(UroToday.com) The Société Internationale D’Urologie (SIU) 2021 annual meeting included a plenary session with the EAU lecture provided by Dr. Arnulf Stenzl discussing comorbidity tailored treatment of prostate cancer. Dr. Stenzl started his presentation by highlighting that the EAU 22 meeting will be held, in person, in Amsterdam from March 18-21, 2022, with four full days of scientific program and exhibition, 1,200+ speakers, 1,700+ posters and video abstracts, and live surgeries. With regards to prostate cancer and comorbidity, there are three important ‘Ps’ we should remember:
- Predisposition: when is it advisable to check?
- Prevention: is it possible to avoid (or “postpone”) development?
- Prediction: course of the disease versus life expectancy
Over the last several years the genomic alterations in prostate cancer, as well as the identification and importance of germline mutations have become readily apparent. Approximately 15.6% of men with prostate cancer have tested pathogenic variants identified in genes (BRCA1, BRCA2, HOXB13, MLH1, MSH2, PMS2, MSH6, EPCAM, ATM, CHEK2, NBN, and TP53). Furthermore, 10.9% of men have germline pathogenic variants in DNA repair genes, with the most common identified being BRCA2 (4.5%), CHEK2 (2.2%), ATM (1.8%), and BRCA1 (1.1%). BRCA2 mutation carriers are associated with a higher incidence of prostate cancer, a younger age of diagnosis, and more clinically significant tumors, as well as the aggressiveness of prostate cancer. Based on the PROfound trial1 showing an improvement in overall survival among those being treated with PARP inhibition with alterations in BRCA1/2 and ATM, the EMA has approved olaparib for “metastatic prostate cancer in men with mutations in BRCA1 or BRCA2 genes in whom medical or surgical treatment to lower testosterone levels (castration) did not work and whose cancer has worsened after treatment with other prostate cancer medicines, including a new hormonal agent.”
Dr. Stenzl notes that a body of literature has suggested that more high-risk and very-high risk prostate cancer is associated with decreased overall survival in patients with type 2 diabetes mellitus:
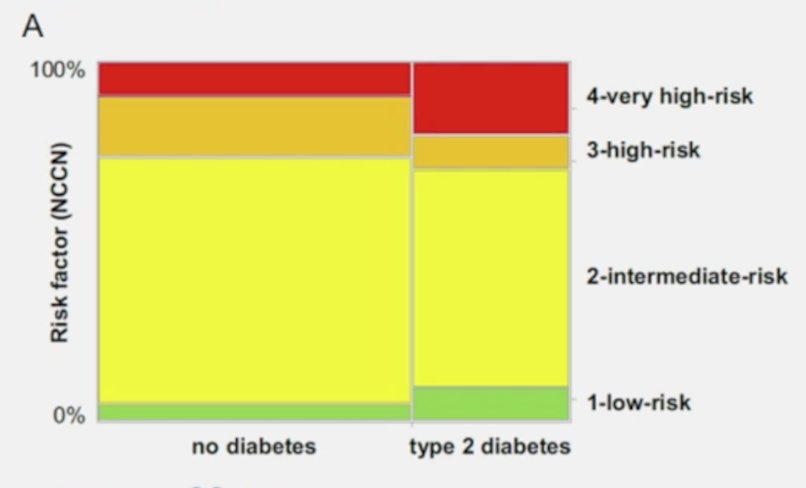
This is likely secondary to enhanced expression of the androgen receptor in prostate cancer and stronger activation of androgen signaling in men with type 2 diabetes. Additionally, tumor-tissue and adjacent tumor tissue have shown altered levels of IR isoforms A and B in favor of isoform A and the IRS-1 to IRS-2 ratio differs in favor of IRS-2 supporting the involvement of the insulin-cascade in pathogenesis.
Metabolic syndrome and the role it plays in prostate cancer has also been added to the EAU guideline, specifically:
- Hypertension: associated with an increased risk of prostate cancer
- Waist circumference: > 102 cm is associated with an increased risk of prostate cancer
- Diabetes: type 2 diabetes mellitus is associated with the development of higher risk aggressive prostate cancer
- Obesity: is associated with a lower risk of low-grade prostate cancer (OR 0.79, p=0.01), but increased risk of high-grade prostate cancer (OR 1.28, p=0.042). This may be secondary to difficulty assessing T-stage via digital rectal exam in obese men.
With regards to prostate cancer development and life style, exogenous/environmental factors have been discussed as being associated with risk of developing prostate cancer or as being etiologically important for the progression from latent to clinical prostate cancer. Japanese men have a lower risk of prostate cancer risk compared to men from the Western world. However, as Japanese men move from Japan to California, their risk of prostate cancer increases, approaching that of American men, implying a role of environmental or dietary factors.
