(UroToday.com) In the Plenary session of the Société Internationale D’Urologie (SIU) 2021 annual meeting Dr. Peter Mulders presented a state-of-the-art lecture on novel therapies in renal cell carcinoma (RCC) and the role of nephrectomy in this rapidly evolving treatment landscape.
Dr. Mulders went back to the seminal publication in 2001 of the role of nephrectomy followed by interferon alpha-2b compared to interferon alpha-2b alone in patients with metastatic RCC. While we have now come back to immunotherapy using immune checkpoint inhibitors, this trial did examine the role of cytoreductive surgery in the context of aspecific immunotherapy. Notably, this study was based, in part, on the observations of spontaneous tumor regression following nephrectomy. Further, this offers the potential to start systemic therapy upon disease progression. In this trial, cytoreductive nephrectomy was associated with an overall survival benefit. Additionally, he emphasized that a small subset of patients treated in this way with interferon were entirely cured of their disease.
On the basis of these data, tumor nephrectomy was recommended with a grade A recommendation in the EAU guidelines on Renal Cell Carcinoma among patients with mRCC who have a good performance status and when treatment is combined with interferon-alpha.
Moving forward, anti-angiogenic agents and tyrosine kinase inhibitors became standard of care for patients with advanced and metastatic RCC, supplanting the cytokines. Dr. Mulders noted that in the pivot trials that led to the acceptance and approval of these agents, the vast majority of patients (79 to 92%) had previously undergone nephrectomy. However, it took many years to complete the randomized trial assessing the role of cytoreductive nephrectomy among patients receiving these agents. He highlighted that, in the meantime, we depended on retrospective analyses. These studies, prone to selection bias, demonstrated improved survival among patients with cytoreductive nephrectomy. Early work from the IMDC group demonstrated that this effect was moderated in part from performance status, with a greater benefit among those with Karnofsky performance status of 80 or greater. Further, work demonstrated that tumor size less than 7cm and a majority of tumor volume confined to the kidney were prognostic.
Two important trials sought to address related questions in this disease space: CARMENA and SURTIME. While CARMENA addressed the question of the role of cytoreductive surgery, SURTIME more specifically addressed the question of its timing.
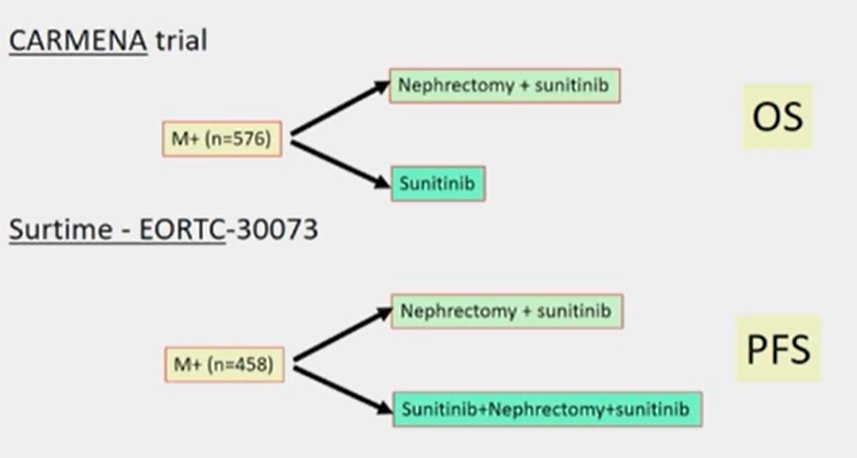
Published in 2018 in the New England Journal of Medicine, the CARMENA trial did not demonstrate a benefit to the combination of cytoreductive nephrectomy and sunitinib, compared to sunitinib alone. However, Dr. Mulders emphasized the importance of understanding which patients dropped out and who continued through their planned treatment. In particular, he noted a preponderance of patients with poor-prognosis. Further, nearly one-fifth of patients did not receive what he termed “optimal” treatment, within their allocated arm. Based on the conclusion of this trial that sunitinib alone was not inferior, he observed that fewer and fewer cytoreductive nephrectomies are performed. Dr. Mulders emphasized that decreasing volumes of surgery are important given the importance of facility with this operative approach.
