(UroToday.com) The 2023 Society of Urologic Oncology (SUO) annual meeting held in Washington, D.C. between November 28th and December 1st, 2023, was host to a prostate cancer course. Dr. Jim Hu discussed the recent advances in robotic prostatectomy, highlighting the following:
- Advances in robotic prostatectomy lengths of stay and adverse events
- Pelvic fascia sparing trade-offs
- Bipolar pedicles to increase surgeon autonomy
- Deep leaning nerve-sparing assessment
- Single port radical prostatectomy trade-offs
- PSMA-targeted visualization during robotic radical prostatectomy
- Comparative effectiveness versus competing treatments
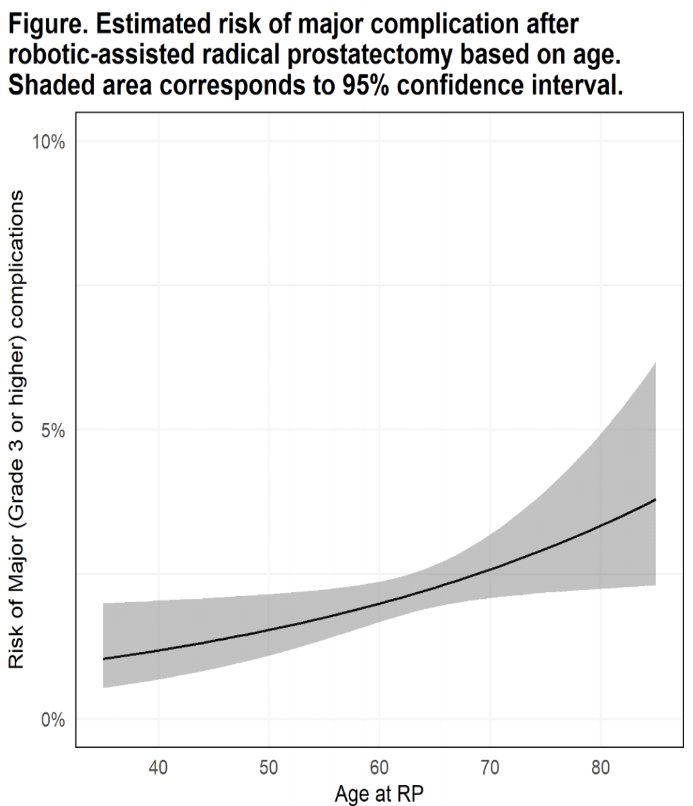
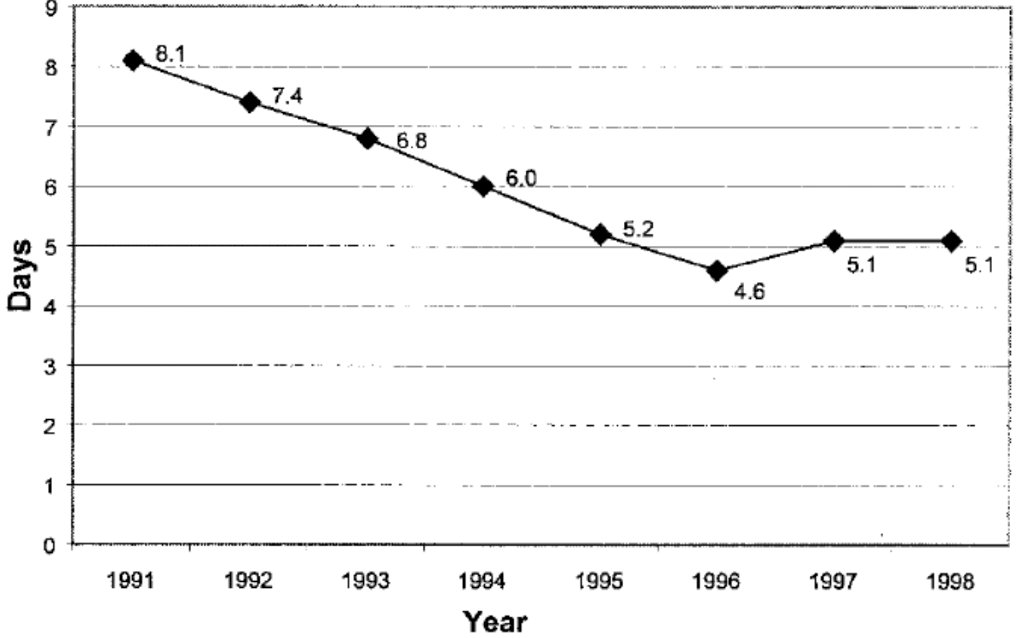
Dr. Hu began by noting that we did not observe significant improvements in post-operative outcomes following radical prostatectomy in the 1990s. There appeared to be a plateau in surgical innovation, and, significantly, post-operative outcomes appeared to be worse in older patients, with many such patients deemed unfit for surgery as a result.1 But did the introduction of robotic-assisted laparoscopic radical prostatectomy (RALP) render these age-related disparities obsolete? Dr. Hu and colleagues performed a retrospective multi-center study from Weill-Cornell NYP (n=588), Georgetown (n=320), and Memorial Sloan Kettering (n=6632) that aimed to evaluate the association