(UroToday.com) In a plenary session of the Society of Urologic Oncology Annual Meeting focused on transperineal prostate biopsy, Dr. Edward Schaeffer began the session by discussing strategies to mitigate infections among patients undergoing prostate biopsy.
Dr. Schaeffer began by highlighting that there is “a simple formula… to reduce infectious complications” including provisioning the use of biopsy in appropriate patients, billing infection-causing bacteria that may be introduced during the procedure, and avoiding the introduction of said bacteria during the procedure.
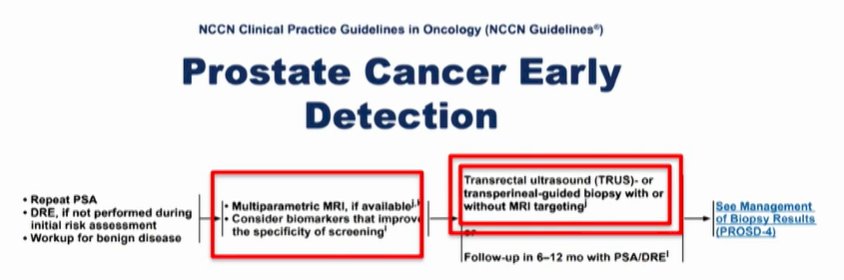
Addressing the first of these, he emphasized the importance of biopsying the appropriate patient. Doing so reduces the total number of biopsies performed and will reduce the burden of biopsy-related complications. To this end, he highlighted data from many trials emphasizing the value of multiparametric MRI (based on data from studies including PRECISION and PRECISE), along with potentially the role for molecular biomarkers, to improve the specificity of screening. He emphasized that the introduction of these tools into the diagnostic algorithm will dramatically decrease the number of biopsies performed without leading to a meaningful misrate for clinically significant disease.
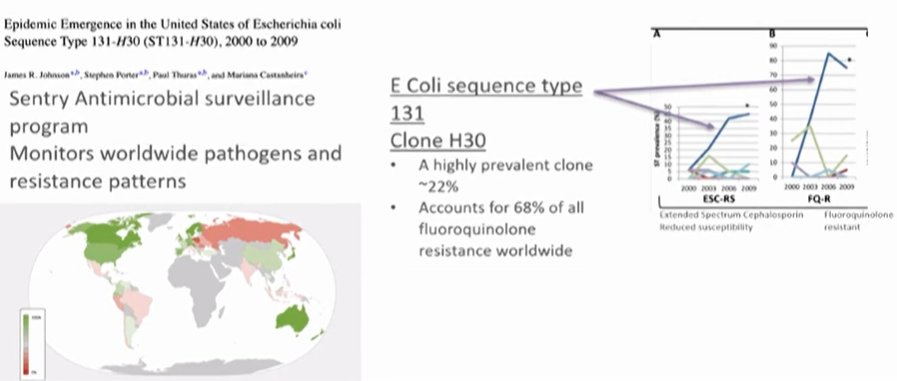
Second, he emphasized that we may kill infection-causing bacteria that are introduced during biopsy. To this end, he cited data published from Dr. Terris more than twenty years ago which showed that, following transrectal ultrasound-guided (TRUS) prostate biopsy, bacteria are found in the prostate tissue approximately 50% of the time, in urine 44% of the time, and in the blood approximately 16% of the time. At the time of publication, infectious complication rates were low despite this due to antibiotic sensitivity. However, beginning in the early 2000s, there was evidence of hospitalizations due to infectious complications following prostate biopsy, driven by the rapid emergency of multi-drug resistant bacteria. This is driven in large part by a highly prevalent strain of E. coli which accounts for nearly 70% of all fluoroquinolone resistance. It emerged in the early 2000s, around when infectious complications were noted.
Dr. Schaeffer then addressed how we may manage these potential resistant organisms. In general, he cited two potential approaches: use of a “bigger hammer” or a “smarter carpenter”. In the first example, he noted the principle of augmented prophylaxis whereas, for the second, he emphasized the potential for targeted prophylaxis. He highlighted the Northwestern protocol which relies on a rectal swab to direct antimicrobial prophylaxis.
