(UroToday.com) In a plenary session of the Society of Urologic Oncology Annual Meeting focused on transperineal prostate biopsy, Dr. Timothy McClure discussed considerations regarding local and regional anesthesia for transperineal and transrectal prostate biopsy, with a focus on the anatomic and neuro-anatomy of the pelvis.
To provide context, Dr. McClure emphasized the growing interest in transperineal biopsy. This is driven in large part by the decreased risk of infectious complications and improved antibiotic stewardship. However, transperineal biopsy is associated with an increased need for analgesia compared to a transrectal approach.
He emphasized the importance of considering three regions for anesthesia when performing prostate biopsy: the anal/rectal region, the prostate region, and the skin and perineum.
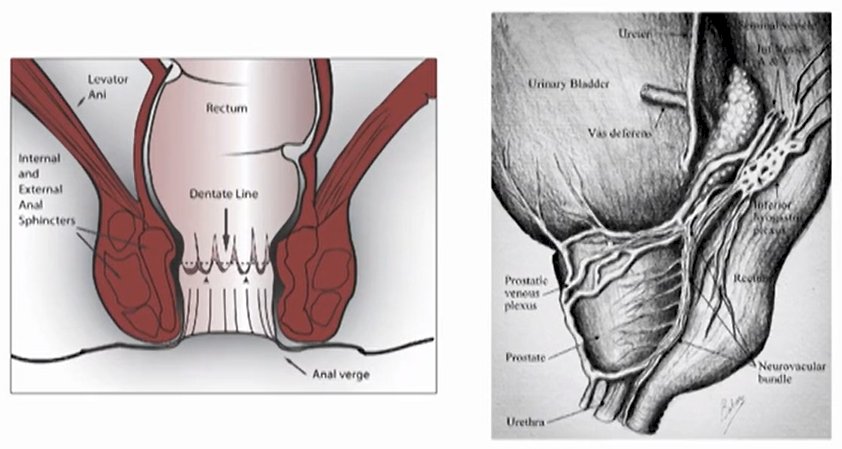
With respect to the anal/rectal region, he emphasized the importance of the dentate line: there is somatic innervation below the dentate line from the pudendal nerve. As a result, there is pain, temperature, and touch sensation. In contrast, above the dentate line, there is only sympathetic and parasympathetic innervation which leads to distension sensation but not the perception of pain. These distinctions are particularly important when considering apical blocks and biopsies.
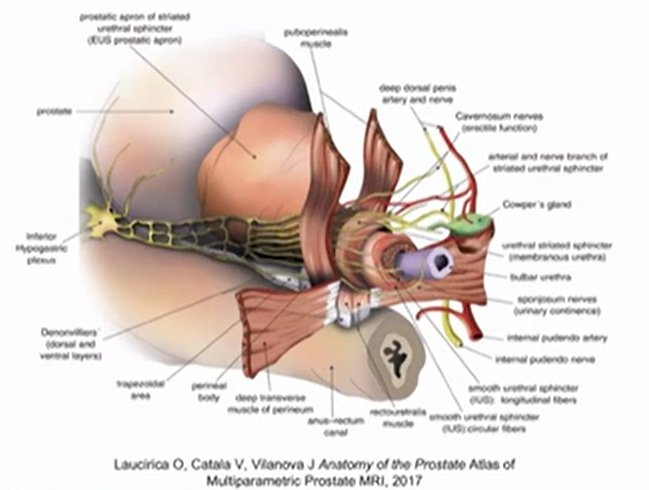
Dr. McClure then highlighted that the prostate is innervated based on the pelvic plexus (inferior hypogastric plexus) which is fed from the S2-4 nerve roots. These nerves converge at the seminal vesicles. Thus, prostate blocks have typically focused on the plexus, the confluence of the nerves at the seminal vesicles, or the prostate apex.
With regards to the perineum, Dr. McClure emphasized that “this is a different beast” as the nerves, particularly the pudendal and perineal nerves, and their branches, provide innervation. For a transperineal approach, anesthesia of these nerves is critical to procedural success.
Overall, he emphasized that there are a variety of techniques. Considering the need for anesthesia of the rectum, Dr. McClure highlighted that this may be relatively easily accomplished with intra-rectal local anesthesia. In terms of the prostate, there are a variety of approaches including a pelvic plexus block, a periprostatic nerve block, or a periapical triangle block. With respect to the prostate and perineum, when considering a transperineal approach, we can consider branches of the perineal nerve block and a pudendal nerve block. Additionally, for a transperineal biopsy, we need to consider anesthesia of the skin.
A pelvic plexus block may be performed by focusing delivery of the local anesthetic at the tip of the seminal vesicle. In contrast, a periprostatic nerve block occurs at the confluence of the pelvic plexus nerves, at the junction of the seminal vesicle and the prostate. The periapical triangle block, as the name suggests, relies on placing an anesthetic at the apex of the relevant nerves and allowing it to act in a retrograde fashion to anesthetize the prostate. The periapical triangle is bounded by the levator ani and the rhabdosphincter.
More recently, it was recognized that there may be considerable pelvic floor and perineal pain following periapical triangle blocks for transperineal biopsy. Thus, Wang et al. proposed the branches of the perineal nerve block to cover the more superficial areas of innervation. They, therefore, attempted anesthesia of the region in which the superficial and deep nerves separate to provide an effect on both. Anatomically, this correlates with where the levator ani crosses the apex of the prostate.
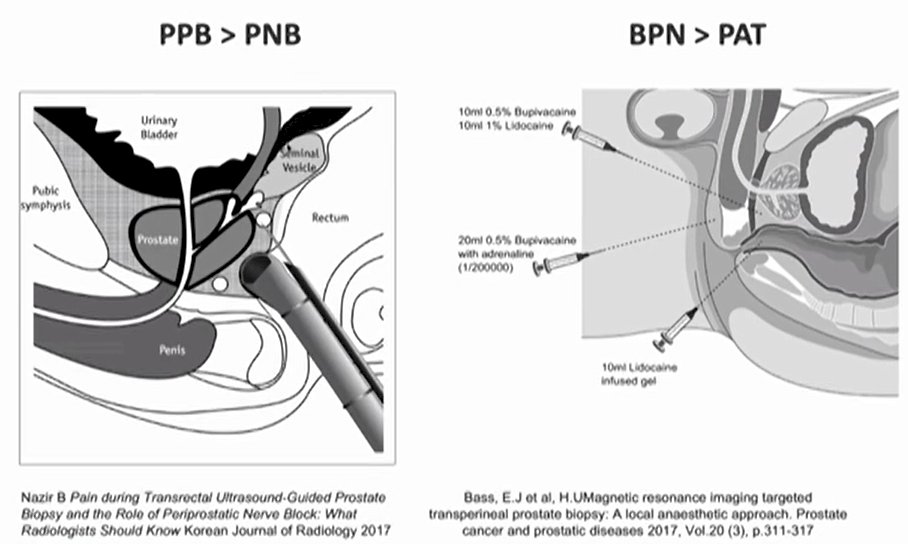
In terms of the transrectal approach, he suggested that a pelvic plexus block provides better anesthesia than a periprostatic nerve block. For patients undergoing transperineal biopsy, a branches of the perineal nerve block may have better pain control. However, the difference, anatomically, is relatively limited and Dr. McClure suggested that you can do both nearly simultaneously.