between older age and risk of post-operative complications. While the risk of grade ≥3 adverse events following RALPs increased with age (50s: 1.5%, 60s: 2%, 70s: 2.6%), the absolute difference was not clinically meaningful and the age-related disparities were significantly lower compared to those observed in the open series.2
Another important shortcoming of open radical prostatectomy that has been ameliorated by robotic approaches has been the hospital length of stay. In the 1990’s, the average hospital length of stay ranged between four and eight days.1
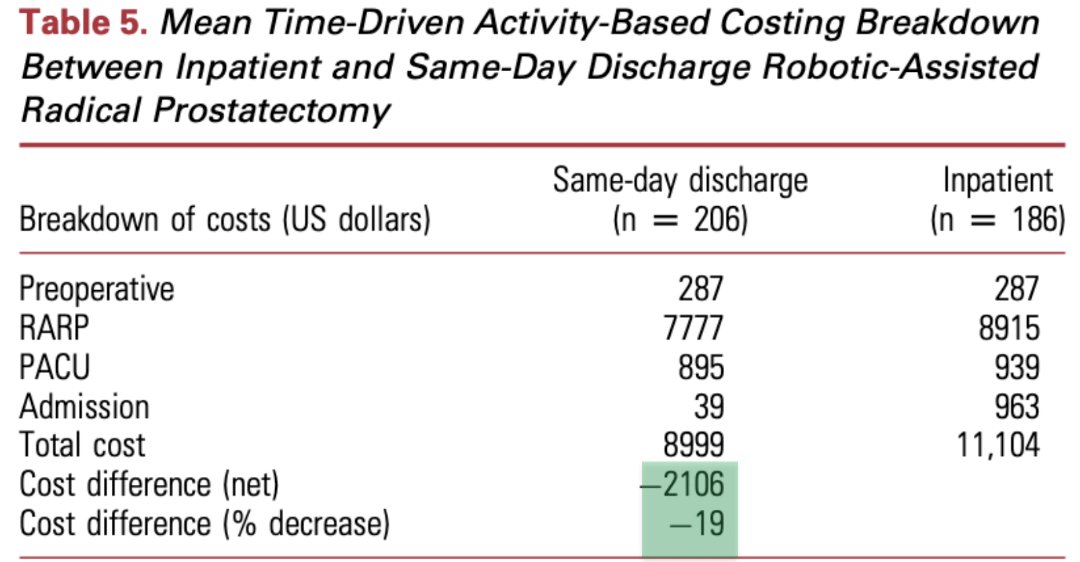
This is in stark contrast to 2023, whereby many well-selected patients are being discharged the same day following an outpatient RALP. In addition to obvious benefits, such as decreasing the hospital’s inpatient admission burden and improving patient satisfaction/convenience, this approach has been shown to decrease net cost by over $2,000 USD, corresponding to a 19% relative decrease in overall costs.2
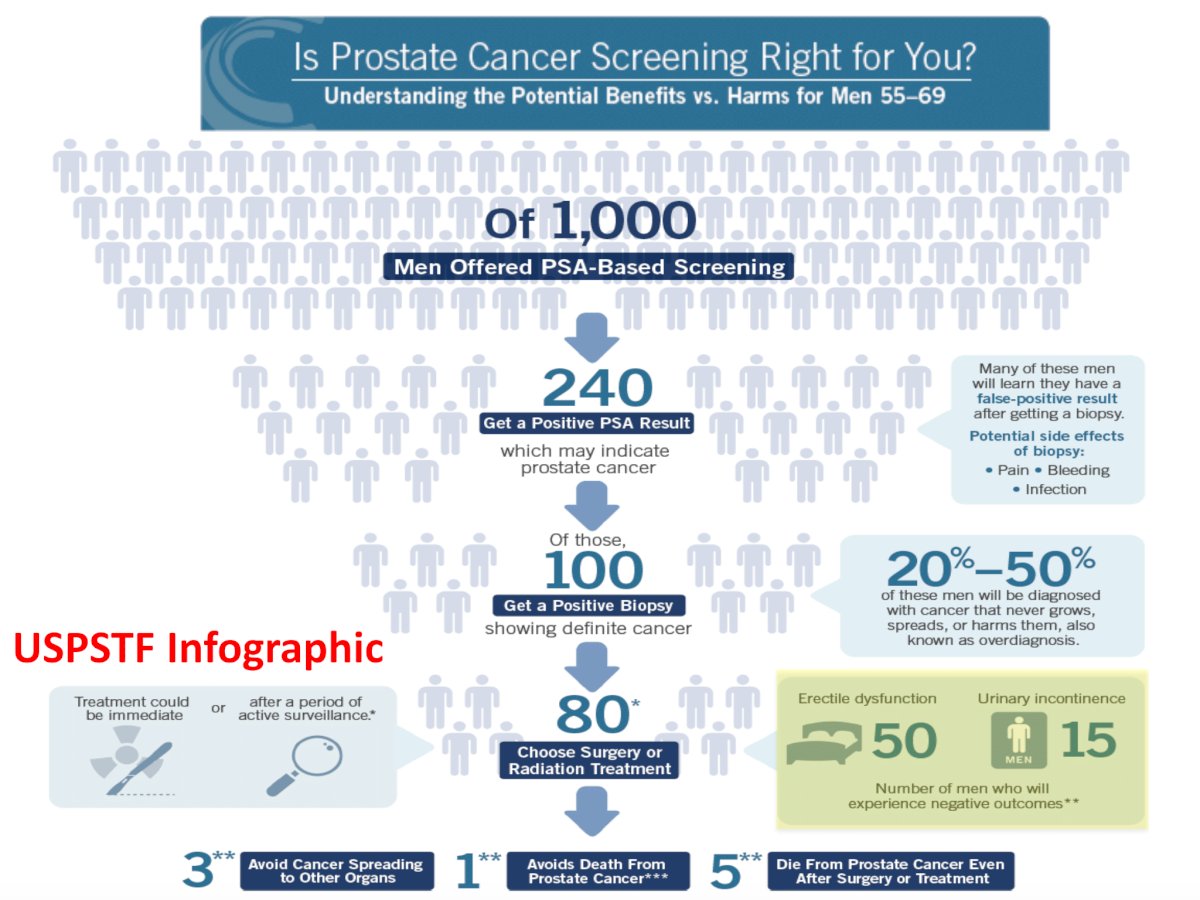
But do these incremental differences matter? When we take a step back and consider that of 1,000 men offered PSA-based screening, 240 are found to have a positive PSA result, 100 are diagnosed with prostate cancer, and 80 choose surgery or radiation, we truly appreciate the population-level effect of any treatment advances on the general population.
