(UroToday.com) The 2024 Society of Nuclear Medicine & Molecular Imaging (SNMMI) annual meeting featured a session on prostate cancer and a presentation by Dr. Seyed Ali Mirshahvalad discussing 18F-DCFPyL PET/MRI radiomics for intraprostatic prostate cancer detection and metastases prediction using whole-gland segmentation. The aim of this study presented at SNMMI 2024 was to evaluate the diagnostic performance of combined 18F-DCFPyL PET/MRI whole-gland-derived radiomics for detecting clinically significant prostate cancer (ISUP Gleason Grade ≥ 2) and predicting nodal and distant metastases in therapy-naïve patients.
This retrospective analysis included two prospective clinical trials included 103 treatment-naïve men who had confirmed or suspected prostate cancer. Recruited patients had either suspicion of prostate cancer and negative systematic biopsies or clinically discordant low-risk prostate cancer (n = 20), patients being considered for focal therapy (n = 31), or patients with unfavorable intermediate or high-risk prostate cancer (n = 52). All patients were enrolled between 2017 and 2020 and underwent 18F-DCFPyL PET/MRI. Radiomic feature analysis of PET/MRI was obtained using commercial software via the quantitation of various radiomics features based on the spatial arrangement and variation of pixel intensities within a defined volume of interest. Whole-prostate segmentations were performed on each modality separately. On the MRI, whole-gland T2-weighted sequence and whole-gland apparent diffusion coefficient (ADC) map were evaluated: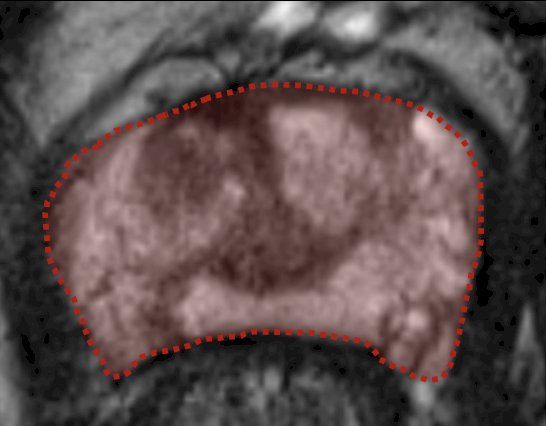
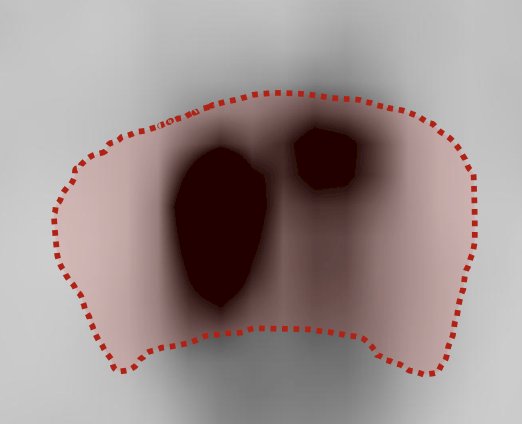
PET volumes of interest were defined based on:
(a) background threshold
(b) peak threshold
(c) threshold at 40%
(d) threshold at 70% of the SUVmax
Since a thresholding method was not available for the MRI component (T2, ADC), the contours for the MRI-derived volumes of interest were performed manually (by an expert specialist in prostate MRI) in a slice-by-slice fashion to cover the entire prostate. The radiomics features, including overall 307 different features, were extracted from the segmented volumes in accordance with the image biomarker standardization initiative guidelines. The reference standard for suspicious prostatic lesions was histopathology (prostate biopsy) in all patients. The highest reported ISUP Gleason Grade was taken into account for each prostate gland. For nodal and distant metastatic assessment, a composite standard of reference was applied for all lesions identified on conventional imaging (CT and bone scan ± mpMRI) or PET and included histopathology, correlative imaging, and clinical/biochemical follow-up. Univariate logistic regression was done to evaluate potential predictors across all calculated features. A predictive modeling approach using multivariable logistic regression with internal cross-validation was performed to calculate estimates and evaluate model performance.
A total of 103 patients with a mean age of 65 years of age, and mean PSA of 23.4 ng/mL were evaluated. Clinically significant prostate cancer was confirmed in 89 (86%) patients, four patients had ISUP Gleason Group 1, and 10 patients were negative for malignancy. Multiple models were built to predict the whole-gland ISUP Gleason Group, including clinical (age and PSA), T2w (MRI-only), 18F-DCFPyL PET (PET-only), clinical + T2w, clinical + PET, T2w + PET (hybrid), and clinical + T2w + PET (full model). The imaging-based hybrid model (T2w + PET) provided the highest AUC (0.89) for the prediction of clinically significant prostate cancer. No statistically significant PET or MRI radiomic feature was found for N-stage prediction. For M staging, the T2w whole-gland radiomic was found to be the best predictive model (AUC 0.94).
Dr. Mirshahvalad concluded this presentation discussing 18F-DCFPyL PET/MRI radiomics for intraprostatic prostate cancer detection and metastases prediction using whole-gland segmentation with the following take-home messages:
- Hybrid PET/MRI radiomics (whole-gland T2w + PET) was the best-performing model to predict clinically significant prostate cancer, outperforming the clinical model
- This indicates a complementary value of the hybrid PET/MRI model for non-invasive clinically significant prostate cancer detection
- Additionally, T2w whole-gland radiomics was able to predict distant metastases in this cohort
- Assessing the prostate gland as a whole can be potentially valuable for further treatment personalization in prostate cancer patients
Presented by: Seyed Ali Mirshahvalad, MD, MPH, FEBNM, Joint Department of Medical Imaging, University of Toronto, Toronto, Ontario, Canada
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Nuclear Medicine & Molecular Imaging (SNMMI) Annual Meeting, Toronto, Ontario, Canada, Sat, June 8 – Tues, June 11, 2024.


