Dr. Seth began by highlighting data from Globocan demonstrating that kidney cancer contributes nearly 400,000 new diagnoses and 175,000 deaths worldwide. With variation between countries, 40-80% of all newly diagnosed renal tumors present as small renal masses with the vast majority detected incidentally. These have a significant variation in clinical behavior of other disease characteristics leading to difficulties in management.
One of the key challenges Dr. Seth identified is that precise diagnosis is difficult, particularly as it relates to the key issue of differentiating benign from malignant lesions. Dr. Seth highlighted that small renal masses are defined as those less than 4 cm (T1a) and that metastases at presentation are rare among those with tumors < 3cm at presentation and, in patients with von Hippel Lindau, that metastases are rare on longitudinal follow-up when the largest tumor is < 3cm. Historically, renal adenomas were defined as those < 3cm.
Dr. Seth then discussed a few important benign lesions which may present as small renal masses, beginning with oncocytoma. This is the most common benign small renal mass. While there are characteristic CT features, Dr. Seth emphasized that none are sufficiently specific to distinguish oncocytoma from renal cell carcinoma (RCC). In terms of biopsy, features overlap with chromophobe RCC thus, immunohistochemistry is required to distinguish the two. Angiomyolipomas, in contrast, have diagnostic CT characteristics in the vast majority, save for approximately 5% who have lipid poor lesions. Indeed, these fat poor AMLs are difficult to distinguish from RCCs though MRI texture analysis may be helpful. Cystic nephroma and mixed epithelial-stromal are other, biologically, related benign tumors. Radiographically these present as Bosniak III cysts with grossly thickened walls or septa.
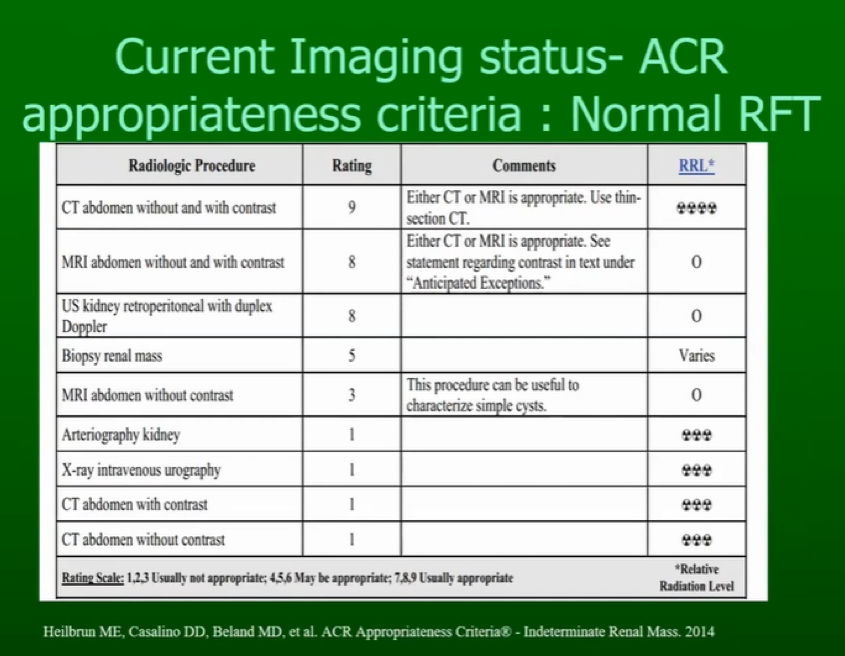
Imaging is clearly important in the evaluation of small renal masses. Among patients with normal renal function, a variety of imaging approaches may be useful. CT with and without contrast is deemed the most appropriate imaging approach.
Among patients with impaired renal function, renal ultrasonography with duplex Doppler is recommended as the preferred approach.