Bigaran and colleagues recently assessed the effect of exercise on cardiometabolic health in men with prostate cancer receiving ADT by performing a systematic review and meta-analysis of the literature.2 Among 14 randomized controlled trials and four non-randomized studies, exercise training improved the following compared to usual care:
- 400-m-walk test (MD −10.11 s, 95% CI [−14.34, −5.88]; p < 0·00001)
- Diastolic blood pressure (−2.22 mmHg, [−3.82, −0.61]; p = 0.007)
- Fasting blood glucose (−0.38 mmol/L, [−0.65, −0.11]; p = 0.006)
- C-reactive protein (−1.16 mg/L, [−2.11, −0.20]; p = 0.02)
- Whole-body lean mass (0.70 kg, [0.39, 1.01]; p < 0.0001)
- Appendicular lean mass (0.59 kg, [0.43, 0.76]; p < 0.00001)
- Whole-body fat mass (−0.67 kg, [−1.08, −0.27]; p = 0.001)
- Whole-body fat percentage (−0.79%, [−1.16, −0.42]; p < 0.0001)
- Trunk fat mass (−0.49 kg, [−0.87, −0.12]; p = 0.01)
The tumor-promoting effects of obesity occur at the local level via adipose inflammation and associated alterations in the microenvironment, as well as systemically via circulating metabolic and inflammatory mediators associated with adipose inflammation. Accurately characterizing the obese stage and identifying patients at increased risk of cancer development and progression will likely require more precise assessments than body-mass index alone. Biomarkers of adipose tissue inflammation would help to identify high-risk populations. Moreover, adipose inflammation is a reversible process and represents a novel therapeutic target that warrants further study to break the obesity-cancer link. Weight reduction via diet and/or exercise can restore many pathways that are dysregulated in the obese state and are of significant interest for cancer prevention and treatment. Epidemiologically, the risk of obesity and prostate cancer may be reversible. Men who lose weight in the period from shortly before to after prostate cancer diagnose may have a lower risk of recurrence, whereas weight gain is positively associated with recurrence after prostatectomy.
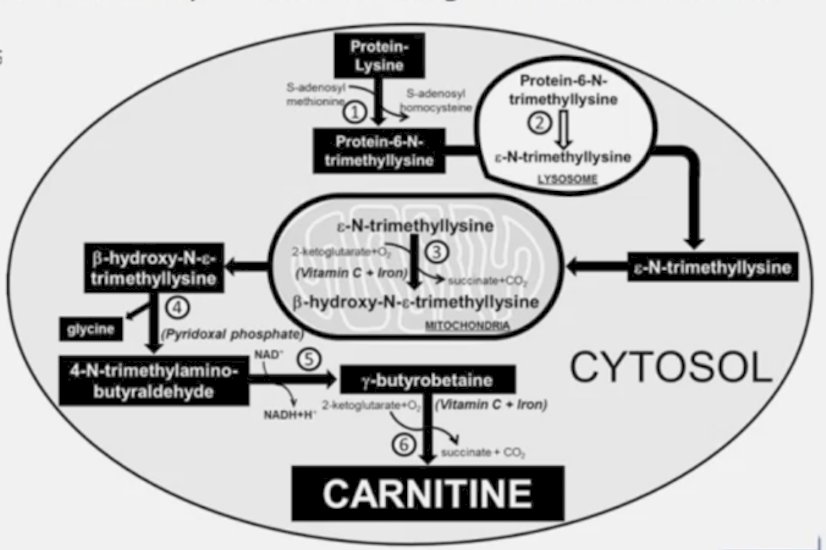
There has also been increased interest in the role of the urine metabolome of prostate cancer. In unpublished data, Dr. Stenzl notes that fatty acid oxidation is the most dominant bioenergetics pathway in prostate cancer, finding that significantly reduced levels of acylcarnitines reflect a reduction in beta-oxidation after radical prostatectomy. In contrast, an increase in citric acid levels conferred increased prostate cancer aggressiveness:
Dr. Stenzl emphasized that comorbidity is more important than age in predicting life expectancy in men with prostate cancer. Albertsen et al.3 conducted a 10-year competing risk analysis of 19,639 men 66 years of age and older identified in the SEER-Medicare database with the goal of providing patients and clinicians more accurate estimates of comorbidity-specific survival stratified by patient age, tumor stage, and tumor grade. During the first 10 years after diagnosis, men with moderately and poorly differentiated prostate cancer were more likely to die from causes other than their disease. Depending on patient age, Gleason score, and number of comorbidities present at diagnosis, 5-year overall mortality rates for men with stage T1c disease ranged from 11.7% (95% CI, 10.2% to 13.1%) to 65.7% (95% CI, 55.9% to 70.1%), and prostate cancer-specific mortality rates ranged from 1.1% (95% CI, 0.0% to 2.7%) to 16.3% (95% CI, 13.8% to 19.4%). Ten-year overall mortality rates ranged from 28.8% (95% CI, 25.3% to 32.6%) to 94.3% (95% CI, 87.4% to 100%), and prostate cancer-specific mortality rates ranged from 2.0% (95% CI, 0.0% to 5.3%) to 27.5% (95% CI, 21.5% to 36.5%). Ultimately, most men with a Charlson Comorbidity Index score of >2 died from competing causes at 10 years of follow-up regardless of their age at the time of diagnosis.
Dr. Stenzl concluded his presentation by once again highlighting the three ‘Ps’ of prostate cancer and comorbidity:
- Predisposition: racial and genetic factors
- Prevention: decreasing obesity with exercise and very low-calorie diets
- Prediction: genetic, adipose tissue inflammation, urine metabolome
Presented by: Arnulf Stenzl, MD, University of Tübingen Medical Center, Tübingen, Germany
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 Société Internationale D’Urologie (SIU) Hybrid Annual Meeting, Wed, Nov 10 – Sun, Nov 14, 2021.
References:
- de Bono J, Mateo J, Fizazi K, et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med 2020 May 28;382(22):2091-2102.
- Bigaran A, Zopf E, Gardner J, et al. The effect of exercise training on cardiometabolic health in men with prostate cancer receiving androgen deprivation therapy: a systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2021 Mar;24(1):35-48.
- Albertsen PC, Moore DF, Shih W, et al. Impact of comorbidity on survival among men with localized prostate cancer. J Clin Oncol. 2011 Apr 1;29(10):1335-1341.