The major new elements that were incorporated into the Pathology chapter were the WHO 2016 grading scheme, the Paris 2015 Cytology discussion, and the Reporting ICCR 2017 recommendations. The WHO 2016 scheme accounted for new staging elements, new histologic subgroups, diverticulum pathology, IHC and molecular IHC. The ICCR (International Collaboration on Cancer Reporting) was an effort from all pathology organizations to create a standardized reporting method so the data is easily translatable – data can be found on www.iccr-cancer.org.
At the end of the day, in this chapter, grading remained the most controversial.
- Distinction between LG Ta and LMP (low malignant potential lesion) is minimal. Does not seme to have much effect on outcomes.
- For Ta and T1 lesions, reverting back to 1973 WHO substratification of HG (WHO 2006). Grade 2 and Grade 3 have been shown to have greater prognostic value that HG alone. Molecular studies recently have confirmed distinct genetic populations with different outcomes.
- T1 subdivision
- Appears to be important for clinical management – but no consensus on method
- Though this is the first time WHO recommended substaging T1, no recommendation on how to report
- ICCR recommends millimiters of invasion, extent of invasion or pT1a/b
- Diverticular tumors
Histology
When it comes to histology, there are numerous subtypes and distinct BCa histologies now. Dr. Konety will talk about some of the variants more later. There have been some changes in the terminology:
- Clear cell added
- Signet ring has been recategorized as a diffuse/plasmacytoid
Concordance of Reporting
She notes that previous studies have demonstrated very high concordance for patients with classic forms of the disease (~90%), but very unimpressive concordance among all histologies (kappa = 0.54)
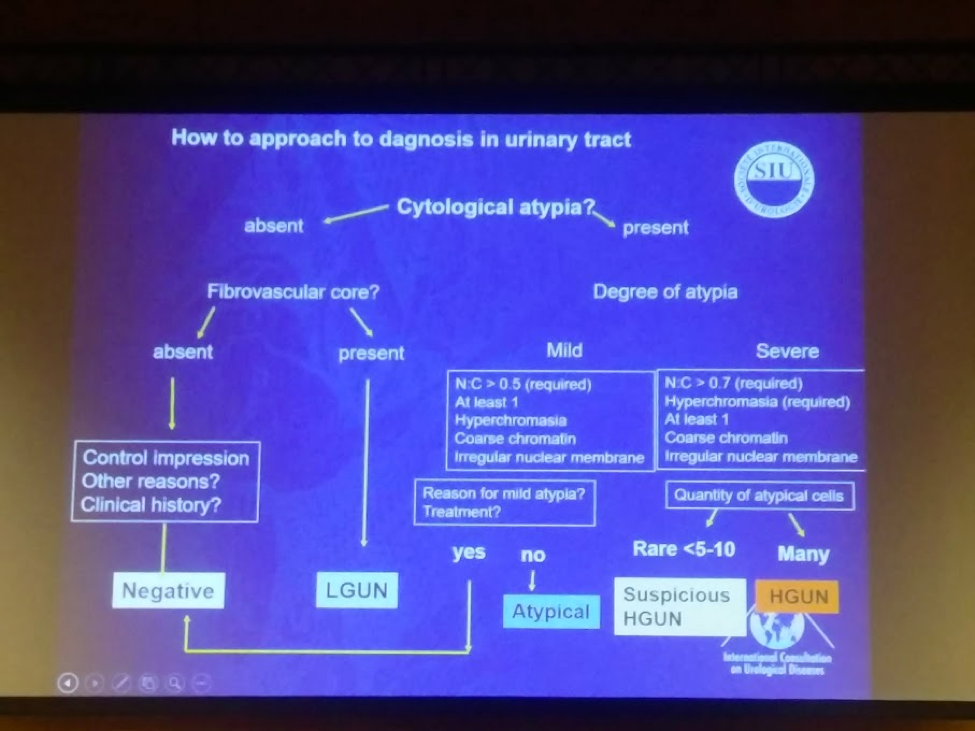
Urine Cytology and the Paris System (2015)
Review of urine cytology terminology and standardization
- Atypical Urothelial cells does not mean cancer!
- A nice flow chart from the Paris system highlights the decision making
- Nuclear:chromatin ratio helps separate atypical from “suspicious for UC”
* E Comparat, SIU 2017.
Reporting on margins
- Margins must be reported as “Cannot be assessed”, “not involved” or “involved”
- However, the chapter will delve into false positives due to stromal changes that may mimic R+ disease
- Soft tissue R+ disease is associated with higher rate of recurrence and lower CSS
- Urethral margins do not seem to carry much clinical value
- Ureteral margins should still be continued
Presented by: Eva Compérat
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 37th Congress of Société Internationale d’Urologie - October 19-22, 2017- Lisbon, Portugal


