- The seed and soil hypothesis - metastatic tumor cells will metastasize to a site where the local microenvironment is favorable, just like a seed will only grow if it lands on fertile soil
- Abscopal effect
- Immune modulation
- Topographic
The nomenclature and staging of metastatic disease have changed over the years.
The rationale for surgery of nodal metastatic disease stems from several factors. First, limited nodal metastatic disease may be cured with surgery (+/-chemotherapy). Surgery in the setting of clinically node-positive disease should be reserved for only those with complete clinical response. However, it is known that only those with a complete pathological response will experience improved survival. Lastly, there could be instances where consolidative surgery in the setting of systemic disease is the only chance for a possible cure.
As previously mentioned, the nomenclature and staging have changed over the years. Between 2003-2010 common iliac node disease was considered metastatic disease. When looking at retrospective population-based data, patients who underwent neoadjuvant chemotherapy and radical cystectomy had a 13% pT0 result, 68% had >=pT2, and all had pN1-3 M0 disease. Their median overall survival was 20 months, with 5-year overall survival of 31%1 (figure 1).
In another National Cancer Database (NCDB) analysis of metastatic bladder cancer patients with extra pelvic nodes, bone, and visceral disease, conservative local treatment was compared to high-intensity local treatment (figure 2). The median overall survival was 15 vs. 10 months, favoring the high-intensity local treatment.2
Figure 1 – Overall survival according to treatment scenario:

Figure 2 – The inverse probability of treatment weighting –adjusted Kaplan-Meier analysis of overall survival in patients who received multiagent systemic chemotherapy combined with high intensity versus conservative local treatment for metastatic urothelial carcinoma of the bladder:2

It is important to recognize that in some patients, cancer can be cured with the systemic disease only, while some remain incurable even with the addition of surgery. Identifying who falls in the gap is the key.
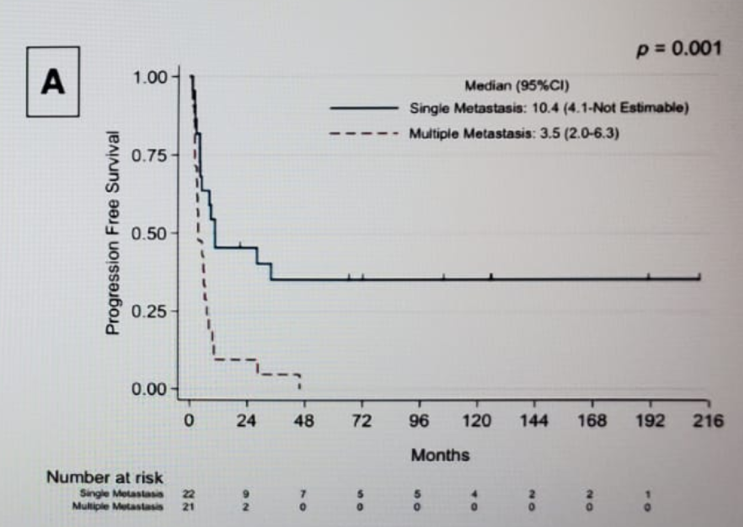
It is possible to refine the selection of metastatic patients undergoing surgery, and there is a clinical rationale for this. In a study assessing 43 patients with metastatic bladder cancer, the majority of which were in the retroperitoneal area, those with a solitary site of disease demonstrated improved survival3 (Figure 3).
Figure 3 – Progression-free survival in single metastasis vs. multiple metastasis:3
There is currently ongoing work that is using genomic expression of different genes to see if this can help us make the right decision about which patients should undergo surgery and If this would improve their prognosis.
These findings highlight the need for a prospective trial to determine whether there is a benefit of multimodal therapy for patients with metastatic urothelial cancer. We need to understand the optimal timing of surgery relative to chemotherapy and factors that determine patient selection. There is also a need to characterize the impact of surgery on patient quality of life. There is a current Southwest Oncology Group that planned a prospective randomized trial to address the role of surgical consolidation in de novo node-positive metastatic bladder cancer (Figure 4). We eagerly await the results of this trial to help guide treatment for these poor-prognosis patients.
Figure 4 – Planned prospective randomized trial:

Presented by: Neema Navai, MD, MD Anderson Cancer Center, Bellaire, TX
Written by: Hanan Goldberg, MD, MSc, Assistant Professor, Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA @GoldbergHanan at the 2020 Society of Urologic Oncology Annual Meeting – December 2-5, 2020 – Washington, DC
References:
- Galsky MD, Stensland KD, Moshier E, et al. Effectiveness of Adjuvant Chemotherapy for Locally Advanced Bladder Cancer. Journal of Clinical Oncology 2016; 34(8): 825-32.
- Seisen T, Sun M, Leow JJ, et al. Efficacy of High-Intensity Local Treatment for Metastatic Urothelial Carcinoma of the Bladder: A Propensity Score-Weighted Analysis From the National Cancer Data Base. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2016; 34(29): 3529-36.
- Li R, Kukreja JEB, Seif MA, et al. The role of metastatic burden in cytoreductive/consolidative radical cystectomy. World journal of urology 2019; 37(12): 2691-8.
SUO 2020: Management of “Node Only” M1 Metastatic Bladder Cancer- Against Surgery


