Changes in reimbursement may affect physician behavior and patient counseling. Prior evidence has suggested that participation in Accountable Care Organizations (ACOs) may improve the value of health care delivery by improving quality and reducing cost. Thus far, in aggregate, the evidence is that ACO participation has had small changes in PSA screening. However, this work has not accounted for variation between individual ACOs. To this end, in a poster presentation today at the Society of Urologic Oncology meeting, Dr. Luckenbaugh and colleagues assessed the variation in prostate cancer screening using PSA testing among individual Medicare Shared Savings Program ACOs.
The authors performed a retrospective cohort study utilizing national Medicare data from 2007 to 2017 with the goal of characterizing rates of change in PSA testing across ACOs. To assess for the appropriateness of PSA testing, the authors stratified their analysis for men aged greater than or equal to 75 years versus less than 75 years of age and stratified their analysis according to predicted five-year survival (high vs low).
Among 21,050,902 identified Medicare beneficiaries who were attributed to ACOs, the authors identified an overall reduction in PSA testing over time (mean rate of change -24.5%, range -70.5% to +72.2%). However, there was significant variation between ACOs as demonstrated in this figure:
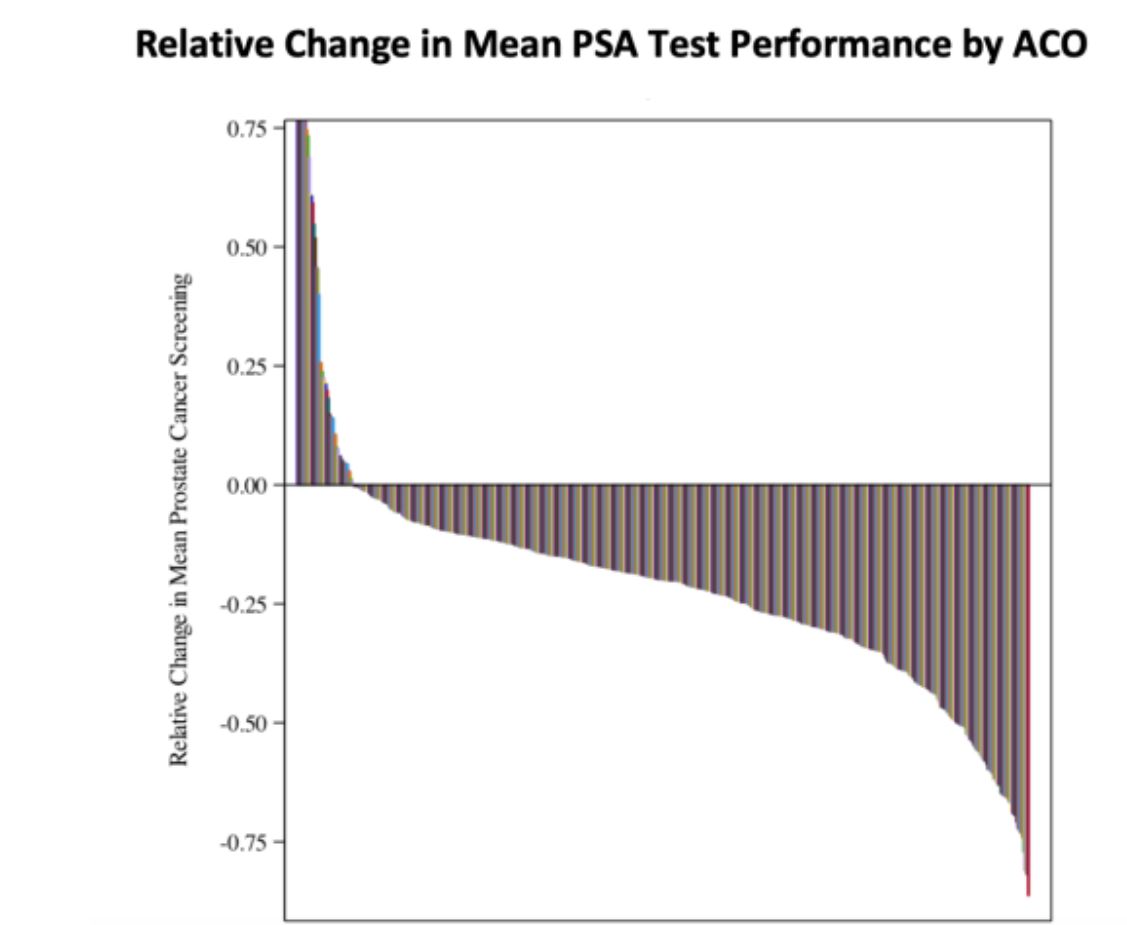
There was an overall greater reduction in PSA screening among men older than 75 years (mean 30%) as compared to those aged less than 75 years (mean 14%, p<0.0001). In a similar manner, there were greater decreases in men with low rather than high expected 5-year survival (41% versus 11%, p<0.0001).
These data demonstrate that there is wide variation between ACOs, and offer a significant opportunity for improvements in the quality of care. The across the board reductions in PSA testing suggest that ACOs are reducing PSA screening even among the men who are most likely to benefit from PSA screening.
Presented by: Amy N. Luckenbaugh, MD, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, Tennesee
Written by: Christopher J.D. Wallis, MD, PhD, FRCSC Contact: @WallisCJD on Twitter at the 20th Annual Meeting of the Society of Urologic Oncology (SUO), December 4 - 6, 2019, Washington, DC
Written by: Christopher J.D. Wallis, MD, PhD, FRCSC Contact: @WallisCJD on Twitter at the 20th Annual Meeting of the Society of Urologic Oncology (SUO), December 4 - 6, 2019, Washington, DC


