
Table 1 – AUA guidelines risk stratification1
Early cystectomy is strongly recommended in patients with BCG unresponsive disease and as initial therapy for patients with the highest risk disease. The rationale behind this therapeutic strategy is due to several reasons. These include the high upstaging risk for T1 HG, the high progression risk for some patients with high-risk disease, and the fact that patients who progress to muscle-invasive bladder cancer (MIBC) have a worse prognosis compared to patients who present de novo.
Dr. Lerner continued and debated what are the indications for early radical cystectomy without first attempting intravesical therapy? According to the AUA guidelines, these are high-risk patients who are fit for surgery, with persistent HG T1 disease on repeat resections, or patients with T1 HG tumors with associated CIS or lymphovascular invasion (LVI), or variant histology (Grade C). According to the EAU guidelines, these are patients with multiple and/or large T1 HG disease, and /or recurrent T1 HG with CIS in the prostatic urethra.
Next, Dr. Lerner elaborated on the indications for early cystectomy for patients who have had intravesical instillations in the past. According to both AUA and EAU guidelines, these are BCG unresponsive patients, which include patients fit for surgery with HG T1 disease after a single course of induction intravesical BCG. Other appropriate patients for early radical cystectomy include patients who are at high risk with persistent or recurrent disease within one year following treatment with two inductions cycles of BCG or BCG maintenance. Additionally, failure to achieve a complete response at three months following BCG induction therapy is an important marker for bad disease, warranting early cystectomy.2 It has also been shown that delaying radical cystectomy, as opposed to early cystectomy, is associated with worse survival (Figure 1).3 As mentioned earlier, concomitant CIS is a predictor for worse cancer-specific survival.3
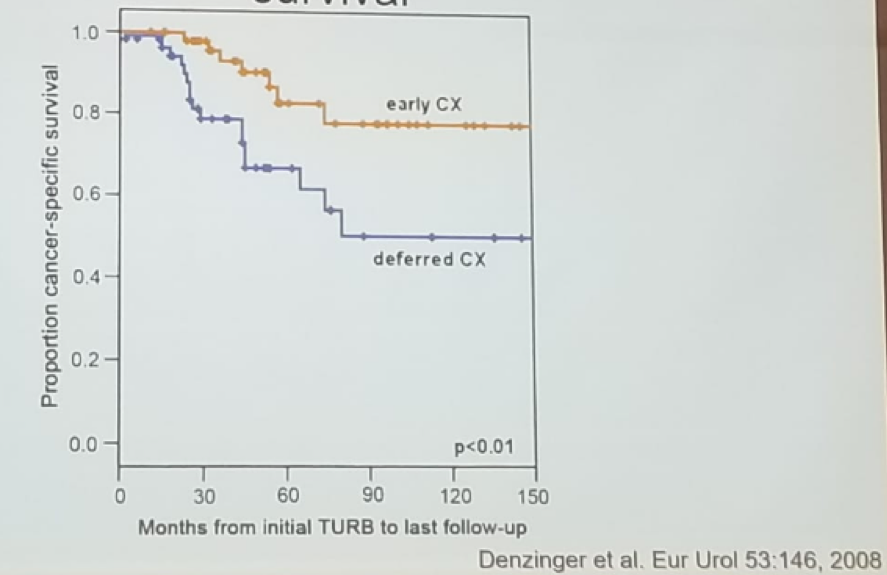
Figure 1 – Delaying cystectomy is associated with worse survival:
The National Comprehensive Cancer Network (NCCN) guidelines also clearly state that for BCG refractory tumor and for HG recurrence after BCG, early radical cystectomy is the most appropriate treatment.
Another important point mentioned by Dr. Lerner is that we should consider extravesical sites of disease in patients who have received BCG therapy, and have failed it due to disease in the prostatic urethra or in the upper tracts.4 In a retrospective analysis of 110 patients with high-risk disease NMIBC treated with BCG without maintenance, it was found that 52% had upper tract or prostatic urethra disease involvement, and 48% had an intravesical recurrence. The prostatic urethra has been found to be the most important predictor of MIBC with a hazard ratio of 12.2 (2.2-65.5), p=0.003. 5 Therefore, sampling of the prostatic urethra near the verumontanum in high-risk patients is essential.
The last topic discussed by Dr. Lerner was variant histology. Due to the high rate of upstaging associated with variant histology, early radical cystectomy should be offered to these patients. Variant histology is associated with high-grade disease and muscle invasion – 86% vs. 53% with pure urothelial carcinoma. The specific histologies that warrant upfront cystectomy include nested, micropapillary, plasmacytoid, and sarcomatoid.
Upfront radical cystectomy can even be offered for patients with Ta low-grade disease when the disease burden is so significant and when it is deemed to be unresectable.
Dr. Lerner summarized his excellent talk stating that initial cystectomy can be offered for patients with an unresectable high burden of Ta low-grade disease, very high-risk T1 HG disease, or with variant histology. BCG failure and unresponsive states result in a substantially high risk for under staging and progression to MIBC. Radical cystectomy has a high probability of long-term cancer control. Lastly, early radical cystectomy for NMIBC does not require administering neoadjuvant chemotherapy.
Presented by: Seth Lerner, MD Baylor College of Medicine, United States
References:
1. Chang S et al. AUA NMIBC GUIDELINES 2016
2. Lerner et al. Urologic Oncology 2007
3. Denzinger et al. Eur Urol 2008
4. Giannarini G et al. Eur Urol 2014
5. Huguet J et al. Eur Urol 2005
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre Twitter: @GoldbergHanan at the 38th Congress of the Society of International Urology - October 4- 7, 2018 - Seoul, South Korea


