Las Vegas, Nevada (UroToday.com) At the 2019 Society of Nuclear Medicine and Molecular Imaging (SNMMI) Annual Meeting, Dr. Alexander (Sandy) McEwan, gave a comprehensive overview of establishing a practice in systemic radiation therapy. This important field of medicine entails the systemic administration of a targeted radionuclide utilizing short-range beta particles, alpha particles or electron emissions to achieve a clinically important outcome for a patient with primary or metastatic cancer.
In this field, the image is the biomarker enabled to provide specific targeting with a high therapeutic index. The radiopharmaceutical is administered systematically, harboring low toxicity. It is possible to perform retreatment with the radiopharmaceuticals although the imaging associated RECIST criteria are a poor predictor of outcomes. This treatment can be given in various combinations and at the adjuvant setting.
The first documented radiopharmaceutical treatment was given in 1941 with the use of iodine-130 for the indication of hyperthyroidism. Since then, there have been many types of treatments given for a growing number of diseases and organs (Table 1).
Table 1- Abbreviated history of radiopharmaceutical theranostics: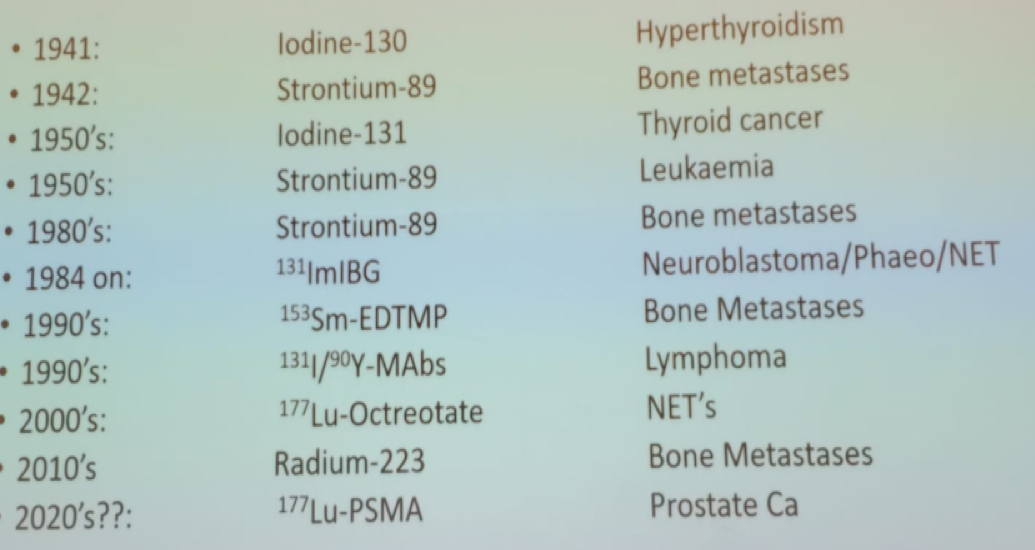
When attempting to establish a theranostics practice there are many barriers and issues that need to be considered and addressed:
1. Socialization - making the therapy accepted and known to all relevant parties
2. Robustness of evidence – attaining the knowledge behind the science of this treatment and being able to present it in an understandable manner to the healthcare professionals and patients
3. Perceived complexification – It is important to make this field appear simple and understandable
4. Administration workflow – the logistics underlying the treatment need to be ascertained and worked in such a way that will allow the treatment process to flow in a continuous manner
5. Education of multiple constituencies, initiation, and continuation of clinical trials to acquire more data and educate the payers as well
6. Training of practitioners from multiple disciplines needs to be performed
Additionally, there is a need to gather and be acquainted with all the relevant data. This includes all relevant clinical, scientific and regulatory data. The nuclear medicine physicians need to engage with the relevant clinical communities, patient advocate communities and hospital administration, as well as access the required funding for this program to initiate and sustain. Lastly, an appropriate infrastructure should be formed for this field of medicine to succeed. This includes trivial factors that are critical, such as finding an appropriate space where the treatment will take place, the required equipment, and the needed personnel.
Dr. McEwan moved on to specifically discuss the specific treatment of Lutetium-Octreotate. Lutetium-177 Octreotate therapy is primarily used to treat people with neuroendocrine tumors (NETs) when other types of treatment, such as surgery or chemotherapy, are not suitable or are ineffective. Lutetium-177 Octreotate is a very specific therapy that can only be used when the tumors express many somatostatin receptors. The common adverse events of this treatment include nausea, carcinoid crisis (rare), hematological adverse events, fatigue, myelodysplasia, and renal/hepatic toxicity.
