-Patient 1: young with excellent performance status, Memorial Sloan Kettering Cancer Center (MSKCC) intermediate-risk disease with a large (16cm) right renal mass, and a small lung nodule.
-Patient 2: elderly with ECOG1 performance status, MSKCC poor-risk disease, a 9cm renal mass, and multiple metastases in the lung, liver, and bone.
-Patient 3: middle-aged, ECOG1 performance status, MSKCC intermediate-risk disease with a 9cm renal mass, a 1cm lung metastasis, and a 2cm lymph node metastasis.
Dr. Karam concluded that most would agree that patient 1 may benefit from cytoreductive nephrectomy and that patient 2 should not. Patient 3 presents potentially more commonly and is the more difficult scenario for clinical decision making.
Dr. Karam began by highlighting old data on cytoreductive nephrectomy from the “previous immunotherapy era” with cytokine therapy (interferon +/- surgery) from SWOG 8949 and EORTC 30947 with pooled results favoring the combination approach with differences in median survival of approximately 6 months. Retrospective data from the University of California, Los Angeles UCLA further suggested an even larger benefit for those treated with interleukin-2 instead of interferon.
However, in the targeted therapy era, data differs somewhat. Consistent retrospective data suggested a benefit to cytoreductive among patients receiving these targeted therapies, with this restricted to patients with a Karnofsky performance status of 80 of greater. This was confirmed in multiple analyses using a variety of institutional and population-based datasets. However, the randomized data failed to confirm these findings. The SURTIME trial examining upfront surgery followed by sunitinib or sunitinib followed by delayed surgery demonstrated no difference in progression-free survival. The CARMENA trial, similar in design to the previous SWOG and EORTC trials, assessed sunitinib alone versus nephrectomy followed by sunitinib and found no difference in overall or progression-free survival. However, Dr. Karam highlighted issues with extrapolating data from CARMENA including the high proportion of patients with poor-risk disease, the high tumor bulk in enrolled patients, significant cross-over, and the prolonged and difficult accrual suggesting many patients who were not enrolled.
He then examined the overall survival data from SURTIME which found a longer overall survival for those undergoing delayed nephrectomy, suggesting that this approach can select outpatients with inherent resistance to systemic therapy. A post-hoc analysis of CARMENA similarly suggested that overall survival is long in patients undergoing secondary nephrectomy following initial sunitinib supporting this approach. Further, patients with only one IMDC risk factor may benefit from cytoreduction.
Dr. Karam highlighted the importance of considering selection bias in retrospective studies. While academically, this may be considered a “curse” for causal inference, from a clinically approach, this is a “blessing” highlighting appropriate patient selection. To this end, he sought to examine ways in which we can select patients for cytoreductive nephrectomy including preoperative factors, response to presurgical systemic therapy, and mutational studies.

Addressing these in sequence, he highlighted data looking at laboratory and clinical data which may allow risk stratification of patients. Patients with 3 or fewer risk factors may benefit while those with more do poorly.
A more recent update found similar factors to be prognostic. These have subsequently been included in a variety of nomograms. A number of other studies have identified patient age, tumor burden, T-stage, hospital factors and non-clear cell histology may be associated with better outcomes following cytoreductive nephrectomy.
Examining the response to pre-surgical therapy as a “litmus test”, there are a number of studies that demonstrate that patients who have progressive disease or worsening performance status following initial systemic therapy do poorly and thus should not be treated surgically. A recent pooled analysis from prospective series at 4 different European centers demonstrated that patients undergoing pre-surgical therapy have improved outcomes compared to those undergoing upfront cytoreductive nephrectomy. Further, data from Dr. Abel suggested that a primary tumor response of 10% or greater in the first 2 months of systemic therapy was associated with improved overall survival.
Finally, Dr. Karam highlighted preliminary data regarding the use of mutational studies to identify patients most likely to benefit from surgery. However, these are not yet ready for clinical use.
Dr. Karam then transitioned to discussing the role of cytoreductive nephrectomy in the “new immunotherapy era” with the utilization of checkpoint inhibitors in systemic therapy. While these approaches have demonstrated benefit as systemic therapy approaches, the role of cytoreductive nephrectomy in patients receiving these therapies is unclear. He highlighted some early data from NCT02210117 which randomized patients to a variety of systemic therapies followed by surgery.
He then proposed a new trial which seeks to address two questions: first, can we pick the patients who will do poorly regardless of surgery in order to avoid operating on them and, second, among those who are not expected to do poorly, does surgery provide a survival benefit? The schema for such a study follows.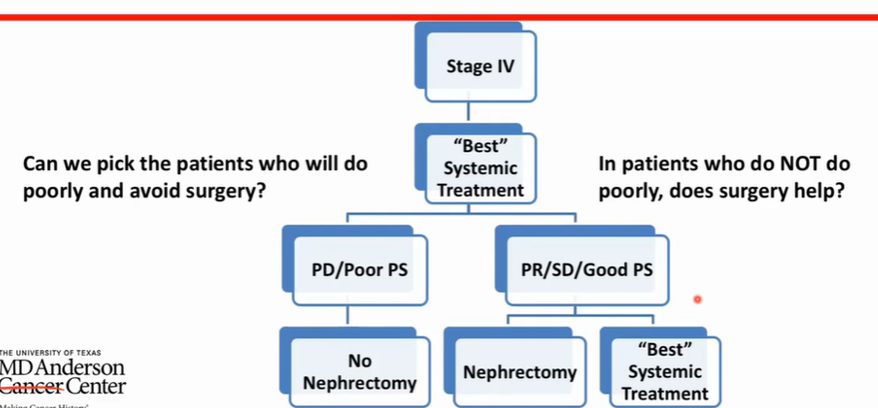
As a take-home message, Dr. Karam highlighted that when considering the role of cytoreductive nephrectomy, the selection is key as it may be associated with long survival in well-selected patients and that factors including preoperative characteristics, preoperative therapy as a litmus test, and molecular analysis may be useful in patients who are being considered for surgery. Outside of clinical trials, he suggested that cytoreductive nephrectomy could be considered in younger patients with clear cell histology, good performance status, limited metastatic burden, 3 or fewer MDACC or IMDC risk factors who respond to presurgical therapy and preferably at high-volume centers.
Presented by: Jose Karam, MD, FACS, Associate Professor in the Department of Urology and Department of Translational Molecular Pathology at The University of Texas MD Anderson Cancer Center in Houston, Texas
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Contact: @WallisCJD on Twitter at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020Read the Opposing Argument: SIU Virtual Congress 2020: Debate: Is There Still a Role for Cytoreductive Nephrectomy in the Management of Kidney Cancer? Against


