Athens, Greece (Urotoday.com) Dr. Renu Eapen gave a talk on the imaging options of patients with biochemical recurrence (BCR) after radical prostatectomy. BCR is generally defined as a detectable PSA level of 0.2 ng/ml or higher after radical prostatectomy (according to the AUA and EAU guidelines). There are many variables related to and affecting BCR.
These include:
- Gleason score
- Pathological stage
- Surgical margin
- Lymph node status
- PSA doubling time (PSADT)
When facing a scenario of rising PSA after local definitive therapy, there are several necessary steps that need to be taken, according to Dr. Eapen. Firstly, PSA needs to be monitored on a regular basis. If the PSA continues to increase from the posttreatment nadir, this most probably indicates persistent cancer and high risk for metastases. If the prostatectomy reveals high risk features, early radiotherapy needs to be considered and the addition of androgen deprivation therapy (ADT) is suggested if nodal disease is found.
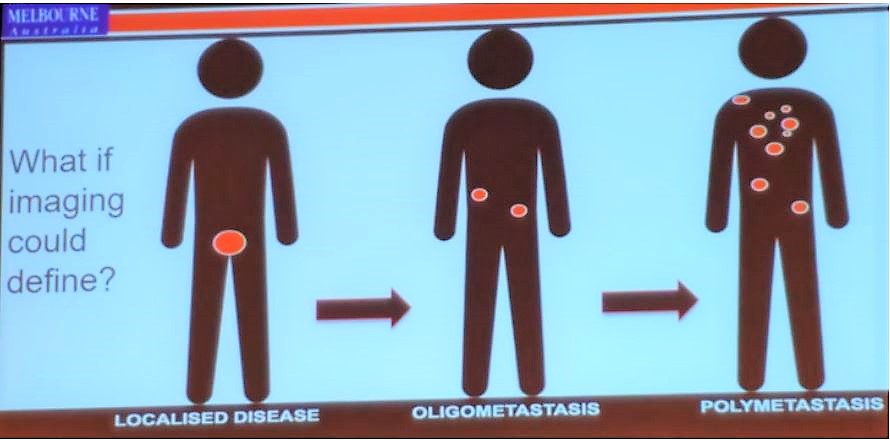
In this scenario of rising PSA after radical prostatectomy, imaging should ideally help us delineate whether the disease recurrence is localized, whether it is oligometastatic or polymetastatic (Figure 1).
Figure 1 – What should imaging help us define when the PSA rises after radical prostatectomy?