Dr. Seth suggested that emerging imaging approaches may be useful where there is uncertainty following standard renal mass protocol CT, using dual-energy CT, contrast-enhanced ultrasound, diffusion-weighted magnetic resonance imaging, and PET/CT.
Dual-energy CT is an approach in which subtraction approaches are used to generate iodine maps which can measure the iodine concentration of a lesion, addressing the issue of pseudo-enhancement and allowing characterization of renal cysts. In a pooled meta-analysis of 5 studies, DE-CT had a pooled sensitivity of 96.6% (95% confidence interval 85.9 to 99.3%) and specificity of 95.1% (95% confidence interval 90.7 to 97.5%) to distinguish benign and malignant lesions.
Contrast-enhanced ultrasound can be employed in patients with impaired renal function. The contrast agent has a phospholipid shell with sulfur hexafluoride gas contained within. This has a similar size and shape as a red blood cell, allowing assessment of vascularity. As with DE-CT, this approach is helpful to assess potential renal cysts.
Magnetic resonance imaging may be used with or without contrast and has demonstrated sensitivity and specificity that is equivalent to or better than contrast-enhanced CT. Recent data has suggested that multiparametric MRI with diffusion weighting improves the diagnostic characteristics of MRI including giving data on the histological subtype of solid renal masses.
Radionucleotide studies may also be helpful to characterize renal masses. First, Iodine-124 labeled girentuximab, an antibody to CA-IX, may be used as a PET-CT tracer. For the identification of clear cell RCC, this PET/CT approach had higher sensitivity and specificity than standard contrast-enhanced CT. Second, 99mTc-Sestamibi SPECT/CT can be used to distinguish oncocytoma and hybrid oncocytic/chromophobe lesions from other renal masses with high sensitivity (88%) and specificity (95%).
Dr. Seth then transitioned to the topic of renal mass biopsy. A systematic review has emphasized that core biopsy has significantly better sensitivity, specificity, and ability to distinguish tumor subtype and grade compared to aspiration cytology. This is a safe approach that uncommon low-grade complications and no documented cases of tumor seeding. The issue with this approach is that of non-diagnostic biopsy with rates ranging from 0 to 47%, and a pooled rate of 8% on systematic review. Cystic lesions, smaller tumors, and greater skin to tumor distance predicted non-diagnostic biopsy results. Tumor heterogeneity is cited as a reason for grade discordance between biopsy and final pathology. Thus, Dr. Seth concluded that the clinical utility of biopsy remains a matter of debate and some patients may be able to undergo surveillance regardless of histologic results and thus may be spared biopsy.
Moving from diagnostic to therapeutic strategies, Dr. Seth discussed active surveillance, in which an initial period of observation allows assessment of tumor growth kinetics and can thus allow the selection of patients for continued observation or intervention. Patient selection is key for successful active surveillance, with previous reports including elderly and comorbid patients. Further, smaller tumors were much more likely to be benign (with a 17% increase in malignant risk for every 1cm of tumor size) and much less likely to be associated with metastases. Among available series, growth rates (at ~0.25cm/yr), progression to metastasis (0-5%), and kidney cancer-related death were all low.
For those opting for treatment, Dr. Seth considered the treatment comparison between partial nephrectomy and ablation. Most guidelines to date recommend ablation in patients with small masses, with many specifying that this should be restricted to selected individuals who are elderly and with competing health risks though others suggesting that this approach is suitable for all patients. Ablation may be achieved through a variety of technical approaches. The best available data are for cryoablation and radio-frequency ablation. There are no prospective data comparing these ablation approaches to partial nephrectomy but two initial small retrospective studies suggest similar overall, cancer-specific, recurrence-free, and metastasis-free survival while a larger recent study suggests higher local recurrence rates for those undergoing ablation.
Presented by: Amlesh Seth, MBBS, MS, M.ch, Professor, Department of Urology, All India Institute Of Medical Sciences, India.
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center Contact: @WallisCJD on Twitter at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020