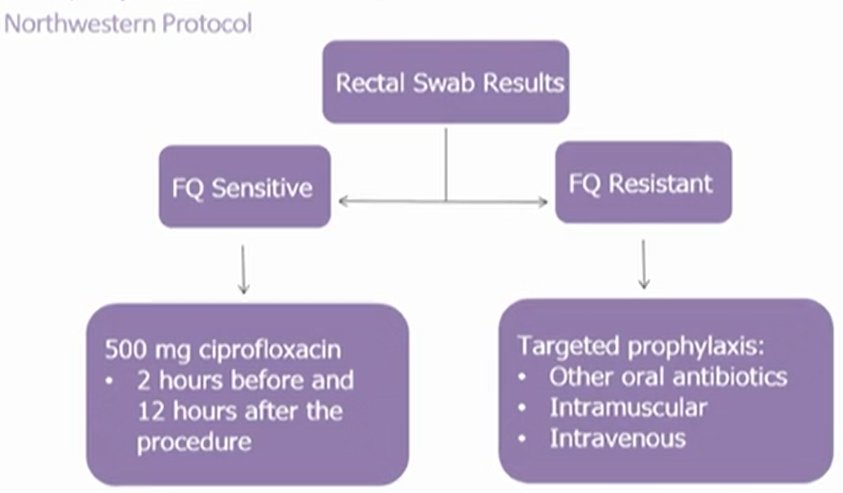
He emphasized that approximately 4 of 5 men will be fluoroquinolone sensitive. The use of this approach, with targeted prophylaxis, significantly reduced infectious complications (from 2.6% to 0% in this cohort). Notably, 38 men were needed to undergo rectal swabs to prevent one complication. This was substantially more cost-effective than the management of infectious complications when they arose (overall cost for 100 men: $1346 v 5598). This approach has been taken up by the Michigan Urologic Surgical Improvement Collaborative. Both a directed prophylaxis approach and an augmented approach were effective at reducing infectious complications and hospitalizations.
Dr. Schaeffer further emphasized that there are additional efforts that may be utilized to reduce infectious complications. These include reducing the bacterial load in the rectal vault. One such approach is the use of povidone-iodine prophylactic cleaning of the rectum prior to biopsy. In a randomized trial, this decreased infectious complications by approximately 50%. However, he emphasized that, despite benefits, studies have generally not found statistically risk reductions. Thus, this is typically not clinically adopted. An alternative is formalin disinfection of the biopsy needle.
However, Dr. Schaeffer posed the question “is transrectal prostate biopsy foundationally flawed due to infection risks?”. This leads to the third approach, where we avoid introducing bacteria during the course of biopsy. This may be accomplished with the use of transperineal biopsy, performed either based on a template or free-hand (using either a free-needle of a registration approach. Dr. Schaeffer noted that transperineal needle biopsy was first utilized in 1922, well before the first transrectal prostate biopsy. Across many studies, rates of infectious complications are low following transperineal prostate biopsy, though many of the early studies used antibiotic prophylaxis.
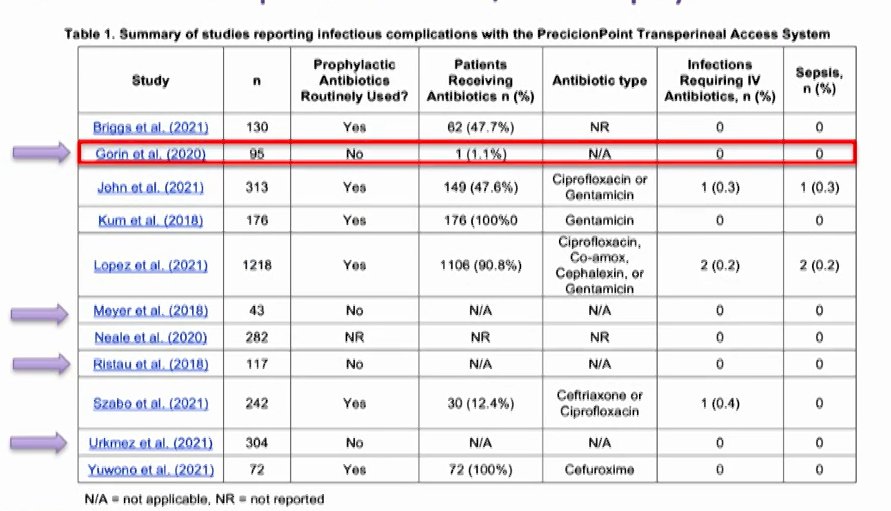
Dr. Schaeffer concluded by highlighting that there is “a simple formula… to reduce infectious complications” including provisioning the use of biopsy in appropriate patients, billing infection-causing bacteria that may be introduced during the procedure, and avoiding the introduction of said bacteria during the procedure with a transperineal approach with skin prep alone. A prospective trial is currently examining the role of transperineal biopsy.
Presented by: Edward M. Schaeffer, MD, PhD, Northwestern University Feinberg School of Medicine