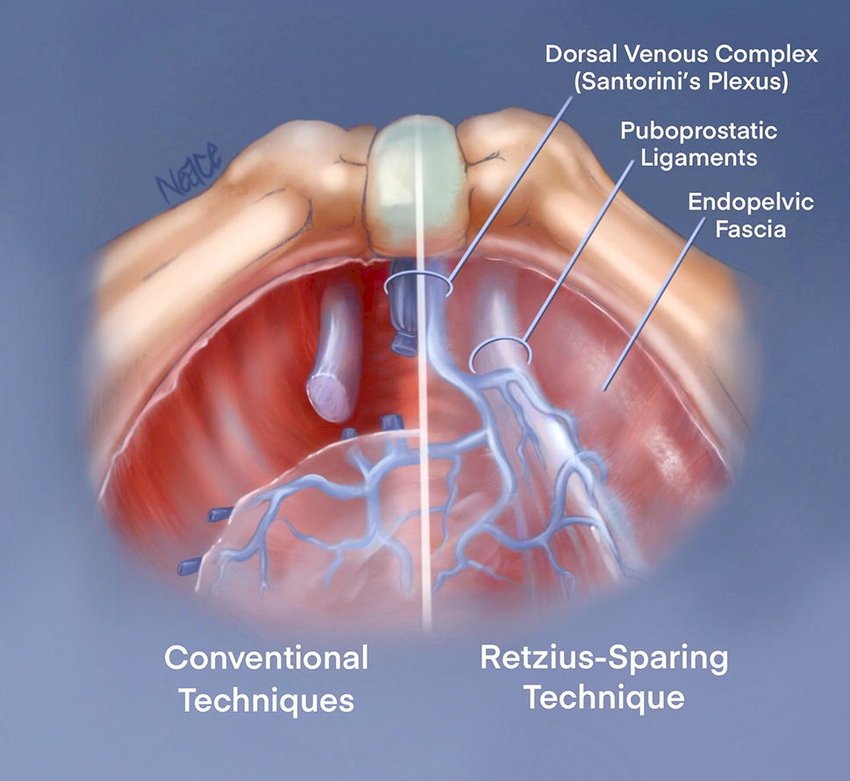
To this end, the Retzius-sparing approach has been developed over the last decade in an attempt to improve post-operative functional outcomes, mainly immediate urinary continence. This approach preserves the peritoneal attachments of the bladder (i.e., the bladder is not “dropped”), which helps maintain the bladder in the same anatomic position. Furthermore, this technique preserves the structures supporting the anterior urethra: the puboprostatic ligaments, endopelvic fascia, and dorsal venous complex.
A systematic review and meta-analysis of 10 prospective studies, including four randomized controlled trials, demonstrated that this approach significantly improved immediate continence (RR: 1.81, 95% CI: 1.26 – 2.60), at the cost of significantly higher pT2 positive margins (RR: 1.39, 95% CI: 1.01 – 1.91).
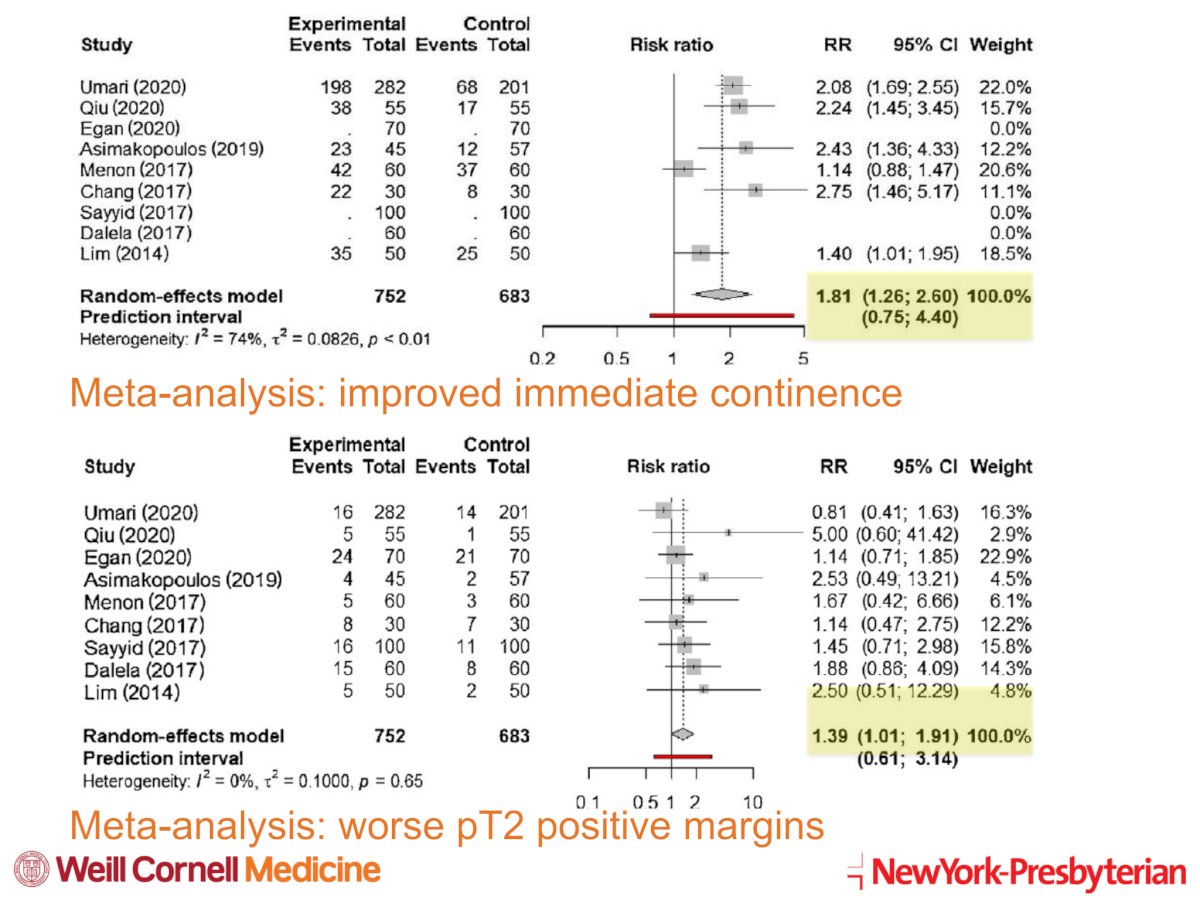
Significantly, this meta-analysis did not demonstrate significant differences in estimated blood loss, 3-, 6-, or 12-months urinary continence, immediate erectile function recovery, or pT3 positive surgical margin status.3
