Thus, ureteroscopy offers distinct advantages in the management of upper tract urothelial carcinoma. First, there is an increased sensitivity for the detection of disease, particularly when used in a complementary fashion with CTU. Further, histopathology from ureteroscopic biopsies can guide decision making. High-grade histology is strongly correlated with invasive stage and may be useful to guide management. However, it is important to note that undergrading is not uncommon. Further, for patients in who nephron-sparing approaches are being electively considered, histologic exclusion of high-grade disease is critical.
The use of ureteroscopy may allow for expanded indications for nephron-sparing surgery, particularly given the size cut-offs in current guidelines that Dr. Gontero deemed “arbitrary”. Thus, even larger low-grade tumors may be considered for endoscopic treatment.
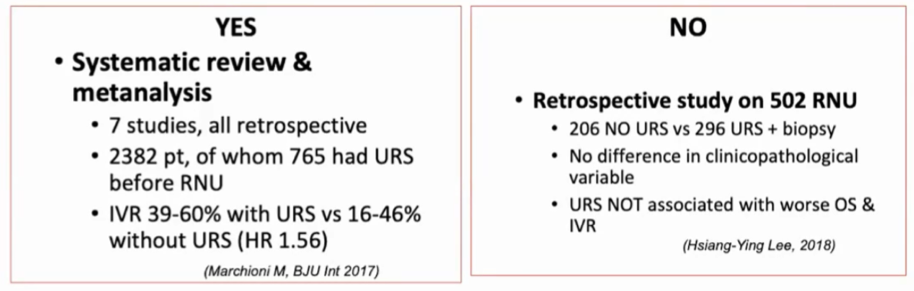
However, there are notable limitations. First, there is an inherent inaccuracy of biopsy staging. While histologic grading is relatively accurate, staging is less so, in part driven by suboptimal harvesting of good quality tissue. As a result, lamina propria is often absent. Additionally, there are theoretical risks as a result of high intra-renal pressures including forniceal rupture and “through mucosa seeding” though reported cases of these have not been documented. Finally, there is a somewhat debatable increased risk of intravesical recurrence associated with ureteroscopy prior to nephroureterectomy. Dr. Gontero highlighted that a systematic review of 7 retrospective studies demonstrated an increased risk of bladder recurrence and suggested that intravesical chemotherapeutic instillation may obviate that risk.
Dr. Gontero highlighted that there is an increasing need for nephron-sparing approaches and that technological advances will likely assist with endoscopic diagnosis and management, including improvements in biopsy devices and approaches, use of in situ diagnosis utilizing confocal laser endomicroscopy, and advances in ablation approaches with evolving laser technologies.
He concluded that the use of ureteroscopy can complement diagnostic gaps in CTU and provide tumor grading which can assist with treatment decision making. Thus, he advocated that it be adopted any time there is uncertainty about the diagnosis of high-risk upper tract urothelial carcinoma on the basis of non-invasive testing methods.
Presented by: Paolo Gontero, MD, Professor of Urology. Chairman Department of Urology, Molinette Hospital, University School of Medicine, Torino, Italy
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center Twitter: @WallisCJD at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020


