(UroToday.com) The Société Internationale D’Urologie (SIU) 2021 annual meeting included a hot topics session on PSMA theranostics with a presentation by Dr. Tobias Maurer discussing the role of targeted salvage surgery in biochemical recurrence. Dr. Maurer started by highlighting from the EAU guidelines that salvage lymph node dissection is not a standard treatment, specifically that “high-level evidence for the oncological value of salvage lymph node dissection is still lacking.”
Long-term outcomes of patients treated with salvage lymph node dissection for nodal recurrence until recently were essentially unknown. Bravi et al.1 undertook a multi-institutional approach to assess these long-term outcomes, including 189 patients who experienced PSA rise and nodal-only recurrence after radical prostatectomy and underwent salvage lymph node dissection at 11 centers between 2002 and 2011. Recurrences were detected with either 11C-choline or 68Ga PSMA. The primary outcome was cancer-specific mortality, and the secondary outcomes were overall mortality, clinical recurrence, biochemical recurrence, and androgen deprivation therapy (ADT)-free survival after salvage lymph node dissection. There were 110 and 163 patients who experienced clinical recurrence and biochemical recurrence, respectively, with clinical recurrence-free and biochemical recurrence-free survival at 10 years of 31% and 11%, respectively. After salvage lymph node dissection, a total of 145 patients received ADT, with a median time to ADT of 41 months:
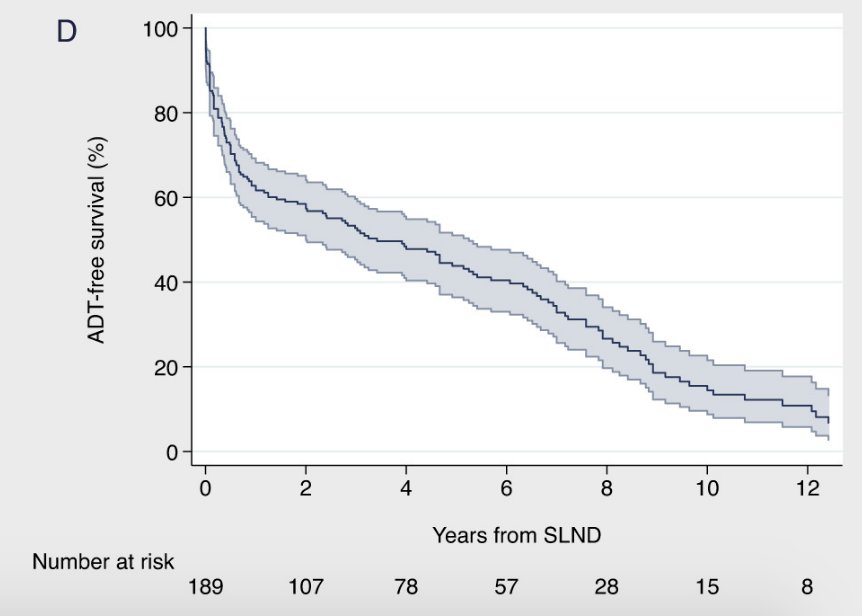
Importantly, additional therapy was warranted in >60% of patients within 6 months of salvage lymph node dissection. At a median follow-up for survivors of 87 (IQR 51 to 104) months, 48 patients died, of which 45 died from prostate cancer. At multivariable analyses, patients who had PSA response after salvage lymph node dissection (HR 0.45; p = 0.001), and those receiving ADT within 6 months from salvage lymph node dissection (HR 0.51; p = 0.010) had a lower risk of death from prostate cancer.
Dr. Maurer notes that there are several aims and criteria of salvage lymph node dissection in the setting of biochemical recurrence:
- Aims:
- Delaying palliative treatment (and associated toxicity)
- Prevention of local complications
- “Permanent cure”?