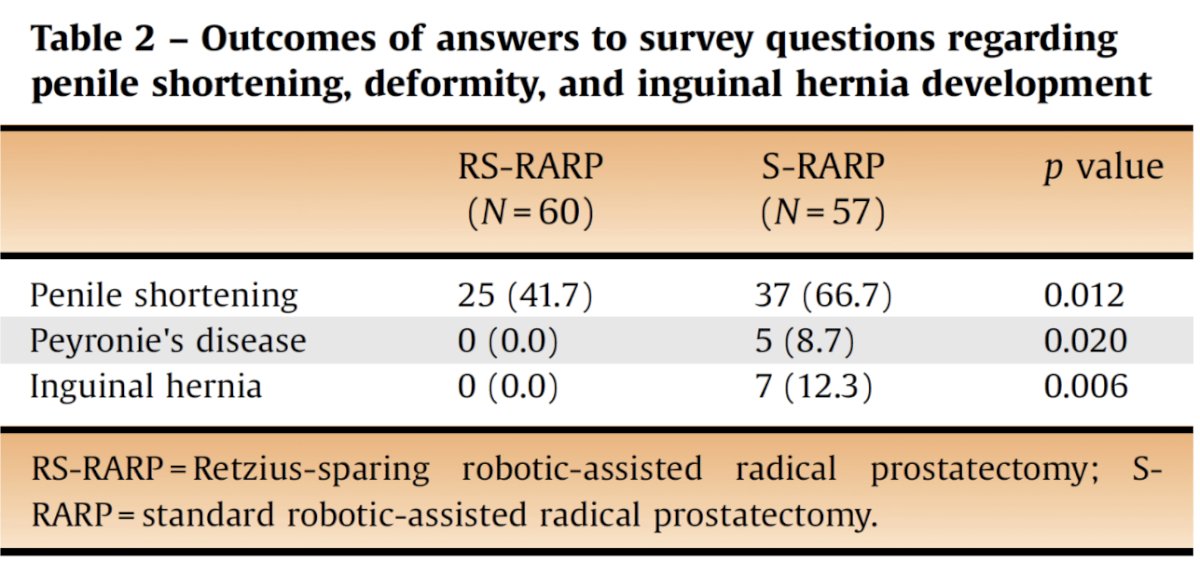
There are also suggestions that the Retzius-sparing approach may be less morbid, compared to standard RALP approaches, for penile shortening, development of Peyronie’s disease, and inguinal hernia sequelae. In a cross-sectional, survey analysis of 117 patients who underwent either Retzius-sparing (n=60) or standard RALP (n=57), there was significantly less penile shortening (42% versus 67%), development of Peyronie’s disease (0% versus 9%), and inguinal hernia (0% versus 12.3%) with the Retzius-sparing approach.4
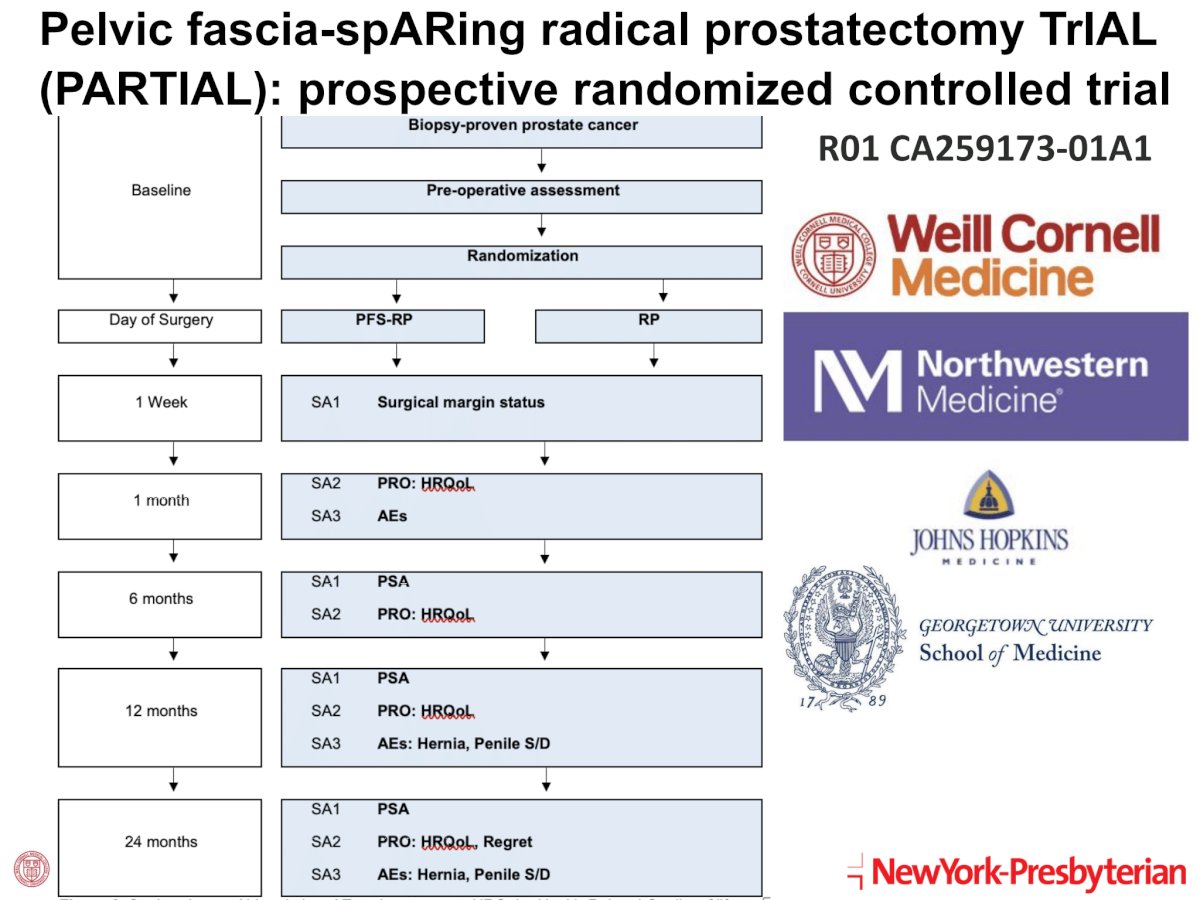
The Pelvic fascia-spARing radical prostatectomy TrIAL(PARTIAL) is a prospective randomized controlled trial that is prospectively evaluating surgical margin status, patient-reported outcomes/health-related quality of life, and adverse events, including hernias and penile shortening/deformity in a randomized fashion.
