Dr. Gontero was the first debater, suggesting therapy with BCG for this patient. There is no doubt that a T1 high-grade disease is considered an aggressive non-muscle invasive bladder cancer (NMIBC). The progression rate of this specific disease is between 27-65%.1 There is a treatment dilemma having to decide between early aggressive radical cystectomy or conservative therapy with BCG.
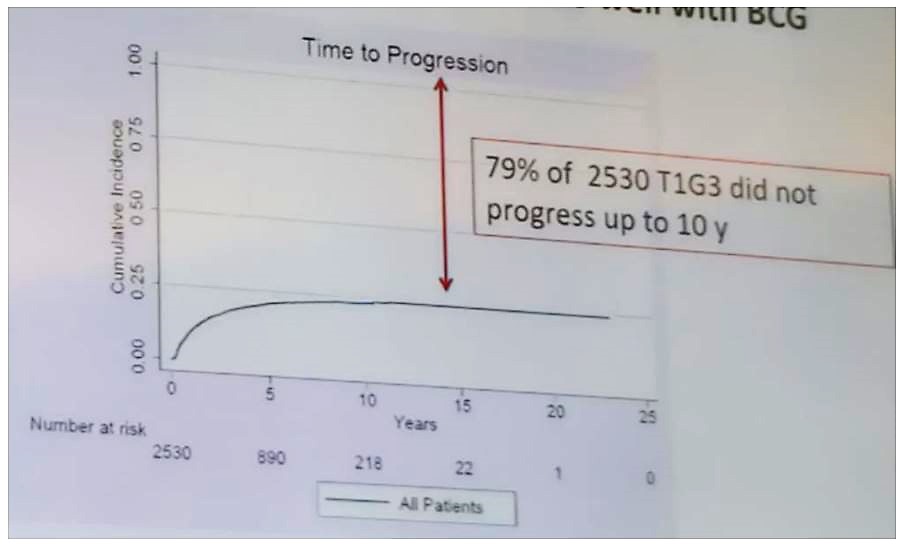
According to Dr. Gontero, most NMIBC tumors at high risk of progression do well with BCG treatment with 79% of 2,530 patients with T1G3 tumors not showing progression in up to 10 years2 (Figure 1). To date, there is no evidence that BCG therapy is inferior to cystectomy in terms of cancer-specific death (CSD). Additionally, radical cystectomy will not cure all T1G3 tumors, with only 20% of such patients being cured by this radical surgery.3
Figure 1 - Most NMIBC tumors at high risk of progression do well with BCG therapy:
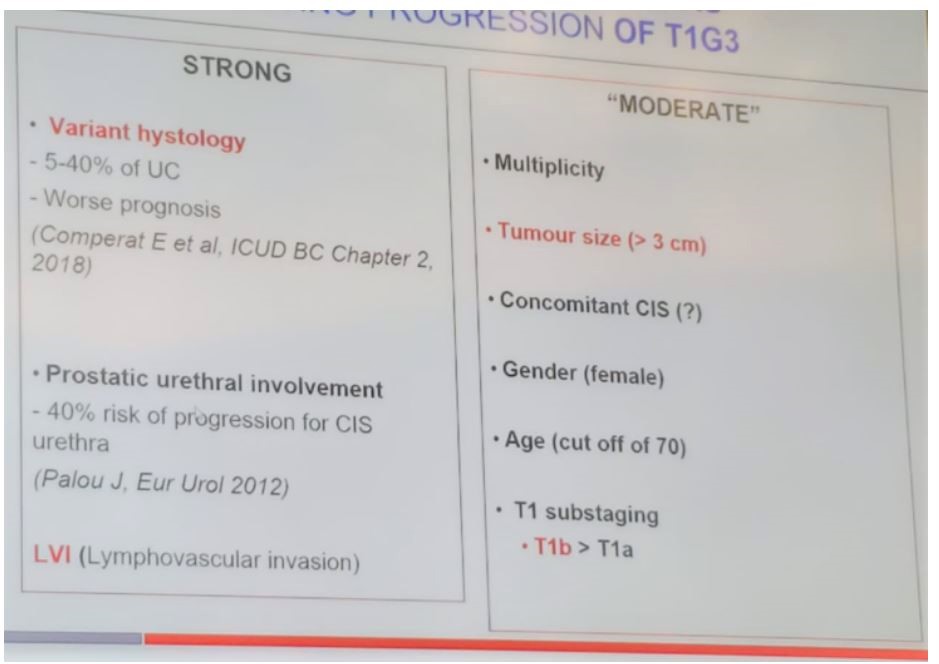
However, if this patient fails BCG therapy, there is evidence showing that delayed radical cystectomy done after BCG failure will show a lower survival advantage. Retrospective series comparing early (before BCG) vs. delayed radical cystectomy (BCG recurrent) in T1G3 tumors have shown a cancer-specific survival advantage in favor of early cystectomy (Figure 2). There are specific clinical prognostic factors affecting the progression rate of T1G3 tumors (Figure 3).