- Criteria:
- Pelvic location
- Low number of metastases on imaging
- Low PSA prior to salvage lymph node dissection
- No ADT at the time of imaging/salvage lymph node dissection
- In 2021: PSMA PET should represent the basis for salvage lymph node dissection
The challenge of salvage surgery is the intraoperative detection of small lymph nodes in the pelvis. One way to assist with detection is to use PSMA-radioguided surgery, which includes a preoperative IV injection of 111In- or 99mTc-labeled PSMA-ligand and subsequently facilitates intraoperative detection of metastatic lesions by gamma probe:

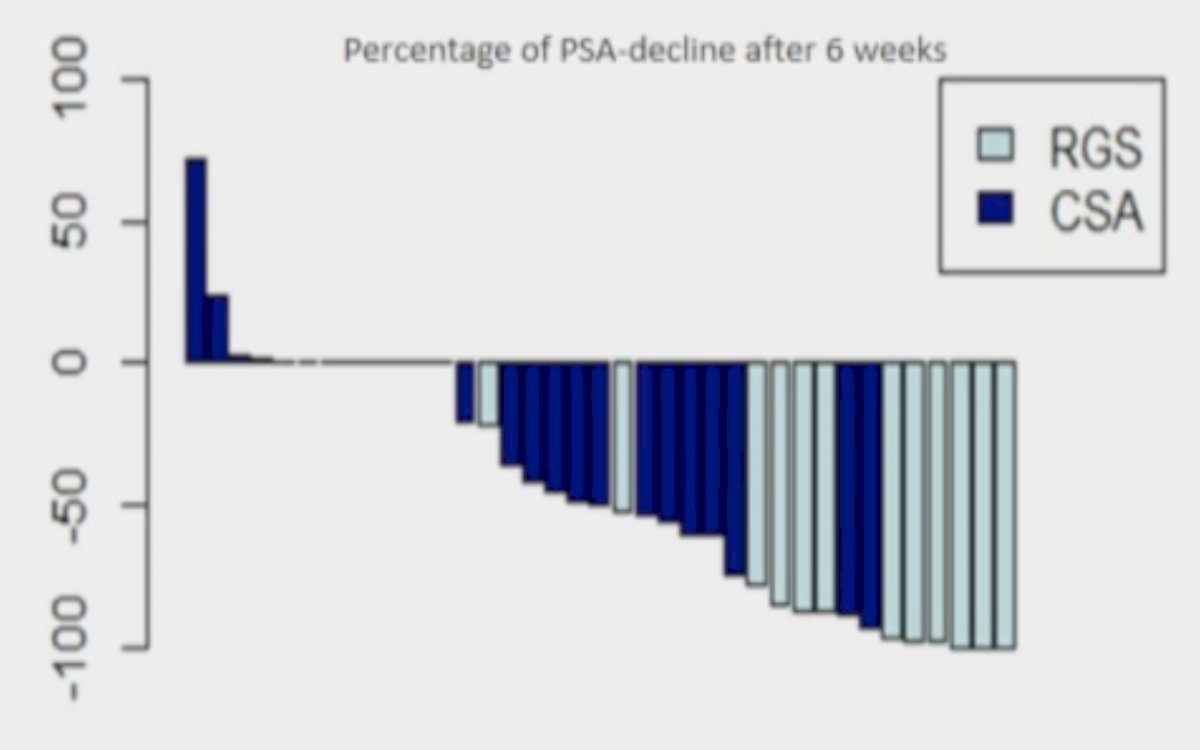
To assess whether PSMA-radioguided surgery is better than conventional surgery, Knipper et al.2 prospectively analyzed 42 consecutive patients who underwent salvage lymph node dissection based on preoperative 68Ga-PSMA-PET imaging between 2015 and 2018. In 29 patients, the dissection field was based solely 68Ga-PSMA-PET imaging (conventional surgical approach), whereas 13 patients underwent 99mTc-PSMA-radioguided surgery. Final