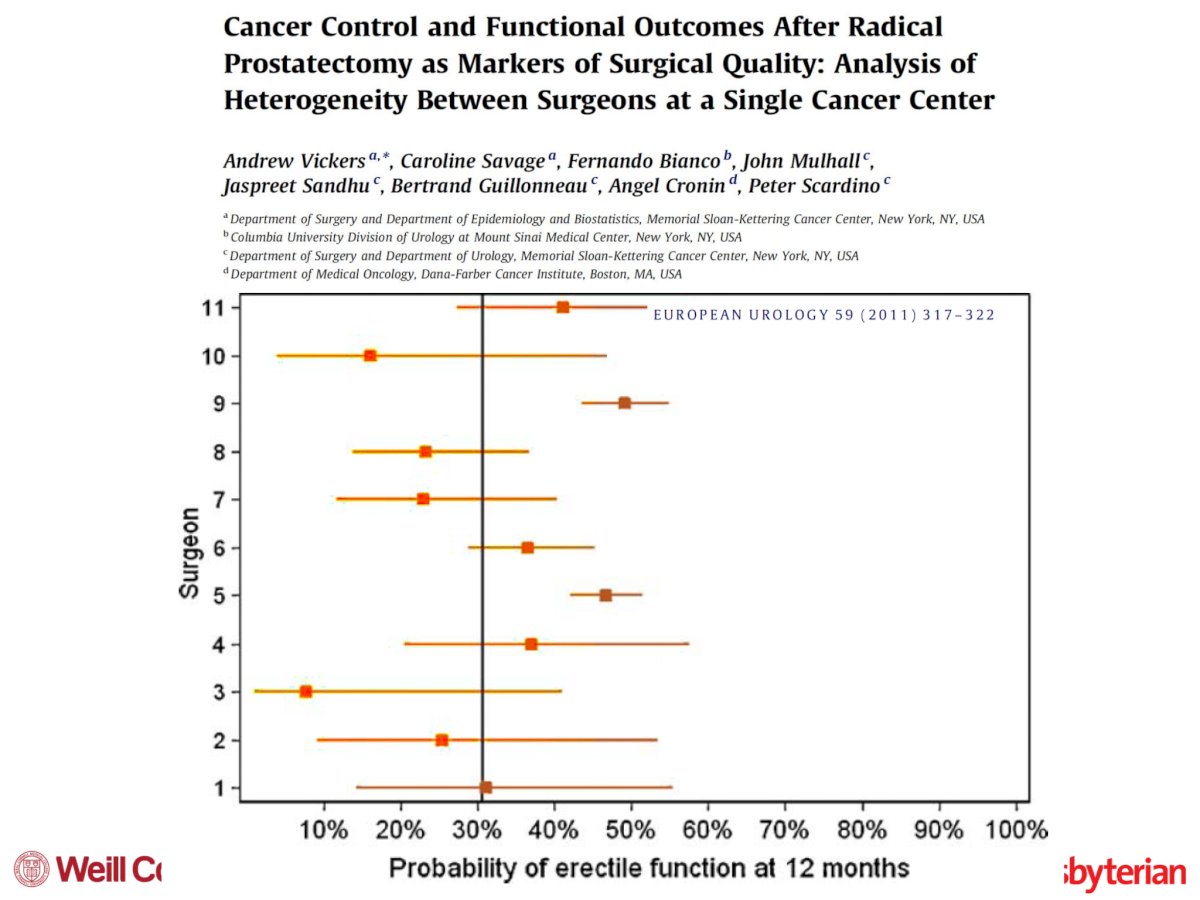
Loss of erectile function remains one of the most ‘notorious’ side effects of radical prostatectomy. There appears to be significant between-surgeon variation in erectile function outcomes, even at the same institutions.5
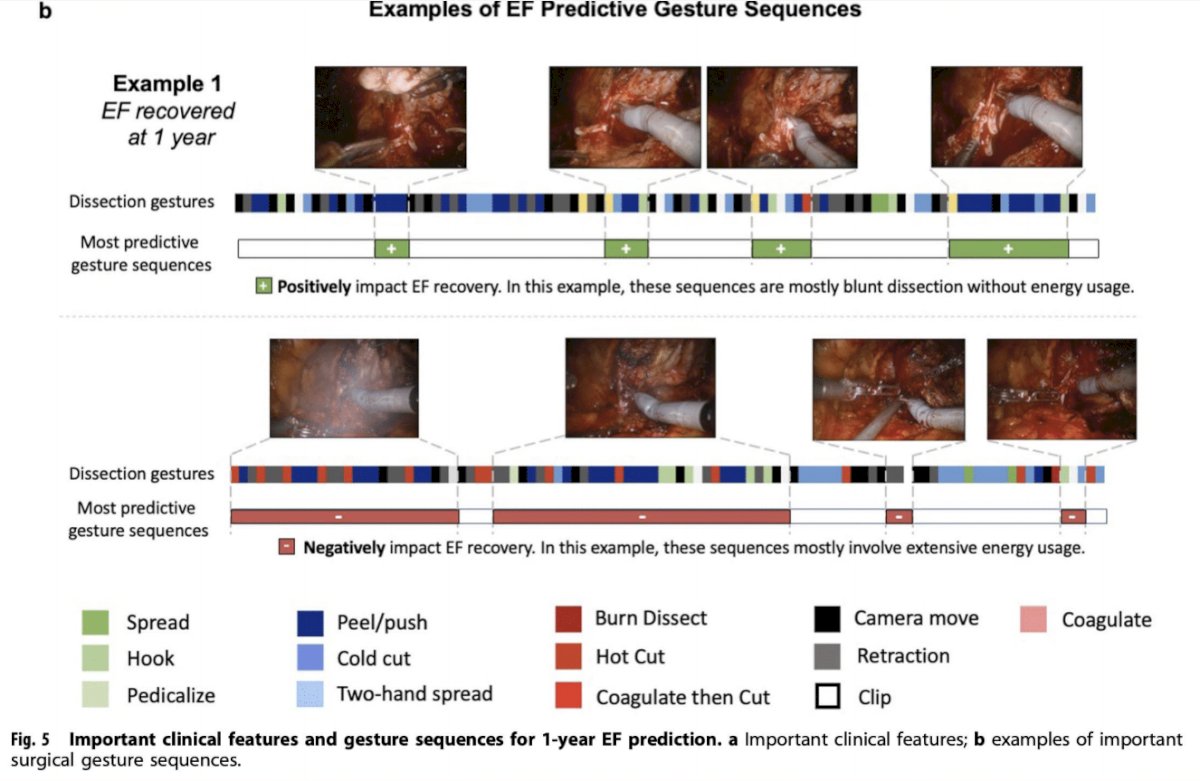
It has thus been hypothesized that such differences may be related to surgical technique, including both tissue handling and energy utilization. Led by Drs. Andrew Hung and Jim Hu, deep learning techniques have been used to assess nerve-sparing techniques during a robotic radical prostatectomy. The investigators have defined a dissection gesture classification, as summarized below:
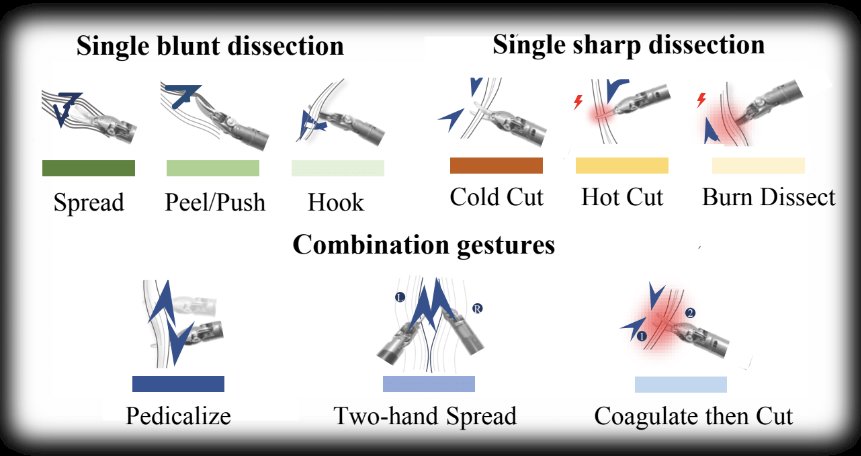
Next, the video with the sequence of surgery was analyzed in the context of these gestures. They identified 34,323 individual gestures performed in 80 nerve-sparing RALPs from two international medical centers. They demonstrated that less use of hot cut and more