There were 420 patients enrolled in this study and registered in the prospective BPH registry from September 2016 to November 2018. Evaluation before treatment included pre-operative transrectal ultrasonography (TRUS) and urodynamic studies (UDS). Questionnaires, including the International prostate symptoms score (IPSS), overactive bladder symptom score (OABSS), Nocturia Quality of Life (N-QOL) and Pittsburgh sleep quality index in Korean (PSQI-K), frequency volume chart (FVC), uroflowmetry, and postvoid residual volume were taken pre-operatively as well as post-operatively at two weeks, three months and six months. The relationship between the parameters of nocturia and pre-operative clinical parameters was examined.
Post-operative Q-max and PVR of 420 patients (mean age 68.4±7.7 years, SD) were significantly improved (p<0.001). The mean frequency of nocturnal voiding was measured pre-operatively and post-operatively at two weeks, three months and six months. In IPSS, these were 2.3 (±1.4), 2.1 (±1.3), 1.6 (±1.0) and 1.4 (±0.8) (p<0.001), pre-operative and two weeks, three months and six months postoperatively, respectively. In OABSS they were 2.0 (±1.1), 1.9 (±1.1), 1.5 (±0.9) and 1.3 (±0.8) (p<0.001), showing a similar decrease in the frequency of nocturnal voiding. With FVC, they were 1.4 (±0.9), 1.7 (±1.3), 1.2 (±0.9), 1.1 (±0.8) (p<0.001). The total volume of nocturnal urine recorded in FVC significantly decreased from 551.9 (±274.6) mL before surgery to 518.4 (±216.2) mL at the post-operative six months (p=0.031). The maximal voided volume also significantly increased from 356.2 (±175.6) mL before surgery to 390.3 (±128.3) mL at postoperative six months (p<0.001). Significant reduction in the frequency of nocturnal voiding at postoperative six months was observed in patients with a greater first desire to void volume measured in the pre-operative UDS, the greater maximal voided volume and less nocturia volume recorded in the pre-operative FVC (p<0.001). A decrease in the frequency of nocturnal voiding was significantly associated with an increase in maximal voided volume (r=-0.271, p=0.002) and a decrease in the volume of nocturnal urine (r=0.462, p<0.001).
The authors concluded that the frequency of nocturnal voiding after HoLEP operation was significantly lower compared to the pre-operative period. This reduction in the frequency of nocturnal voiding is thought to have significantly attributed to the increase in the maximal voided volume recorded in FVC.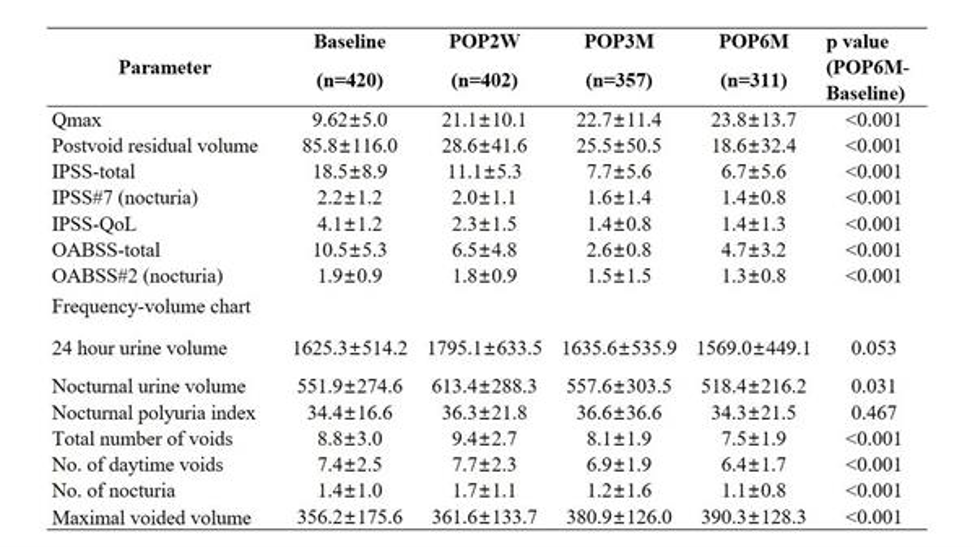
Presented by: Hwanik Kim, MD, Seoul National University Hospital, Seoul, South Korea
Written by: Bilal Farhan, MD, Assistant Professor, Division of Urology, University of Texas, Medical Branch, Texas; Twitter: @BilalfarhanMD, at the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting, SUFU 2020, February 25 - 29, 2020, Scottsdale, AZ