pathology revealed no metastases in nine conventional surgical approach patients (31%), whereas all visible lesions on preoperative 68Ga-PSMA-PET were removed in patients who underwent radioguided surgery. A PSA decline in general, >50% and >90% within 6 weeks was seen in 50%, 29%, and 7% versus 100%, 92%, and 53% in conventional surgical approach versus radioguided surgery groups, respectively (all p<0.01):
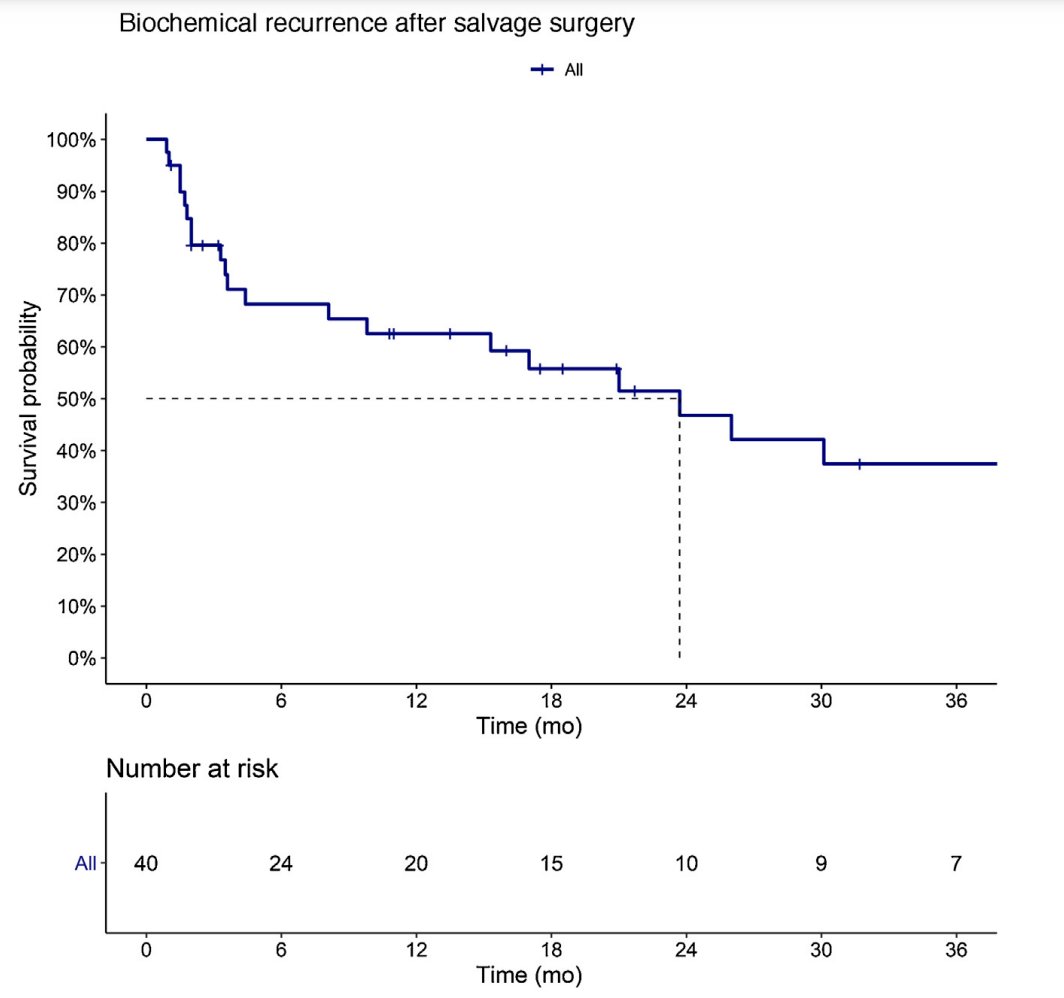
In follow-up work from Dr. Knipper and Maurer’s group (unpublished) using 99mTc-PSMA-radioguided surgery, their cohort is now 377 patients (2014-2020) with a median preoperative PSA of 1.0 (IQR 0.5-1.9) ng/ml, and 53.6% of patients having a clinical biochemical response (PSA < 0.2 ng/mL) after salvage lymph node dissection. However, median biochemical recurrence-free survival was only 7.8 months (without additional therapy), which according to Dr. Maurer is secondary to ~50% of patients never reaching a clinical biochemical response. The median therapy-free survival in this cohort is nearly 3 years (~34.9 months).