use of peel/push was statistically associated with better chances of 1-year erectile function recovery. They also demonstrated that there were interactions between surgeon experience and gesture types – similar gesture selection resulted in different erectile function recovery rates dependent on surgeon experience.6
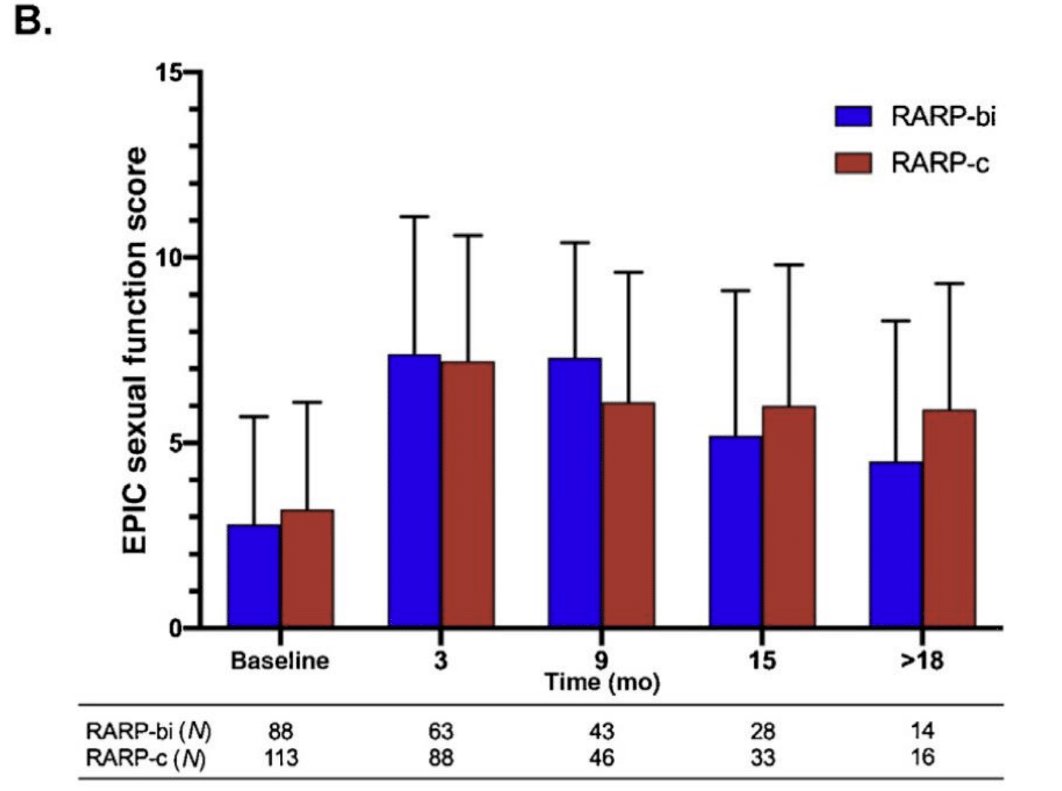
Another important point of discussion regarding surgical techniques is the need for clips during the ligation of the prostatic pedicles. It has long been believed that energy application should be minimized in the prostatic pedicle region to minimize thermal damage to the neurovascular bundles. However, bipolar energy application allows for the controlled transfer of energy between the jaws of the instrument, minimizing energy spread as observed with monopolar energy sources. In 2022, Dr. Hu’s group published the results of a retrospective study of 338 men who underwent a RALP between July 2018 and March 2020. They demonstrated