Dr. Mulders then discussed the SURTIME trial which utilized a multidisciplinary treatment approach, with all patients receiving surgery and systemic therapy. He emphasized that, while it was a protocol violation, they typically delayed the initiation of sunitinib therapy following surgery until there was evidence of disease progression (on average one year, though much longer in some). In contrast, an initial systemic therapy approach allows optimal selection of patients (without disease progression) for surgery who are most likely to benefit. Further, SURTIME demonstrated that the morbidity of surgery was not increased.
Even since CARMENA and SURTIME enrolled, there have been substantial advances in the systemic therapies used for mRCC including immunotherapy, novel tyrosine kinases, combinations of these approaches, and newer experimental approaches (including CAR t-cell and NK-cells). In general, these treatments are chronic and palliative, rather than curative, in nature. Thus, he emphasized the potential value of surgery by delaying systemic therapy and its associated toxicity.
In mRCC treatment which is predominately palliative in nature, he emphasized the importance of balancing efficacy and toxicity of both systemic therapy and surgery. In the surgical context, the morbidity of surgery is higher for cytoreductive surgery than for surgery in the localized setting. However, he made a number of arguments (based initially on reports from 10 years ago) in support of the role of cytoreductive nephrectomy: palliation of local symptoms, treatment of primary tumor which has not responded to systemic therapy, delaying the time to disease progression, the ability to potentially improve survival or response to systemic therapy, in cases where systemic therapy has not be very effective, the potential (though rare) for spontaneous regression, and the importance of adequate histologic characterization. Further, he emphasized that most trials of systemic therapies have been performed in patients who have undergone nephrectomy. However, these may be balanced by arguments against cytoreductive surgery including the significant surgical morbidity and mortality, a lack of proven benefit among systemic therapies other than interferon, the potential that patients may spend a large proportion of their time recovering from surgery, the potential for systemic disease progression during the recovery from surgery which may preclude systemic therapy, and the delay in the initiation of systemic therapy.
In making these decisions, he emphasized the importance of prognostic classification. For patients with a primary tumor in situ, these patients always will be classified as intermediate or poor-risk disease. In a multi-disciplinary setting, he emphasized the importance of considering patient, tumor, and other characteristics.
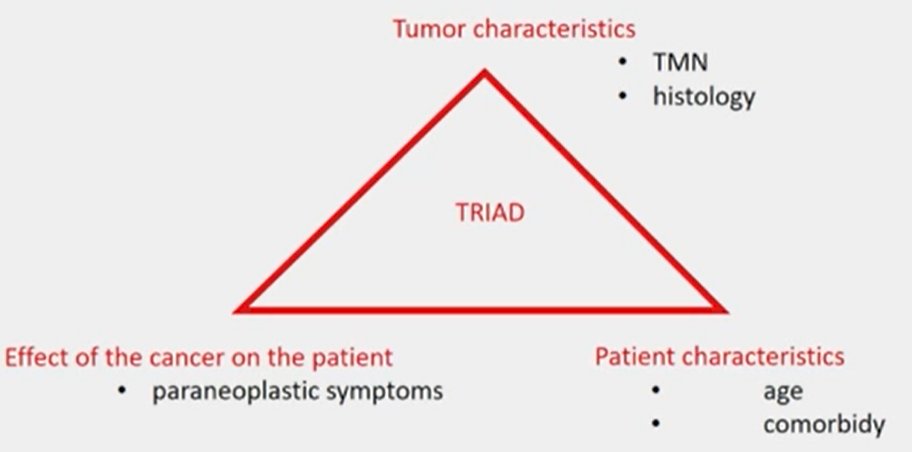
He highlighted that patients with paraneoplastic syndromes may have their symptoms ameliorated by resection of the primary tumor. Building off this principle, he suggested that surgery benefits patients with mRCC when it is palliative as it may improve quality of life delays systemic therapy, and may affect survival. Thus, when deciding on the role of cytoreductive surgery, we must consider to what degree we may achieve these ends.
Presented by: Peter Mulders, MD, PhD, University Medical Center Nijmegen, The Netherlands