With regards to surgical treatment of local recurrence after radiotherapy, Dr. Maurer’s group has also assessed the utility of PSMA-radioguided surgery
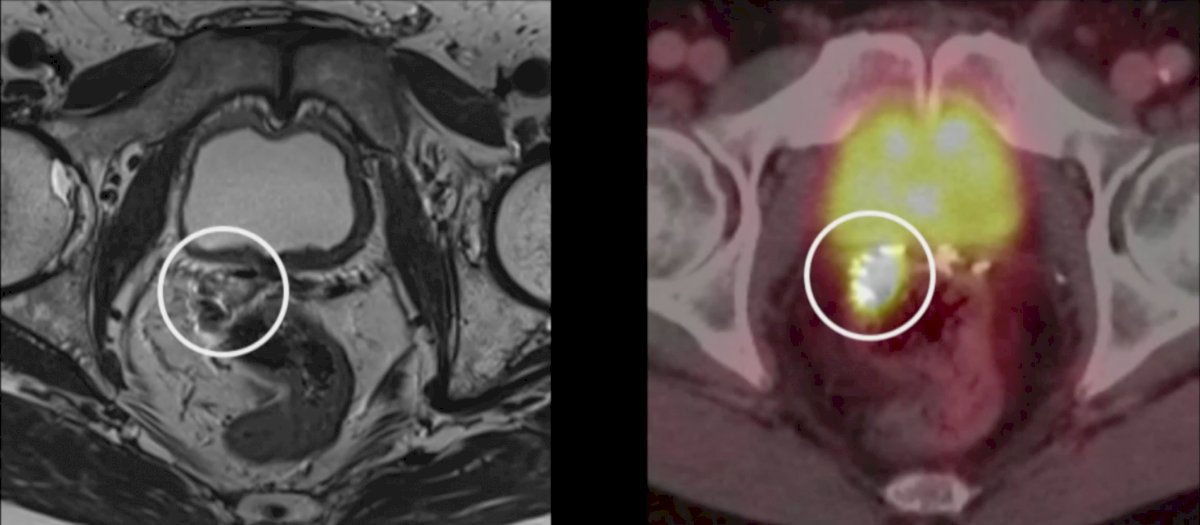
In this study, 40 patients were treated with open salvage surgery in two centers (2014-2020), with all patients presenting with biochemical recurrence after radical prostatectomy with a singular local recurrence at PSMA PET imaging. Among these patients, 33 (82.5%) received previous salvage radiation therapy. Prior to salvage surgery, the median PSA was 0.9 ng/ml (IQR 0.5–1.7 ng/ml), and postoperatively the median PSA nadir was 0.1 ng/ml (IQR 0–0.4 ng/ml). In 31 (77.5%) patients, clinical biochemical response was observed. Over a median follow-up of 24.4 months, 22 (55.0%) patients experienced biochemical recurrence and 12 (30.0%) received further therapy. At 1 year of follow-up, the biochemical-free survival rate was 62.2% and treatment free survival rate was 88.3%:
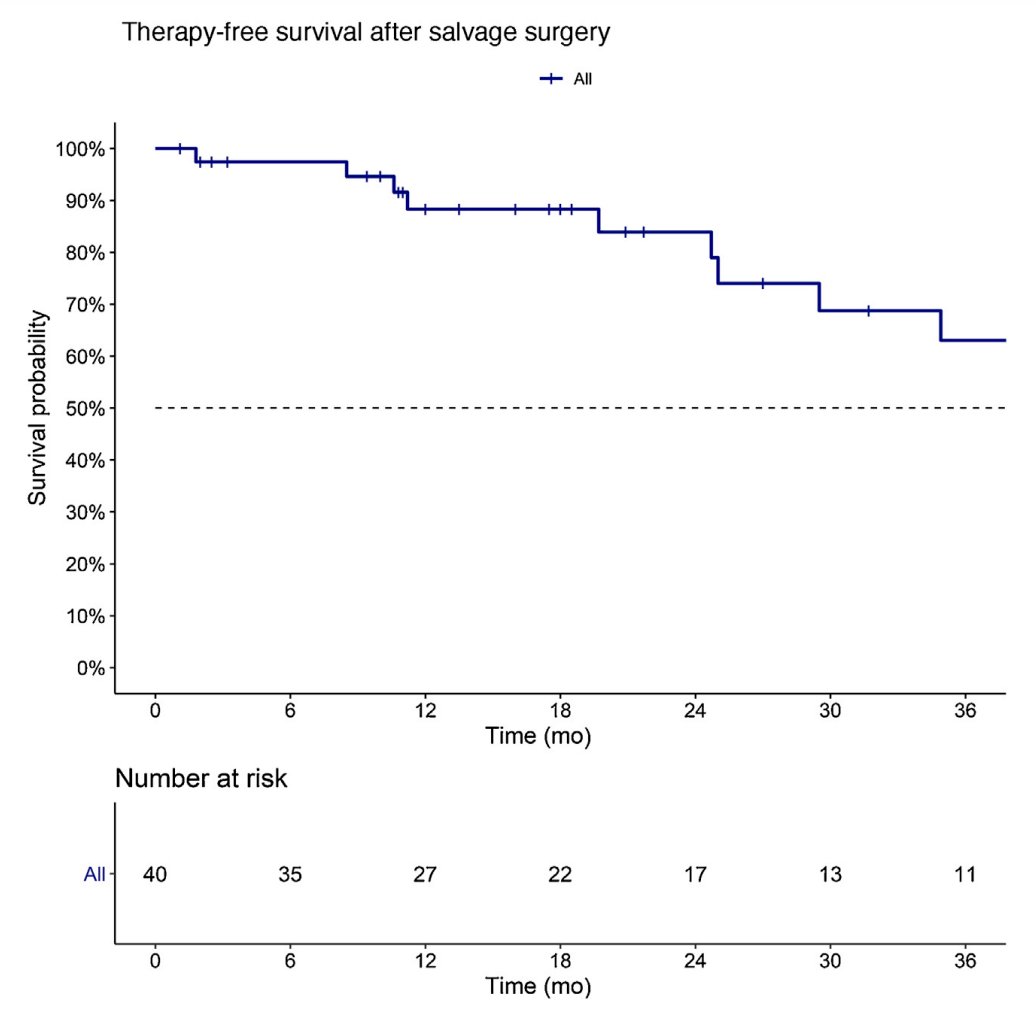
The previous studies discussed by Dr. Maurer were all open salvage procedures, however recently they have been able to use robotic surgery for salvage therapy based on the advent of a drop-in gamma probe to facilitate robotic minimally-invasive PSMA-radioguided surgery. Additionally, in work that is accepted but not yet published, Dr. Maurer notes that patient selection for PSMA-radioguided surgery may be aided by biomarkers, specifically circulating tumor cells. Both biochemical recurrence (p = 0.018) and therapy free survival (p=0.2) was improved for circulating tumor cell negative versus circulating tumor cell positive patients. Based on this work, Dr. Maurer and colleagues have started the BioPoP (NCT04324983) study, with an aim of identifying predictive biomarkers for successful salvage surgery in PSMA PET positive oligometastatic prostate cancer. The goal is 150 patients in this trial (have currently enrolled 90 patients), with the key inclusion criteria that patients are already scheduled for PSMA-radioguided surgery. Key measurements for biomarker discovery including circulating tumor cells, extracellular vesicles, circulating DNA, Cyr61, and tissue specimens.
Another study from Dr. Maurer’s group is the ProSTone (NCT04271579) trial assessing the extent of salvage lymph node dissection (given that a bilateral template is “standard”), specifically assessing if one-sided salvage extended lymph node dissection is enough for these patients. This is a prospective, multicenter trial (goal of n=397), with 1:1 randomization to unilateral versus bilateral salvage lymph node dissection. Key inclusion criteria are 1-3 PSMA PET positive lymph nodes and a PSA < 4 ng/mL.
