(UroToday.com) In the Plenary session of the Société Internationale D’Urologie (SIU) 2021 annual meeting, Dr. Mark Emberton presented the SIU-Mostafa M. Elhilali Award Lecture focusing on his reflections on the evolution of prostate cancer treatment.
After acknowledging the important contributions of Dr. Elhilali, Dr. Embrton moved to note the contributions of Hugh Hampton Young, who performed the first radical prostatectomy in April 1904. Since that time, prostate cancer treatment has been undertaken without image guidance. In fact, Dr. Emberton emphasized, only in the past two decades have we had imaging approaches, namely multiparametric magnetic resonance imaging (mpMRI), which allow for useful guidance in the treatment of patients with localized disease.
MpMRI has allowed a detailed understanding of prostate anatomy, its relationship to adjacent organs, and of prostate tumors. In particular, Dr. Emberton highlighted the ability of mpMRI to identify and diagnose tumors in the anterior aspect of the prostate, tumors that may be missed through a physical examination with digital rectal examination and transrectal ultrasound (TRUS) as well as with systematic TRUS-guided biopsies.
While the first publication of prostate MRI was published in 1984, there have been dramatic technological advancements in the past decades. The clinical utility of these technical advances has only recently begun to be fully appreciated and acted upon to improve patient care and outcomes. Prior to routine prostate imaging, prostate cancer risk stratification failed to account for tumor volume, tumor location, tumor morphology, clustering of tumors, imaging phenotypes, radio-genomics, the method of sampling, or anatomic adjacencies. He, therefore, described these as “rudimentary at best”.
He then concentrated on the question of tumor location. He first noted that radiotherapy is now often delivered on the basis of a treatment plan informed by mpMRI findings, a term coined “dose-painting” with increased dose delivered to the radiographically obvious tumor. This has the potential to allow for increased dose delivery to the tumor with sparing of normal tissues, potentially increasing efficacy and decreasing toxicity.
From a surgical perspective, Dr. Emberton emphasized the increasingly important role of tumor location in surgical planning and patient counseling and education. In particular, he cited the example of planned nerve sparing on the basis of MRI findings. Further, recent work has used 3-D printing for surgical planning and patient counseling.
In addition to helping to evolve current treatment paradigms, Dr. Emberton further emphasized that this anatomic understanding of prostate cancer has allowed a new class of therapy for patients with prostate cancer, namely focal therapy. This lies somewhat intermediate between active surveillance and traditional whole gland treatment approaches. Dr. Emberton emphasized that the traditional active surveillance vs whole gland treatment paradigm relies on a threshold-based treatment decision.
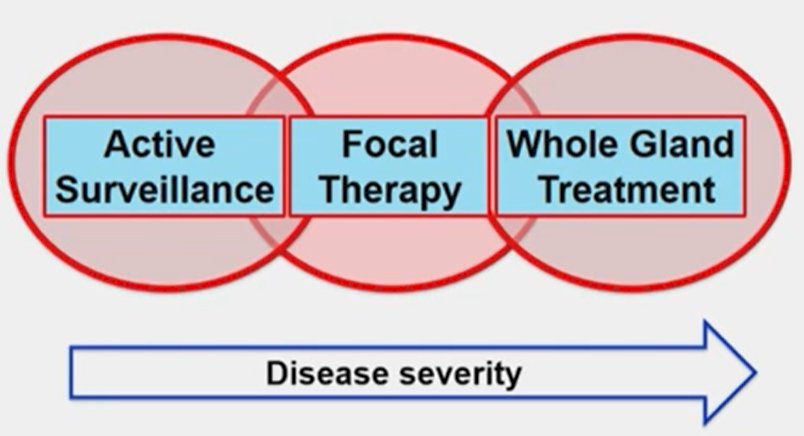
Focal therapy allows an intent to treat the radiographically apparent tumor (with a margin of normal tissue) while sparing additional normal tissues. Over time, this approach has evolved from hemi-gland therapy to more focused treatment approaches, in part based on improved understanding of the positive and negative predictive values of the imaging approaches. Currently, he emphasized that focal therapy often incorporates the principles of active surveillance, with planned treatment to clinically significant index lesions with surveillance of secondary, clinically insignificant disease.
Citing data that is now more than 10 years old, Dr. Emberton emphasized that the majority of patients treated with focal therapy on the NCRN Multicentre INDEX trial, 90% had intermediate or high-risk disease, with a minority having low-risk disease. Today, he emphasized that those with low-risk disease should be treated expectantly. However, this “tissue selective” treatment paradigm is, in Dr. Emberton’s view, complementary to surveillance among patients with low-risk disease and whole gland treatment in patients with more extensive or aggressive disease.
He emphasized that reviews of this approach were initially very skeptical, however, these results were then treated with substantial interest and excitement. He noted editorial commentary from Dr. Walsh who has very critical of publication using mpMRI as an endpoint for high-intensity focused ultrasound. However, over time, there has been an increasing body of evidence supporting this approach.
As the evidentiary body has grown, Dr. Emberton emphasized that a number of different technologies have been shown to predictably and reliably destroy tissue, including extremes of temperature (direct and indirect applications), high-voltage current, high-dose rate radiotherapy, laser light, toxic direct injection, and cancer selective treatments.
Dr. Emberton then discussed patients who would be eligible for focal therapy, emphasizing that this includes patients with a discrete lesion on MRI who have clinically significant prostate cancer on biopsy, tumor location which allows the opportunity to apply a margin (of 5mm), and a high utility for preserving genitourinary function (particularly erectile function, as this is where focal therapy outcomes differ most substantially from whole gland treatment). Further, patients must have an awareness and acceptance of the uncertainty of this treatment approach, as well as an awareness and acceptance of salvage strategies if focal therapy were to prove ineffective or insufficient.
When applied in this manner, Dr. Emberton emphasized that many groups have demonstrated promising results from phase I and phase II studies. In their cohort, 89% of men achieved the trifecta of pad-free, leak-free continence, erections sufficient for intercourse, and cancer control at 12 months with focal HIFU. Moving forward, he emphasized that technology (with augmented reality informed by mpMRI and exported to the HIFU platform) allows for increasingly precise treatment targeting, as well as the generation of treatment margins.
He then cited a number of examples using focal HIFU, cryotherapy, and IRE. Based on a systemic review of trials published to date, erectile function is very well preserved with this treatment approach. Notably, PDE-5 inhibitor usage increased by about 30% in the first year following focal therapy, however. In a randomized comparison with active surveillance, both urinary and sexual functions were comparable. Further, grade 2 complications were somewhat higher among treated patients (41% vs 25%); however, grade 3 (9.6% vs 9.6%) and grade 4 events (0.5% vs 0.5%) were comparable.
He, therefore, summarized that the last decade of prostate cancer treatment has been driven by the novel understanding of tumor location which has driven more precise risk-stratification. This has both improved existing treatments and opened up novel therapeutic approaches.


