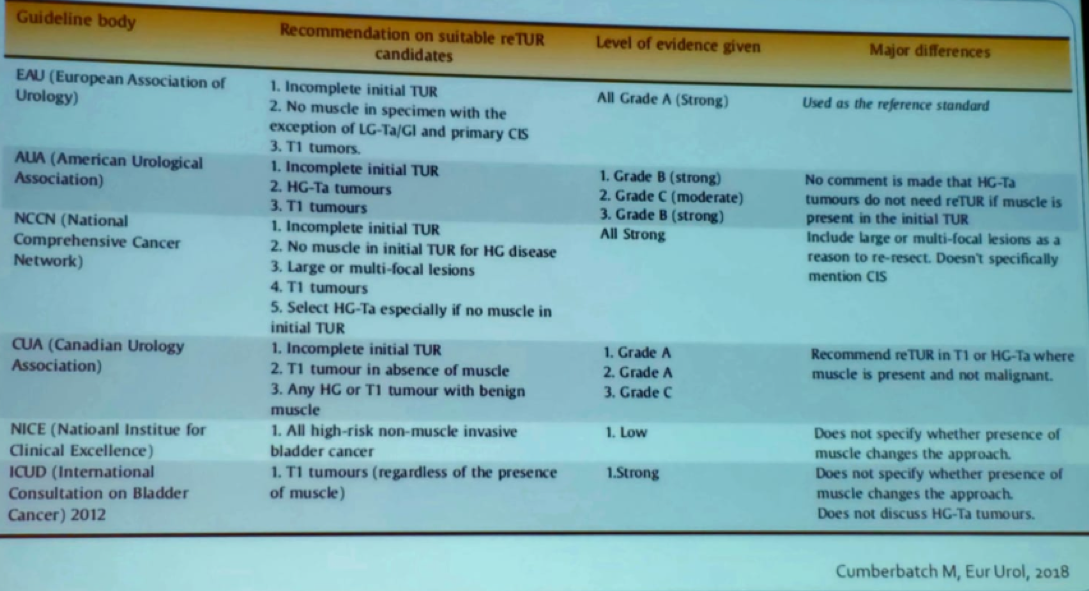
There has bee some discussion in the past regarding the need to perform another TURBT after the initial one, which is called the restaging TURBT (re-TURBT). Table 1 demonstrates the current recommendation by the various large specific guidelines.
Table 1 – Recommendations regarding restaging TURBT:
Dr. Kamat mentioned the scenarios where it is mandatory to perform re-TURBT and no debate has been reported:
1. When the first resection was incomplete
2. Following an office biopsy
3. Aborted procedure
4. When there is clinical suspicion of a worse disease than had originally been reported by the pathologist
Next, Dr. Kamat raised the question of whether we are overindulging in re-TURBT. In a large systematic review of over 8000 patients with high-grade Ta and T1, detrusor muscle was found at initial TURBT in 30-100% of cases. Most residual tumors (36-86%) were found at the original resection site1. However, when stratifying the recurrence rate by whether the patients had a repeat TURBT, the difference was significant with 58% vs.16% recurrence rate in favor of those who had a repeat TURBT1. The disease-free survival was also better for those who had a resection (83% cs. 69%)1.
When assessing the rates of upstaging to T2 disease, the variance was quite significant (22-32%)1. This urologic procedure is the most under-appreciated and under-taught in urologic clinics. In this procedure. Dr. Kamat stated the importance of the various methods to increase the diagnosis rate in cystoscopy and eventually re-TRUBT, such as narrow-band imaging, and blue-light cystoscopy (Figure 1).
Figure 1 - Recommended enhanced imaging in cystoscopy:

The next topic discussed was the development of BCG-unresponsive non-muscle invasive bladder cancer. BCG unresponsive can be defined as:
1. Persistent or recurrent carcinoma in situ (CIS) – within 12 months of completion of adequate BCG therapy
2. Recurrent high grade and Ta1 disease – within 6 months of BCG induction
3. Persistent or new T1 high-grade disease - at first evaluating (3 months) following induction BCG
For all these patients, repeat TURBT is mandatory. Repeat TURBT has been shown to lower the time to recurrence.2 The impact of re-TURBT on outcomes has shown that these patients undergo radical treatment and have increased survival 3 months after achieving histologically identified muscle invasions.
The MD Anderson cancer center algorithm for advanced prostate cancer is shown in Figure 2.
Figure 2 – MD Anderson cancer center algorithm for the management of bladder cancer.
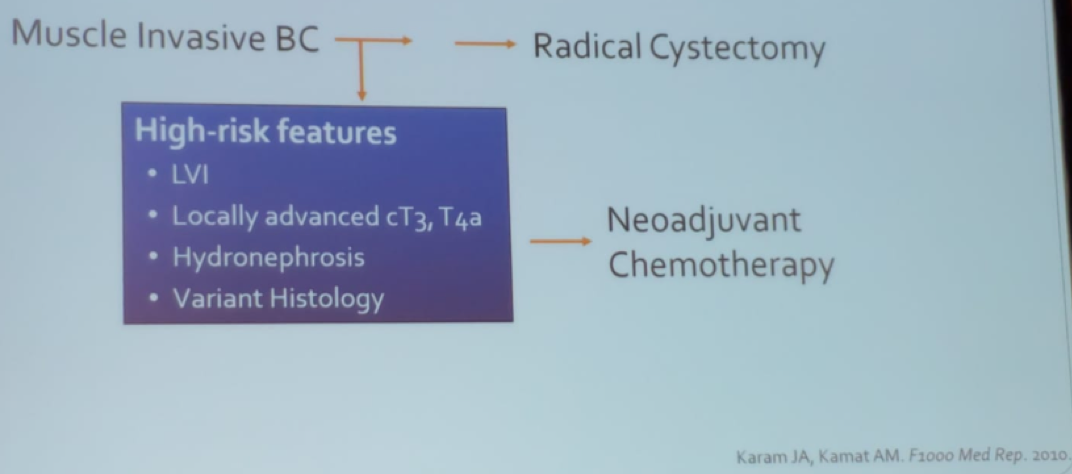
Pathological stage T0 at radical cystectomy for bladder cancer has been shown to be associated with improved outcomes independent of traditional clinical risk factors3.
In summarizing his talk, Dr. Kamat mentioned performing repeat TURBT will be required if the following parameters are seen:
- Ta high-grade tumor – only if suspicions of incomplete resection or enrolled to the wrong clinical trial
- T1 low-grade tumors – because they are rare enough, so it is better to examine again if nothing was missed
- T1 high-grade tumors
- T2 tumors
Presented by: Ashish Kamat, MD, MBBS, Professor of Urology, Director of Urologic Oncology Fellowship, MD Anderson Cancer Center, University of Texas, Houston, Texas
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
1. Cumberbatch MGK, Foerster B, Catto JWF, et al. Repeat Transurethral Resection in Non-muscle-invasive Bladder Cancer: A Systematic Review. Eur Urol 2018; 73(6): 925-33.
2. Sfakianos JP, Kim PH, Hakimi AA, Herr HW. The effect of restaging transurethral resection on recurrence and progression rates in patients with nonmuscle invasive bladder cancer treated with intravesical bacillus Calmette-Guerin. The Journal of urology 2014; 191(2): 341-5.
3. Kassouf W, Spiess PE, Brown GA, et al. P0 stage at radical cystectomy for bladder cancer is associated with improved outcome independent of traditional clinical risk factors. European urology 2007; 52(3): 769-74.