With regards to the future, Dr. Maurer notes that this will likely include fluorescent and/or hybrid PSMA tracers to ease guidance of PSMA-radioguided surgery:
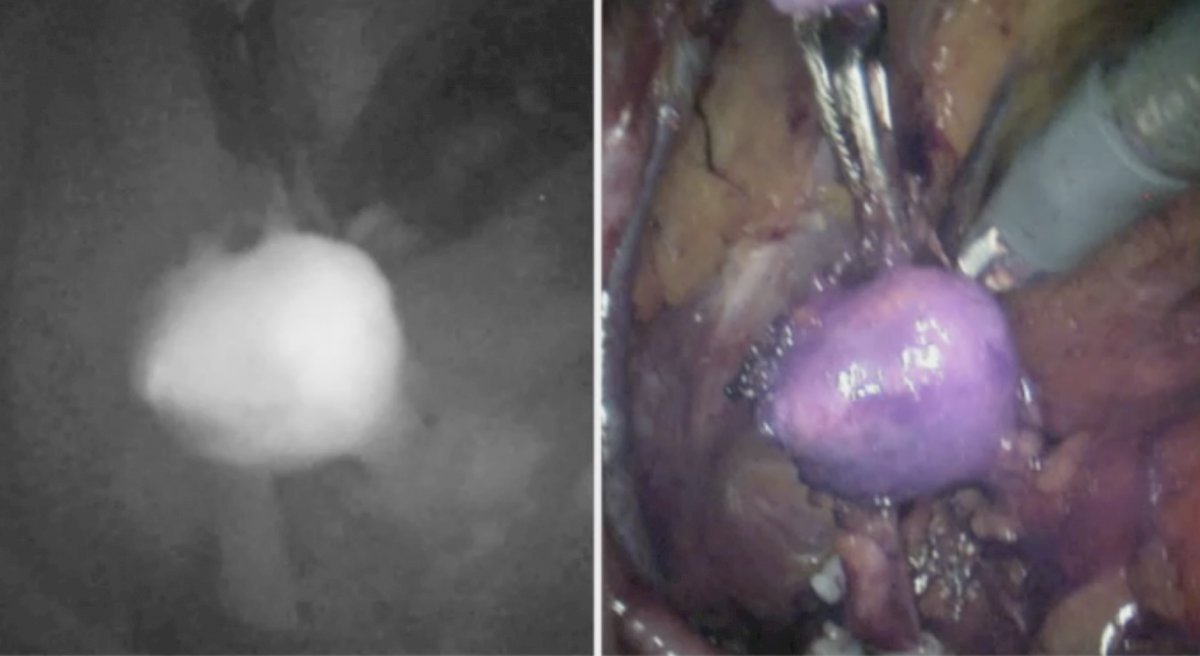
Dr. Maurer concluded his presentation assessing the role of targeted salvage surgery in biochemically recurrent prostate cancer with the following take-home messages:
- Metastasis directed therapy is still outside the current guideline recommendations
- If considered, metastasis directed therapy should be based on novel molecular imaging (PSMA-PET)
- As follows is the proposed treatment landscape in the biochemical recurrent-setting:
Presented by: Tobias Maurer, MD, Department of Urology, Martini-Klinik, University Hospital Hamburg-Eppendorf, Hamburg, Germany
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 Société Internationale D’Urologie (SIU) Hybrid Annual Meeting, Wed, Nov 10 – Sun, Nov 14, 2021.
References:
- Bravi CA, Fossai N, Gandaglia G, et al. Long-term Outcomes of Salvage Lymph node dissection for nodal recurrence of prostate cancer after radical prostatectomy: Not as Good as Previously Thought. Eur Urol 2020 Nov;78(5):661-669.
- Knipper S, Tilki D, Mansholt J, Berliner C, et al. Metastases yield and prostate-specific antigen kinetics following salvage lymph node dissection for prostate cancer: A comparison between conventional surgical approach and prostate-specific membrane antigen-radioguided surgery. Eur Urol Focus. 2019 Jan;5(1):50-53.
- Knipper S, Ascalone L, Ziegler B, et al. Salvage surgery in patients with local recurrence after radical prostatectomy. Eur Urol. 2021 79:537-544.