that there were no significant differences in erectile function recovery with the use of bipolar ligation of the prostatic pedicles versus clips.7
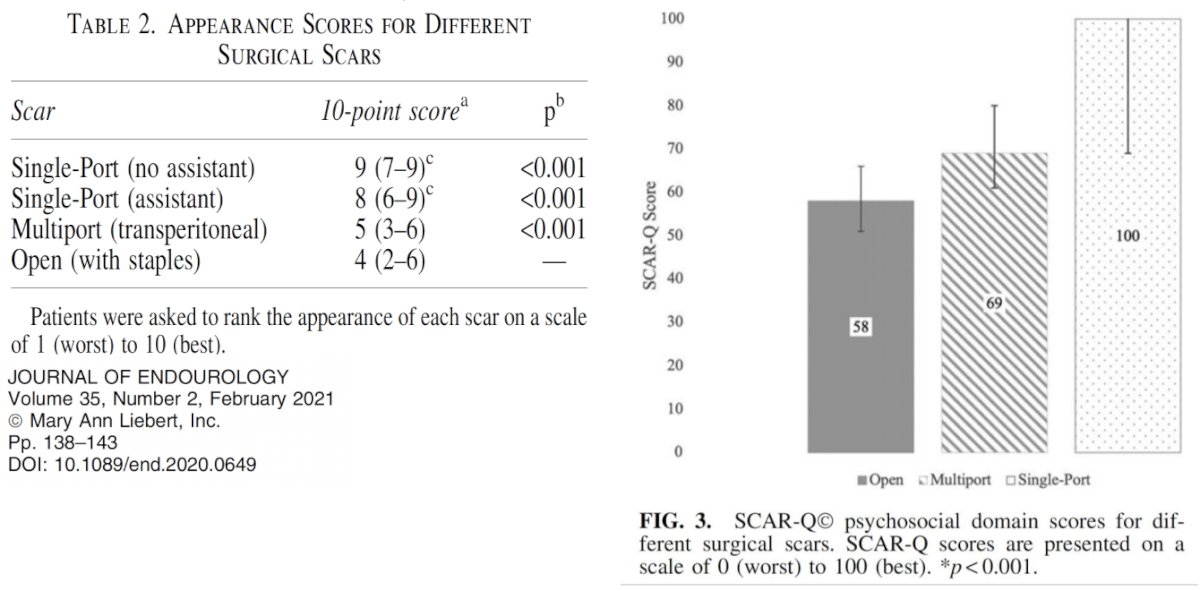
Another novel advance in this field has been the emergence of single port approaches to robotic radical prostatectomy. In addition to avoiding the peritoneum via an extraperitoneal approach (useful for patients with prior laparotomies and adhesions), it appears that the single port scar offers the best cosmesis with the lowest psychosocial impact.8
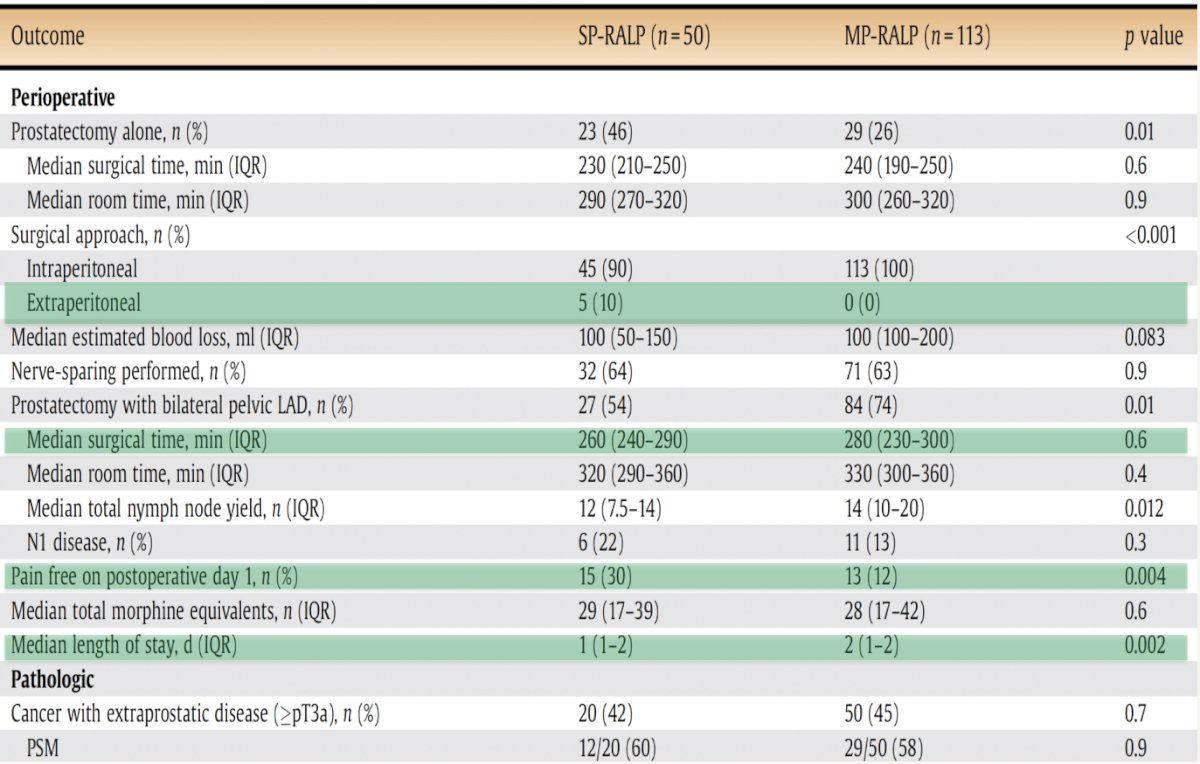
Additional potential advantages of the single port approach include improved pain-free outcomes on post-operative day 1 (30% versus 12%) and a shorter median length of stay (1 versus 2 days).
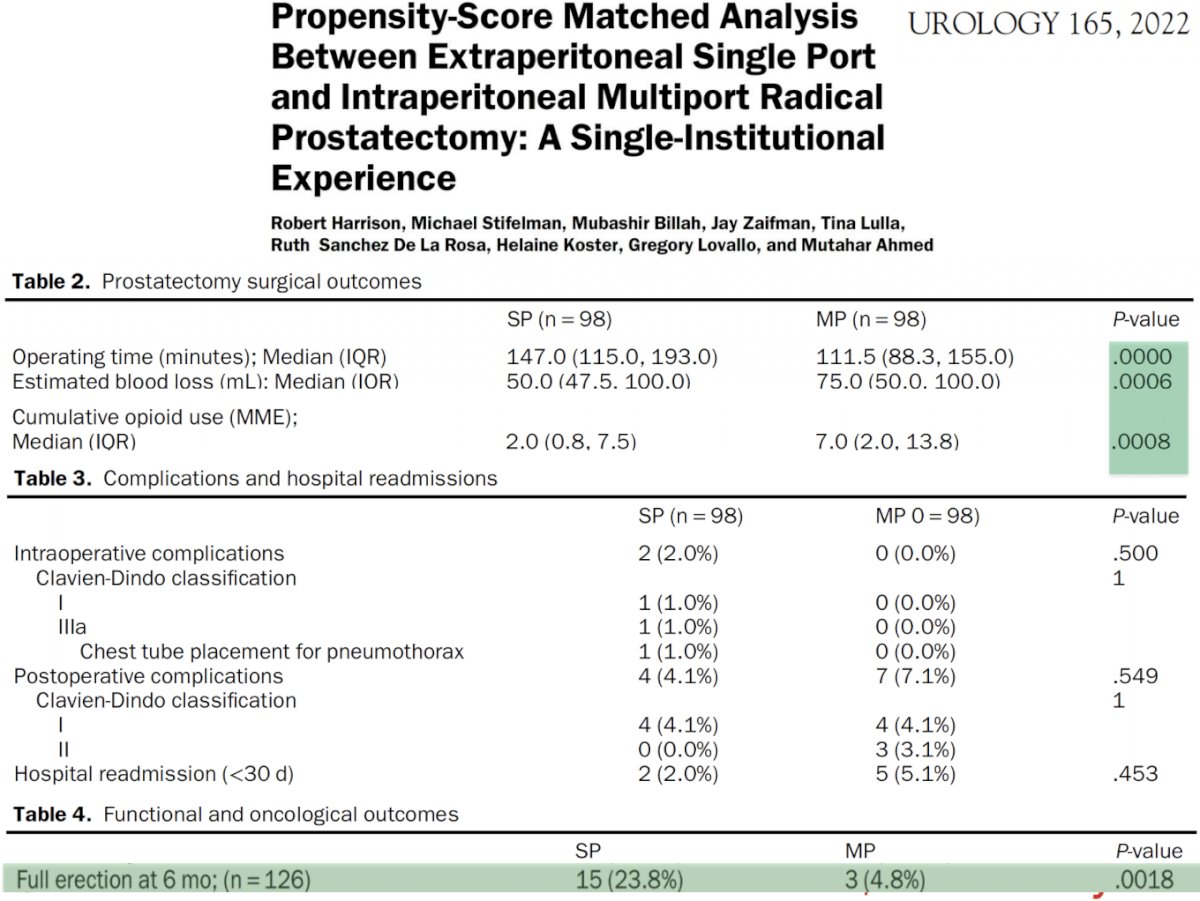
There are also suggestions that this approach may be associated with improved erectile functional outcomes at 6 months, potentially related to tissue handling/manipulation.
