(UroToday.com) The 2024 Southeastern Section of the AUA (SESAUA) annual meeting featured a bladder cancer session and a presentation by Dr. Lila McGrath discussing non-narcotic compliance and clinical outcomes in Enhanced Recovery After Surgery (ERAS) cystectomy patients. Non-narcotic analgesia is a central component of ERAS protocols which have been shown to decrease narcotic utilization after radical cystectomy.
However, the effect of individual non-narcotic analgesics on clinical outcomes in cystectomy ERAS patients is unknown, especially given variability in post-operative non-narcotic regimens. At the 2024 SESAUA annual meeting, Dr. McGrath and colleagues reported on the association between non-narcotic compliance rates and clinical outcomes, including length of stay and time to bowel movement within a well-established ERAS cystectomy protocol.
This study retrospectively reviewed the Levine Cancer Institute/Atrium Health prospectively managed radical cystectomy ERAS database, evaluating 260 consecutive radical cystectomy patients under ERAS protocol between January 1, 2017 and March 3, 2021. Intraoperative transversus abdominus plane block was added in April 2018, and narcotic pain medications were utilized as needed. Ketorolac, gabapentin, and acetaminophen compliance were defined as receipt of the non-narcotic as prescribed by protocol: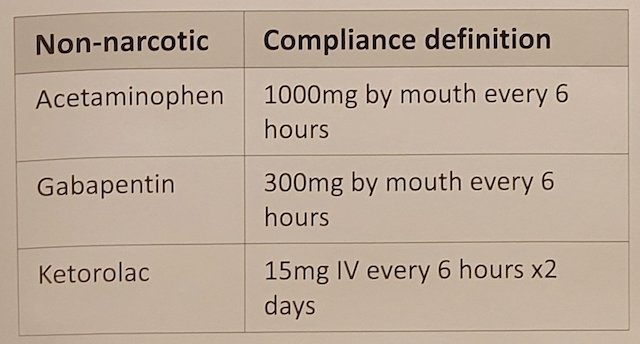
The impact of post-operative non-narcotic totals (as dichotomized variables) on length of stay and time to bowel movement was evaluated with general linear models. Analyses were adjusted for use of transverse abdominus plane block and surgeon.
There was no association between non-narcotic compliance and length of stay across all three non-narcotics (ketorolac p = 0.388; gabapentin p= 0.409; acetaminophen p = 0.409). While there was no association between ketorolac (p = 0.223) or acetaminophen (p = 0.933) compliance and time to bowel movement, gabapentin compliance was associated with shorter time to bowel movement (3.7 days vs 4.3 days; p = 0.009):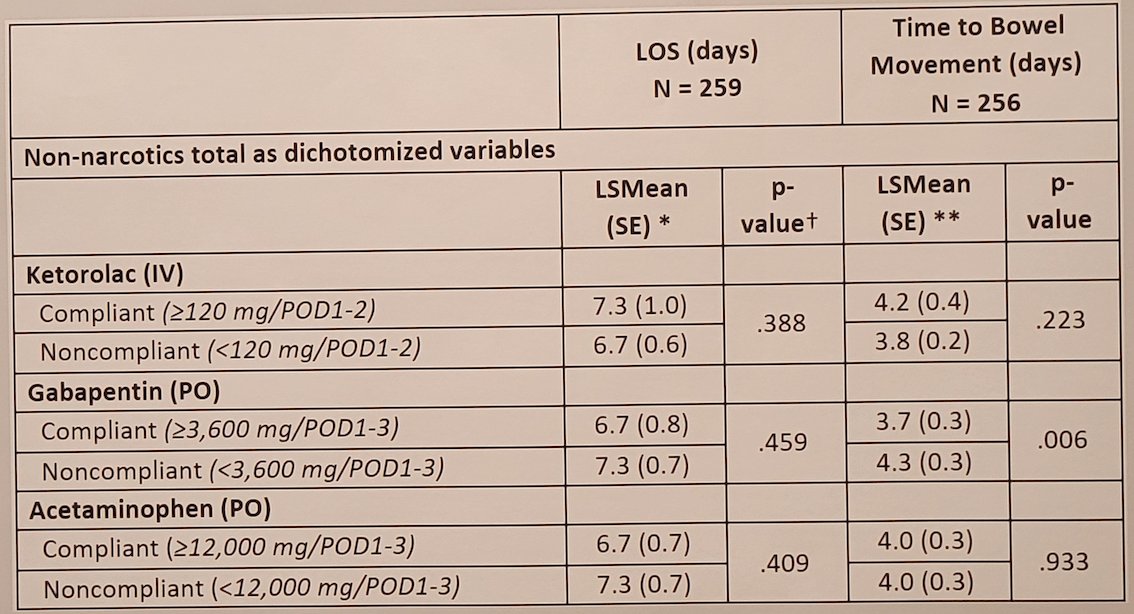
Dr. McGrath concluded her presentation discussing non-narcotic compliance and clinical outcomes in ERAS cystectomy patients with the following conclusions:
- Non-narcotic compliance with ketorolac, gabapentin, or acetaminophen was not associated with length of stay in this ERAS cystectomy cohort
- Compliance with gabapentin was associated with a shorter time to bowel movement
- These results highlight the complex interplay of ERAS protocol elements and further research will continue to illuminate elements which contribute to positive ERAS outcomes
- Additional future aims include developing a risk-adapted approach to non-narcotic analgesia in this ERAS protocol by targeted subtraction of non-narcotic analgesia elements
Presented by: Lila McGrath, Levine Cancer Institute/Atrium Health, Charlotte NC
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Southeastern Section of the American Urological Association (SESAUA) Annual Meeting, Austin, TX, Wed, Mar 20 – Sat, Mar 23, 2024.