Figure 2- Early cystectomy has a survival advantage when compared to delayed cystectomy (after BCG failure) in T1G3 tumors:
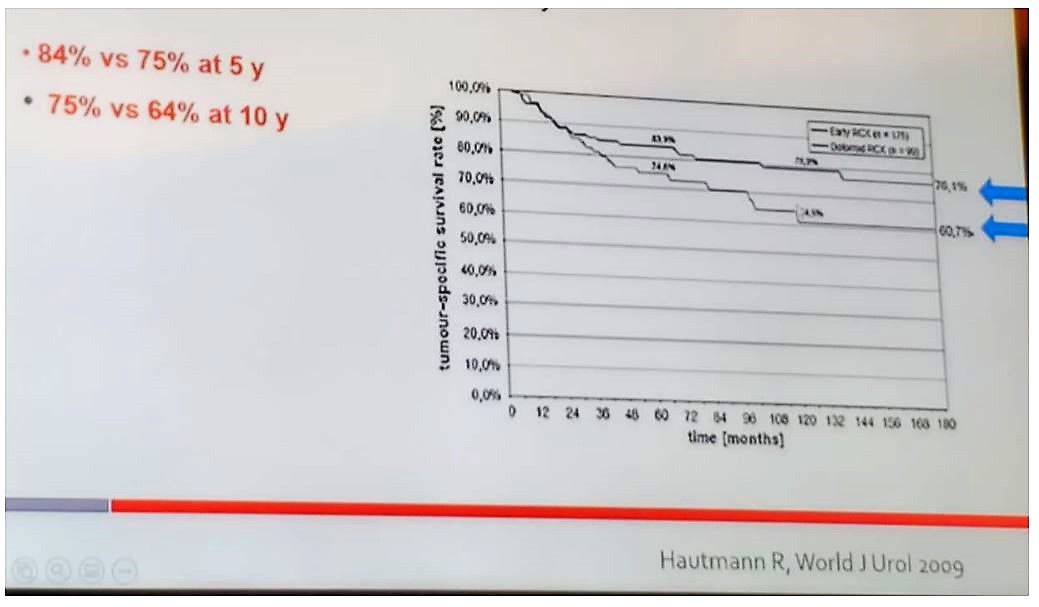
Figure 3 – Clinical prognostic factors affecting the progression of T1G3 tumors:
Next, the question of whether variant histology is a contraindication to BCG was raised. In a small multicenter retrospective study assessing 47 patients with variant histology, BCG was associated with improved cancer-specific survival.4
In the particular case presented, Dr. Gontero suggested hat the first step should be to perform a re-TUR as the risk of downstaging is quite high.5 The pathology derived at re-TUR may affect the treatment decision.6
NMIBC and muscle-invasive bladder cancer (MIBC) have different genetic signatures. One study aimed to find a unifying subtype category and identify aggressive NMIBC. Some of the T1G3 are more aggressive and we need to be able to identify them. Approximately 20% of NMIBC have a muscle-invasive molecular signature.7
Dr. Gontero concluded his talk stating that to date there is no evidence to convince this patient with T1G3 that BCG is inferior to radical cystectomy. Currently, there is a shortage of reliable markers and /or risk tables to help us predict at an individual basis the patient’s risk to progress to MIBC. Hopefully, in the near future, genomic signatures will perhaps help in the treatment decision.
Presented by: Dr. Paolo Gontero, Chairmen of the Division of Urology, San Giovanni Battista Hospital (Molinette), and Associate Professor of Urology at the University of Studies of Torino, Italy
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
1. Nieder AM, Brausi M, Lamm D, et al. Management of stage T1 tumors of the bladder: International Consensus Panel. Urology 2005; 66(6 Suppl 1): 108-25.
2. Gontero P, Sylvester R, Pisano F, et al. Prognostic factors and risk groups in T1G3 non-muscle-invasive bladder cancer patients initially treated with Bacillus Calmette-Guerin: results of a retrospective multicenter study of 2451 patients. Eur Urol 2015; 67(1): 74-82.
3. Stein JP, Lieskovsky G, Cote R, et al. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2001; 19(3): 666-75.
4. Yorozuya W, Nishiyama N, Shindo T, et al. Bacillus Calmette-Guerin may have clinical benefit for glandular or squamous differentiation in non-muscle invasive bladder cancer patients: retrospective multicenter study. Japanese journal of clinical oncology 2018; 48(7): 661-6.
5. Naselli A, Hurle R, Paparella S, et al. Role of Restaging Transurethral Resection for T1 Non–muscle invasive Bladder Cancer: A Systematic Review and Meta-analysis. European Urology Focus 2018; 4(4): 558-67.
6. Soria F, Pisano F, Gontero P, et al. Predictors of oncological outcomes in T1G3 patients treated with BCG who undergo radical cystectomy. World journal of urology 2018; 36(11): 1775-81.
7. Tan TZ, Rouanne M, Tan KT, Huang RY-J, Thiery J-P. Molecular Subtypes of Urothelial Bladder Cancer: Results from a Meta-cohort Analysis of 2411 Tumors. European Urology 2019; 75(3): 423-32.