In a meta-analysis on peptide receptor radionuclide therapy (PRRT) used for NETs1, it was concluded that PRRT appeared to be an acceptable option, which is relatively safe provided a renal protection solution of lysine and arginine amino acids is given to adults with advanced NETs. Metaiodobenzylguanidine (MIBG) is a compound that can be combined with radioactive iodine (I-131) to deliver targeted radiation therapy (I-MIBG). I-MIBG may be an effective therapy for malignant neuroblastoma in pediatric patients, paraganglioma or pheochromocytoma. Hematologic toxicity, severe infections, and secondary malignancies need to be considered when administering these treatments. To date, there is no strong evidence to support that one therapeutic radiopharmaceutical is more effective than others. Lastly, the authors of the meta-analysis concluded that there is a great need for well-designed randomized controlled trials with controlled entry criteria, and this is the most important point.
In a recent large meta-analysis of Lu-177 PRRT for the treatment of NET, 18 studies were included with 1,920 patients2. The pooled disease response rate was shown to be 29.1% with a disease control rate of 74.1%. Despite these promising results, there are still many unanswered questions behind the science of this medical field. These include:
1. What is the correlation between response and disease control?
2. What is the biology of the tumor that responds and those that do not respond to this unique treatment?
3. Radiobiology issues
4. Dosimetry
5. Clarification on the sequencing of treatment
6. Administered doses
Next, Dr. McEwan delved into the topic of engagement with the various populations of interest, including healthcare professionals, patients, hospital administration and funding factors. For other healthcare professionals to recognize and acknowledge the important contribution therapeutic radiopharmaceuticals has to offer, it is important to create a substantial presence of nuclear medicine in the multidisciplinary recurring tumor boards. The nuclear medicine physician needs to convey the advantages and disadvantages of this treatment, when it is indicated and when it is not. Through constant engagements and significant presence, rewarding partnerships can be established. By establishing a theranostic practice, it is important to recognize that the nuclear medicine physician will by implication become a clinical practitioner. If nuclear medicine physicians provide this unique and important systemic anti-cancer therapy, they need to be involved, take charge and lead the way.
Additionally, engaging patient advocacy groups and patient support groups is essential. Patients have been waiting a long time for this type of treatment and are eager to learn and know more. It is also necessary to speak and engage with the nursing services to get them on board as soon as possible.
The multidisciplinary neuroendocrine board should consist of a nuclear medicine physician, or as Dr. McEwan calls him/her the “nuclear oncologist”, the endocrine surgeon, medical oncologist, radiation oncologist, endocrinologist, radiologist, pathologist, tumor group nurse coordinator/navigator, and practice nurse.
Next, the processes, workflow, and educations regarding the novel treatment were discussed. The patient flow, how to accept new patients, the referral process etc. need to be configured for this treatment. Doctors need to ascertain how patients are going to be followed and at what capacity. Lastly, reporting of all these clinical visits need to be performed as soon as possible. When establishing the education part of this treatment, it is important to make sure patients receive information through accessible means such as information sheets and online data. Lastly, each patient needs to receive a radiation therapy letter explaining their type of treatment and its immediate implications, especially for travel. For all patients being treated and followed in the clinic, it is imperative to collect quality of life data through using patient questionnaires, diaries, side effect profiles, toxicity profiles, and treatment schedules. It is also mandatory that the practitioner interacts with the administration and conveys to them the advantages of having this treatment available. Other healthcare professionals need to recognize it and support it. Resident programs should include rotations and data acquisition in theranostics.
The last important topic discussed for establishing a successful practice in the theranostic practice is the infrastructure that is required. Adequate space is needed (either a chemotherapy daycare of individual rooms) with consult rooms, family area, private bathroom, nursing stations, technologist area, space for pumps, poles, and monitoring equipment.
The therapeutic nuclear medicine advanced associate curriculum needs:
1. Increased base knowledge in oncology practice
2. Increased base knowledge in dosimetry
3. Radiobiology
4. Clinical trials training
5. Quality of life assessment
6. Communication with the relevant industry
Dr. McEwan concluded his comprehensive talk stating that we need to develop an “R” RECIST criteria for systematically administered radiopharmaceuticals. Lastly, more data is required from large prospective trials.
Presented by: Alexander (Sandy) McEwan, MD, Professor in the Department of Radiology & Diagnostic Imaging, Faculty of Medicine and Dentistry, University of Alberta, Alberta, Canada
Written by: Hanan Goldberg, MD, Urology Department, SUNY Upstate Medical University, Syracuse, New York, USA, Twitter: @GoldbergHanan at the 2019 SNMMI Therapeutics Conference: Therapies, Theranostics, and Building Your Radionuclide Clinical Practice, October 25-27, 2019 in Las Vegas, Nevada
References:
1. Gulenchyn KY, Yao X, Asa SL, Singh S, Law C. Radionuclide therapy in neuroendocrine tumours: a systematic review. Clinical oncology (Royal College of Radiologists (Great Britain)) 2012; 24(4): 294-308.
2. Saravana-Bawan B, Bajwa A, Paterson J, McEwan AJB, McMullen TPW. Efficacy of 177Lu Peptide Receptor Radionuclide Therapy for the Treatment of Neuroendocrine Tumors: A Meta-analysis. Clinical nuclear medicine 2019; 44(9): 719-27.