The introduction of PSMA PET imaging has significantly changed our perspective of imaging, and therefore this is the recommended imaging modality in this setting (choline PET is also an option, but it is not as good as PSMA1). We now have the understanding that conventional imaging at these low PSA levels is quite useless.1
There is minimal data regarding the use of multiparametric MRI (mpMRI) in this scenario, but this is most likely not as good as PET PSMA. mpMRI can only detect some recurrences at a PSA of 1.0-2.0 ng/ml, with diffusion-weighted imaging showing the best results.2 This is clearly not good enough, as the PSA levels are significantly lower at the initial phase of BCR.
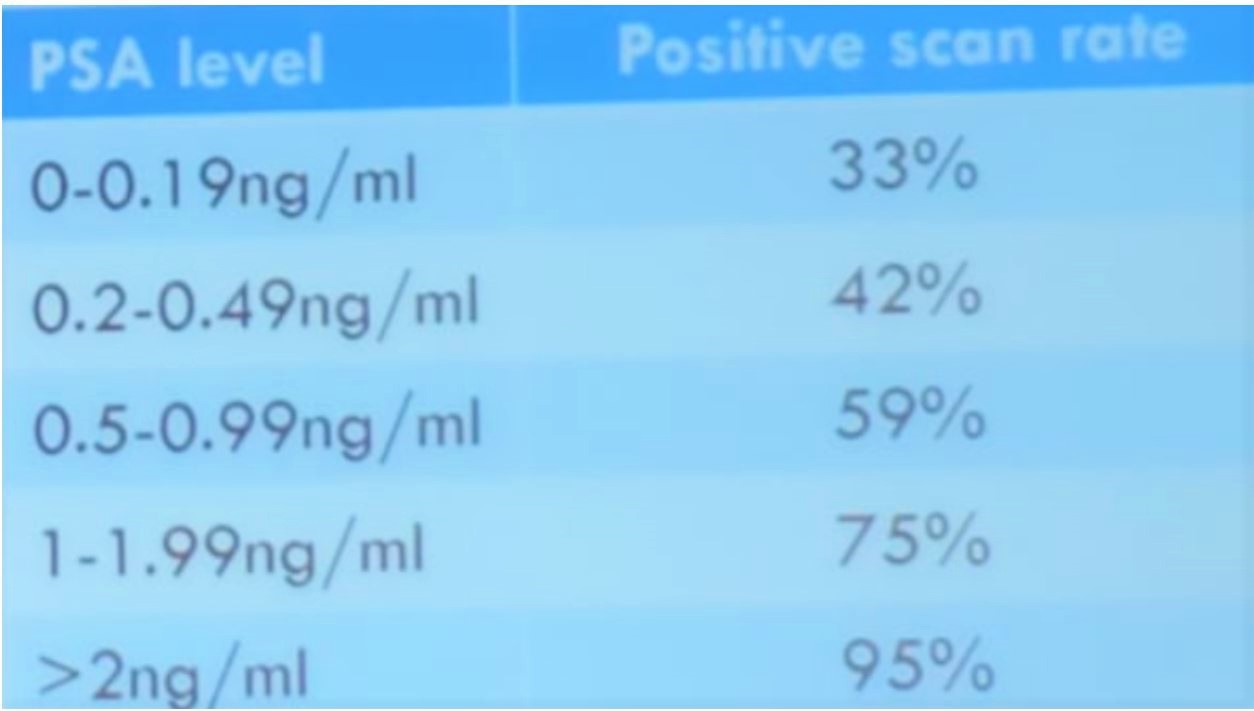
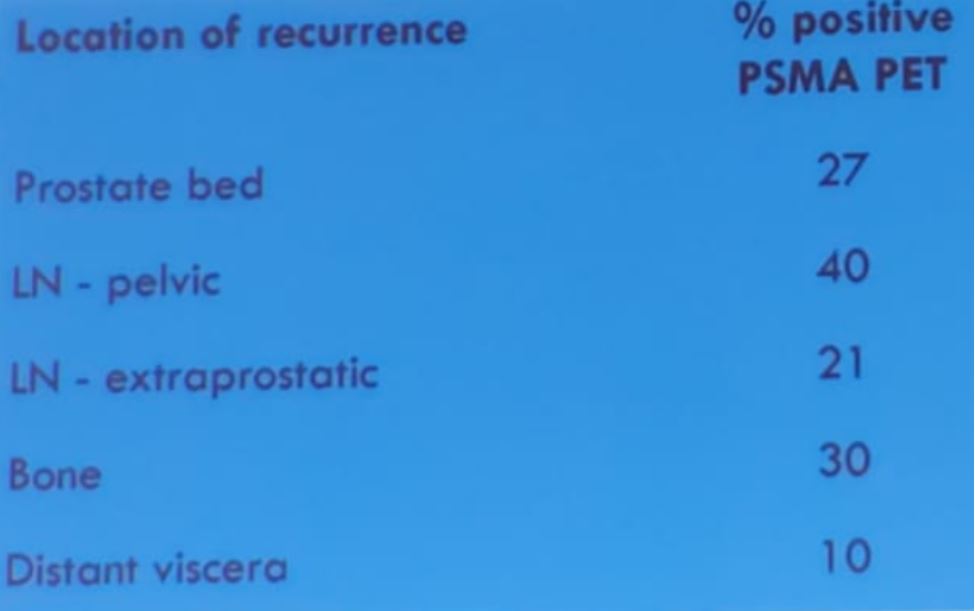
PET PSMA has a high sensitivity even at low PSA values, and a specificity of over 95%3, with an increasing positive scan rate, which is in accordance with rising PSA levels (Table 1). The location of recurrence also varies regarding the % of positive PET PSMA scans (Table 2). There is also a correlation between PSADT and the rate of positive PET PSMA scans. Long PSADT (> 6 months) correlates to a 64% positive PET PSMA, and short PSADT (<=6 months) correlates to a 92% positive PET PSMA.
