(UroToday.com) In a Hot Topic session of the Société Internationale D’Urologie (SIU) 2021 annual meeting focused on the role of artificial intelligence (AI) in urology, Dr. Jean-Christophe Bernhard discussed the potential of 3-dimensional (3D) models to enhance the quality of robotic-assisted partial nephrectomy.
By way of introduction, Dr. Bernhard emphasized that there are a number of commercially available 3D modeling software programs which will apply AI to DICOM files. These may allow us to improve our ability to bridge the gap between two-dimensions and three-dimensions. He drew the analogy of a navigation assistant while driving for surgery.
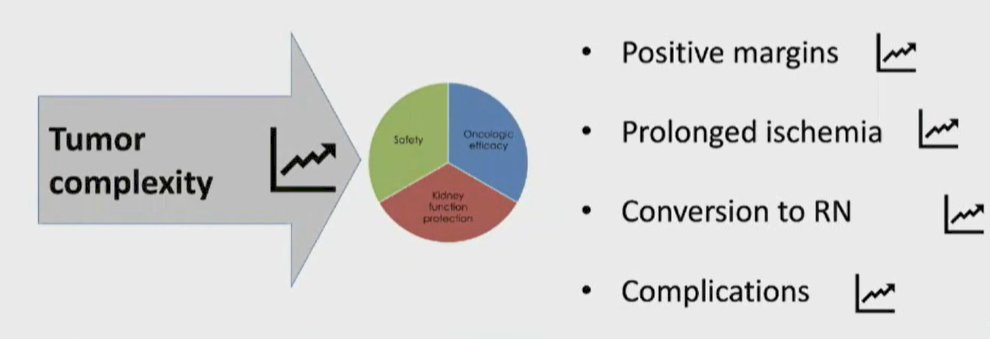
The goal of this approach is to improve the patient-specific anatomic understanding, surgical strategy and planning, anticipation of potential intra-operative pitfalls, outcomes of surgery, and the overall patient experience. He emphasized that the more complex a tumor is, the higher the expected benefit of utilizing these 3D models as these cases are associated with higher rates of positive surgical margins, prolonged ischemia, conversion to radical nephrectomy, and complications.
He emphasized that 3D modeling software will apply AI algorithms for automatic structure recognition and computed tomography (CT) scan segmentation in a semi- or full-automatic fashion. These models will extract information regarding the volume and location of critical structures including the tumor, the vessels, the collecting system, and the normal renal parenchyma. Additionally, these models can predict the anticipated extent of ischemia associated with clamping, with an ability to distinguish various clamping locations including hilar or selective or sub-selective sites.
While these models may be useful pre-operatively, there may also be utilized intra-operatively for navigation (so-called 3D model assisted surgery). In the context of the Da Vinci surgical robotic platform, TilePro may be used for visualization through the console.
Dr. Bernhard then highlighted that 3D virtual imaging of renal tumors may allow for increased accuracy of applying nephrometry scores. This was done as a prospective non-comparative study among 101 patients with a comparative assessment of RENAL and PADUA scores based on the 3D model and 2D CT scan. Additionally, the authors compared the predictive accuracy of scoring based on 3D and 2D assessments on overall and major postoperative complications. Interestingly, the use of 3D models resulted in a significant decrease in the nephrometry score in approximately 50% of patients. However, this 3D model based scoring approach was associated with the best predictive accuracy for both overall and major complications.

Moving from initial prognostication to surgical performance, Dr. Bernhard highlighted a recent randomized trial among patients who received 3D model based surgical planning (n=48) or 2D CT based surgical planning (n=44). Comparing intra-operative surgical outcomes, the authors found decreased estimated blood loss and length of stay for patients whose surgical plan was informed by 3D models. There was no significant difference in terms of operative time or clamp time. However, they did note that the more challenging a case was (as characterized by the nephrometry score), the greater the benefit of the 3D modeling.
Then, moving from pre-operative planning to intra-operative surgical guidance, he highlighted their own UroCCR study 51 which was a retrospective analysis of 645 patients treated by 3 expert surgeons, either with 3D intra-operative guidance or with standard robotic-assisted partial nephrectomy. 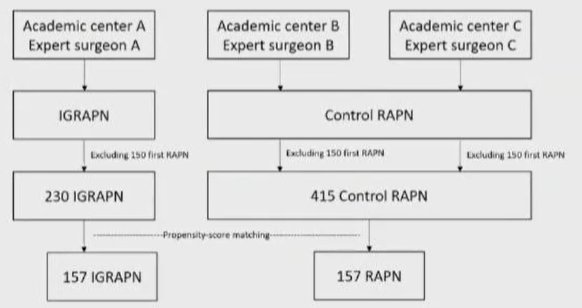
Again assessing intra-operative and post-operative surgical outcomes in a propensity-score matched analysis, the authors found a benefit to the use of the 3D intra-operative guidance with respect to the rate of conversion, the proportion of clampless partial nephrectomy, major complications, transfusion, hospital length of stay, and trifecta though this came at the expense of approximately 50 to 60 minute longer operative time. Assessing functional outcomes, there appeared to be benefits in terms of early renal function recovery, with decreased change in eGFR at discharge and in the first 6 months.
Additionally, moving from virtual 3D models to 3D printed models, Dr. Bernhard emphasized that this may improve personalized patient education. This may allow for an improved patient understanding of renal physiology, kidney anatomy, disease, and tumor characteristics, as well as the surgical procedure.
He, therefore, concluded by emphasizing that there are many ways to use 3D models in robotic-assisted partial nephrectomy, for pre-operative surgical planning, for intra-operative surgical navigation, and for patient counseling. These have particular benefits for ischemia sparing techniques.
Presented by: Jean-Christophe Bernhard, MD, University Hospital of Bordeaux, France


