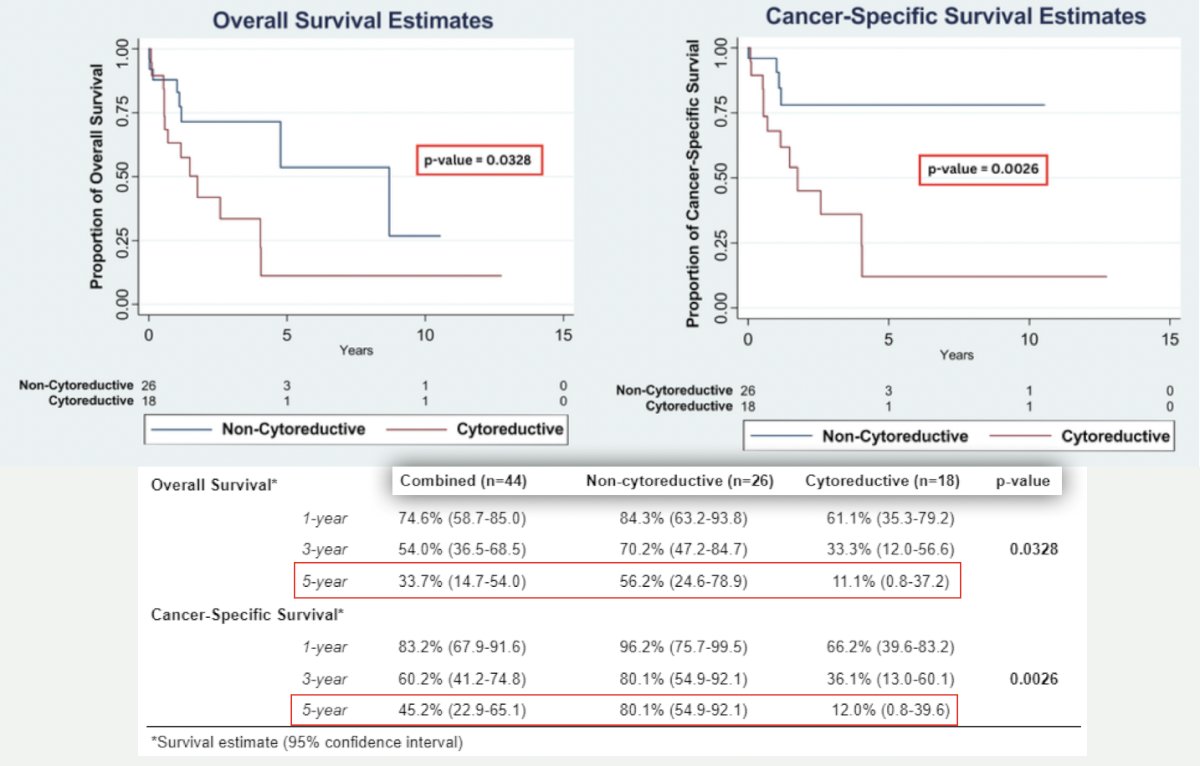
Dr. Nicaise concluded his presentation by discussing the safety and efficacy of surgery in metastatic and non-metastatic renal cell carcinoma with supradiaphragmatic tumor thrombus involving cardiac procedures with the following conclusions:
- Radical nephrectomy with supradiaphragmatic tumor thrombectomy is safe with durable treatment response in patients with non-metastatic RCC
- Although the safety of cytoreductive radical nephrectomy is comparable, further investigation into the role of neoadjuvant therapy is recommended given the 5-year survival estimates of ~11-12%
Presented by: Edouard Nicaise, MD, Emory University School of Medicine, Atlanta, GA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Southeastern Section of the American Urological Association (SESAUA) Annual Meeting, Austin, TX, Wed, Mar 20 – Sat, Mar 23, 2024.


