Washington, DC (UroToday.com) Continuing the plenary session on nonmuscle invasive bladder cancer (NMIBC) at this year’s Society of Urologic Oncology Annual Meeting, Dr. Mark Soloway presented on the management of small, low grade bladder cancer recurrences.
His thesis was that the traditional teaching to “remove clinically localized GU cancer when diagnosed” was not relevant in this clinical scenario. To support this, he began by citing evidence and guidelines supporting conservative management approaches in patients with low risk prostate cancer and small renal masses. Thus, he suggested a risk-adapted management approach for patients with low-grade Ta bladder tumors. This is largely driven by the underlying disease biology and epidemiology:
- 60% of bladder tumors present as TaLG
- TaLG has a high recurrence rate (30-60%)
- These have an excellent prognosis without evidence of metastatic behaviour or progression to muscle invasive disease (0.8%)
He argued that urologists could reliably identify patients with low grade disease cystoscopically. Supporting this, he cited data from Dr. Herr which asked physicians to predict whether a tumor was TaLG, TaHG, or T1HG based on endoscopic appearance in 150 consecutive patients with recurrent papillary tumors with a history of Ta or T1 disease. This study showed good concordance between visual assessment and histologic assessment: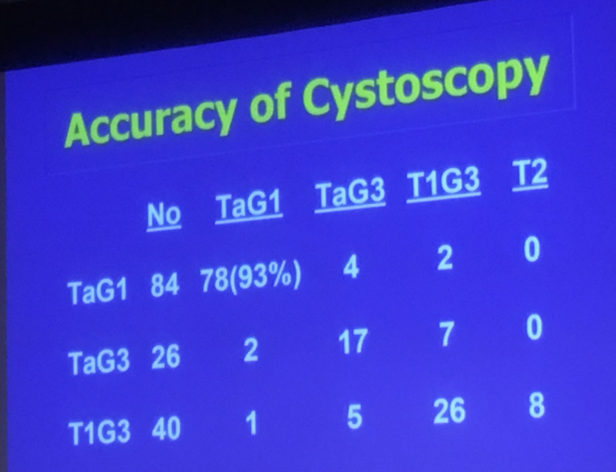
Observation of patients with low grade, superficial disease offers many potential benefits:
- Decrease visits to the OR
- Avoid repeated bladder trauma
- Reduce morbidity of TURBT and anesthesia
- Cost saving
Dr. Soloway suggested that such an approach would not be suitable for patients with gross hematuria, significant tumor growth, or a change in appearance suggesting more aggressive disease. Instead, these patients would warrant formal operative resection.
He then highlighted data that he published in 2003 demonstrating that, among 32 patients with a history of Ta or T1 bladder tumors, none progressed to muscle invasive disease when small, superficial recurrences were managed conservatively. A number of other groups subsequently validated these results.
Stopping short of an entirely conservative approach, Dr. Soloway suggested that office-based cautery provided an alternative which removes tumor with minimal discomfort, significant cost savings, and increased convenience for both patients and physicians. He presented data to support the use of laser resection in this setting which offered significant cost savings.
He highlighted that this approach is recommended in both AUA/SUO and EAU guidelines and closed by suggesting that management of patients with low-grade Ta bladder tumors should focus on deintensification to reduce costs and the burden of treatment without compromising oncologic outcomes.
Presented by: Mark Soloway, MD, FACS, Chief of Urologic Oncology, Memorial Healthcare SystemWritten by: Christopher JD Wallis, MD, PhD, Urologic Oncology Fellow and Instructor in Urology at Vanderbilt University Medical Center at the 20th Annual Meeting of the Society of Urologic Oncology (SUO), December 4 - 6, 2019, Washington, DC


