Dr. Eapen highlights that it is critical for therapeutic decision making to define the extent of disease. One in four patients have high-risk prostate cancer and more than 80% of these patients have curative intent treatment, including 56% of patients having surgery while most very high-risk patients have radiotherapy. Conventional imaging (CT, bone scan) is insufficient to detect non-localized disease with sub-optimal sensitivity and specificity, whereas more accurate imaging allows tailored multimodal treatment planning and may improve outcomes.
Dr. Eapen notes that the prostate-specific membrane antigen (PSMA) PET-CT scan is becoming a challenger to conventional imaging, highlighting that we now have a randomized control trial to support PSMA PET-CT.
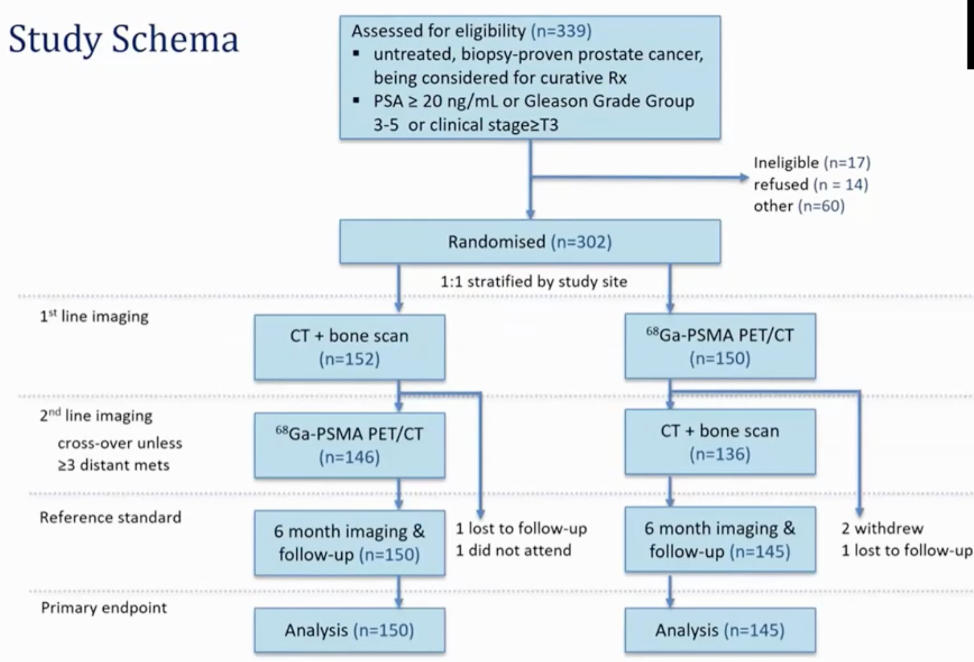
In the proPSMA trial, 302 men were randomly assigned: 152 (50%) men to conventional imaging and 150 (50%) to PSMA PET-CT, with balanced baseline characteristics. Of 295 (98%) men with follow-up, 87 (30%) had pelvic nodal or distant metastatic disease.1 After conventional imaging, men were then crossed-over to receive the other modality of imaging:
The primary endpoint for this study was the accuracy of PSMA PET-CT, which had a 27% (95% confidence interval [CI] 23-31) greater accuracy than that of conventional imaging (92% [88-95] vs 65% [60-69]; p<0.0001):
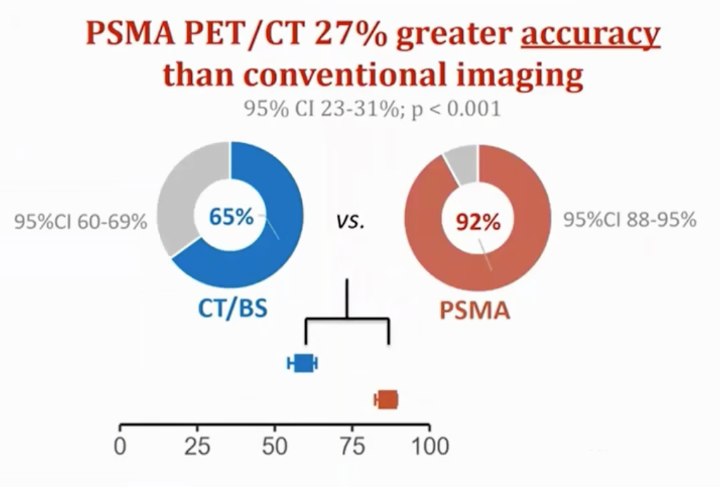
PSMA PET-CT compared to conventional imaging had a higher sensitivity and specificity for the detection of any metastatic disease, which was true for pelvic nodal and distant metastases groups. Additionally, in a sensitivity analysis, there was superior accuracy with PSMA PET-CT if equivocal lesions were considered positive rather than negative. A key secondary endpoint in the proPSMA study was the change in patient management. Dr. Eapen notes that first-line conventional imaging conferred management change less frequently (23 [15%] men [10-22] vs. 41 [28%] men [21-36]; p=0.008) and had more equivocal findings (23% [17-31] vs. 7% [4-13]) than PSMA PET-CT. In patients who underwent second-line imaging, management change occurred in seven (5%) of 136 patients following conventional imaging, and in 39 (27%) of 146 following PSMA PET-CT. Furthermore, radiation exposure was 10.9 mSv (95% CI 9.8-12.0) higher for conventional imaging than for PSMA PET-CT (19.2 mSv vs 8.4 mSv; p<0.001), and there was high reporter agreement for PSMA PET-CT, with a κ=0.87 for nodal disease and κ=0.88 for distant metastases.
One of the main questions that emerged from proPSMA is if conventional imaging is negative but novel imaging shows metastatic disease, do we abandon the standard of care (surgery or radiotherapy)? Whether we should try harder for a tissue diagnosis and how we assess the management impact remains to be established.
Dr. Eapen concluded that metastatic disease should be defined by novel imaging:
- Defining the extent of disease is critical for decision making and more accurate imaging may improve outcomes
- The proPSMA study demonstrated superior accuracy of PSMA PET/CT to conventional imaging and is a “one-stop shop” single scan
- Management impact needs further evaluation, but it does allow for improved patient counseling and offers theranostic possibilities
Presented by: Renu Eapen, MD, Consultant Urologist, Peter MacCallum Cancer Centre, Melbourne, Australia
Written by: Zachary Klaassen, MD, MSc, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md at the 2020 Société Internationale d'Urologie Virtual Congress (#SIU2020), October 10th - October 11th, 2020
Reference:
1. Hofman, Michael S., Nathan Lawrentschuk, Roslyn J. Francis, Colin Tang, Ian Vela, Paul Thomas, Natalie Rutherford et al. "Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multi-centre study." The Lancet (2020).
Related Content:
Read the Opposing Debate: SIU Virtual Congress 2020: Debate: Imaging in the Definition of Oligometastatic Prostate Cancer - Oligometastatic Disease Should be Defined Based on Standard Imaging Modalities
Watch: PSMA PET/CT Imaging for Staging High-risk Prostate Cancer Prior to Curative-intent Surgery or Radiotherapy (proPSMA) - Michael Hofman and Declan Murphy
Read: EAU 2020: ProPSMA Study: A Prospective Randomised Multi-Centre Study of PSMA-PET/CT Imaging for Staging High Risk Prostate Cancer Prior to Curative-Intent Surgery or Radiotherapy