Table 1 – Positive scan rate of PET PSMA in various rising PSA levels after radical prostatectomy
Table 2 – Percent of positive PET PSMA scans with regards to the location of recurrence after radical prostatectomy
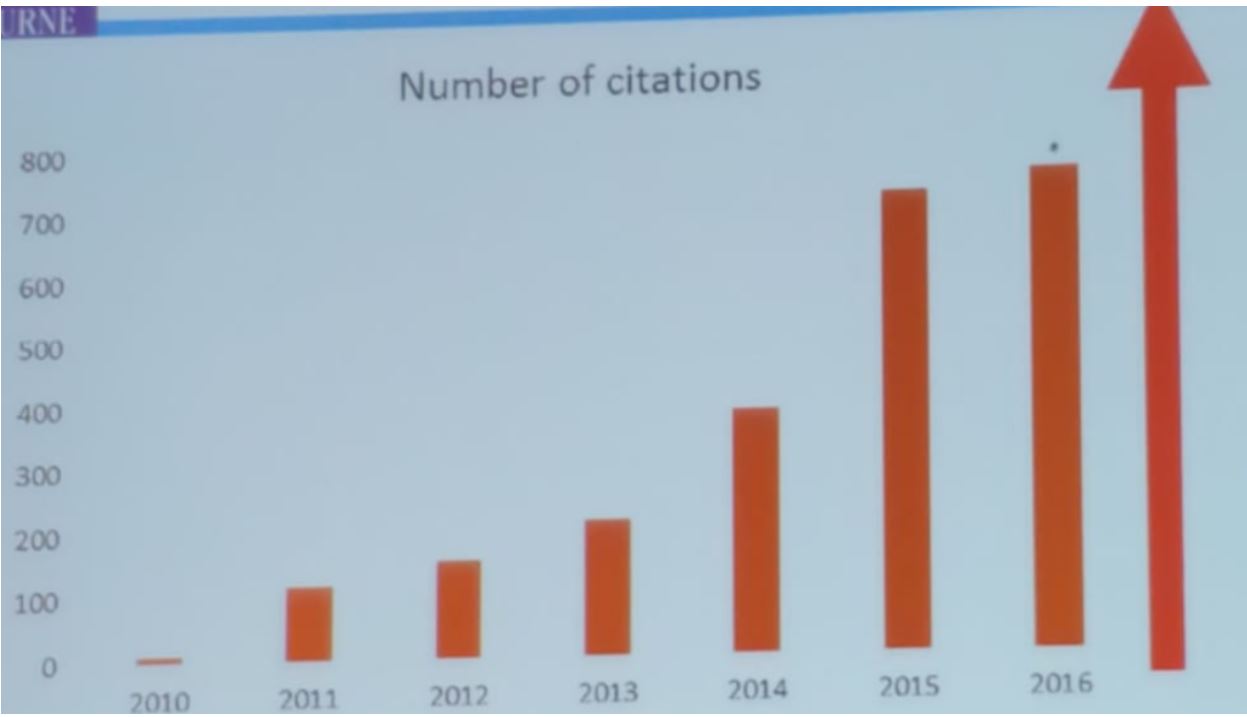
Due to its superior attributes, compared to conventional imaging, the number of studies involving PET PSMA has risen significantly through the years with an increasing number of citations as can be seen in figure 2.
Figure 2 – Number of citations mentioning PSMA PET through the years:
Dr. Eapen concluded her talk with some important take-home messages.
- PSA and associated PSA kinetics can predict the risk of metastatic disease diagnosed by PET PSMA, which has superior sensitivity and specificity, compared to conventional imaging modalities.
- Therefore, PSMA PET improves detection of metastases with BCR.
- The accuracy of PET PSMA rises in accordance to rising PSA levels. The “sweet spot” to order PET PSMA is when the PSA is between 0.2-0.5 ng/ml (45% positive PSMA PET scan rate).
- Most importantly, there is still a great need for more data regarding the use of this imaging modality.
Presented by: Dr. Renu Eapen, Consultant Urologist in the Genitourinary Oncology, Peter MacCallum Cancer Center, Melbourne, Australia
Written By: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New-York, US @GoldbergHanan at the 39th Congress of the Société Internationale d'Urologie, SIU 2019, #SIUWorld #SIU2019, October 17-20, 2019, Athens, Greece
References:
1. Sandgren K, Westerlinck P, Jonsson JH, et al. Imaging for the Detection of Locoregional Recurrences in Biochemical Progression After Radical Prostatectomy—A Systematic Review. European Urology Focus 2019; 5(4): 550-60.
2. Buergy D, Sertdemir M, Weidner A, et al. Detection of Local Recurrence with 3-Tesla MRI After Radical Prostatectomy: A Useful Method for Radiation Treatment Planning? In vivo (Athens, Greece) 2018; 32(1): 125-31.
3. Perera M, Papa N, Roberts M, et al. Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer-Updated Diagnostic Utility, Sensitivity, Specificity, and Distribution of Prostate-specific Membrane Antigen-avid Lesions: A Systematic Review and Meta-analysis. Eur Urol 2019.