Women with SUI, naïve for SUI surgery, candidate to MUS were evaluated. Exclusion criteria were previous SUI surgery, associated pelvic organ prolapse, predominant urge urinary incontinence, previous pelvic surgery and/or radiotherapy, neurologic diseases. The population was divided into patients with DU (Group A) and women without DU as a control group (Group B). All patients underwent pre-operative urodynamics (UDS). DU was defined by the stricter criteria reported in the literature: Pdet/Qmax < 10 cmH2O and Qmax < 12 ml/sec (Gotoh M et al., Int J Urol 2006). Preoperative and 1-year follow-up evaluation included: free uroflowmetry (UFM), post-void residual urine (PVR), PVR-ratio (PVR-R: the ratio between bladder volume and PVR), the International Continence Index Questionnaire Urinary Female LUTS (ICIQ-FLUTS). Post-operative urinary retention (POUR) was defined as: PVR ³200 ml in > 2 evaluations.
Both the Groups had 34 patients, with similar demographic characteristics. POUR was detected in 35.3% (12/34) in Group A vs 8.8% (3/34) in Group B and resolved in 3-30 days and in 7-20 days respectively. In both groups, 5.9% (2/34) had a tape incision within one month of the first surgery. At 1-year follow-up SUI recurrence and de-novo urgency were 5.9% and 11.8% in both groups respectively. Table 1 shows outcomes at 1-year follow-up.
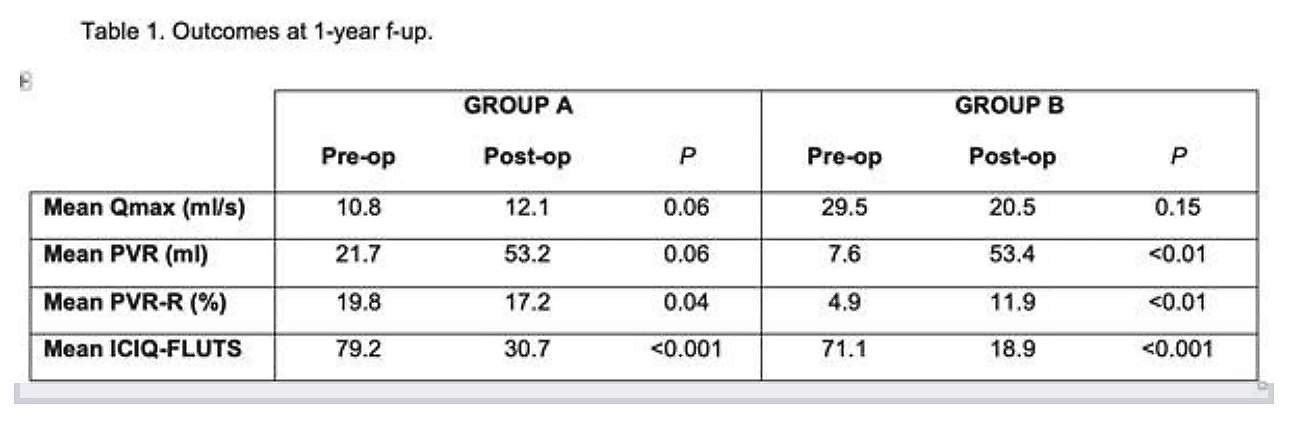
Preoperative urodynamics is useful to select patients with DU who are at higher risk of transient POUR and may need tailored counseling and preoperative teaching with intermittent catheterization. Thus, preoperative urodynamics diagnosis of DU may impact pre and postoperative DU did not affect the cure rate in women treated with MUS for SUI. Women with DU had four times higher early transient POUR with the same rate of resolution of the no-DU group. DU did not affect the re-operation rate for POUR.
Presented by: Matteo Balzarro, MD1
Co-Authors: Emanuele Rubilotta, MD1, Antonio D'Amico, MD1, Ester Illiano, MD2, Vito Mancini, MD3, Elisabetta Costantini, MD2, Frank Van der Aa, MD, PhD4, Alessandro Antonelli, MD1
1. Department of Urology, AOUI Verona, Verona, Italy
2. Department of Andrology and Urogynecological Clinic, Santa Maria Terni Hospital, University of Perugia, Perugia, Italy
3. Department of Urology and Renal Transplant, University of Foggia, Foggia, Italy
4. Department of Urology, UZ Leuven, Belgium
Written by: Bilal Farhan, MD, Assistant Professor, Division of Urology, University of Texas, Medical Branch, Texas; @BilalfarhanMD at the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting, SUFU 2020, February 25 - February 29, 2020, Scottsdale, Arizona