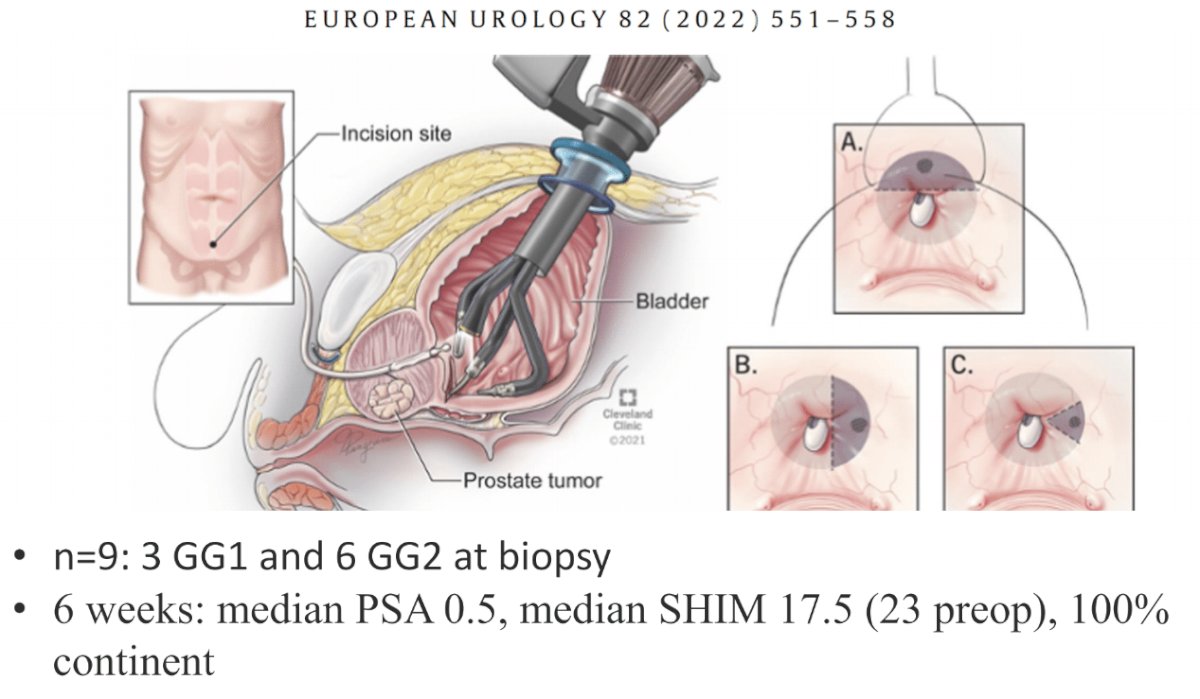
One unique application of the single port platform has been the robotic transvesical partial prostatectomy for localized prostate cancer. In a series of nine patients published in 2022 excellent short-term functional outcomes were reported,10 although this needs validation in larger series with long-term oncologic and functional outcomes.
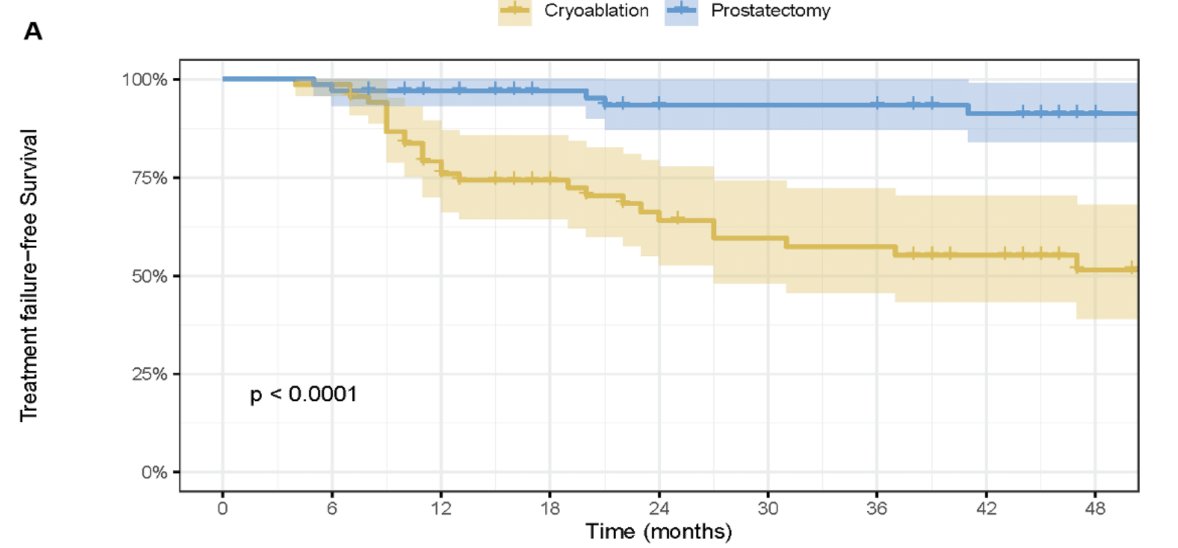
Dr. Hu next briefly discussed his team’s SUO 2023 abstract, a propensity-score matched comparison of partial gland cryoablation versus radical prostatectomy.
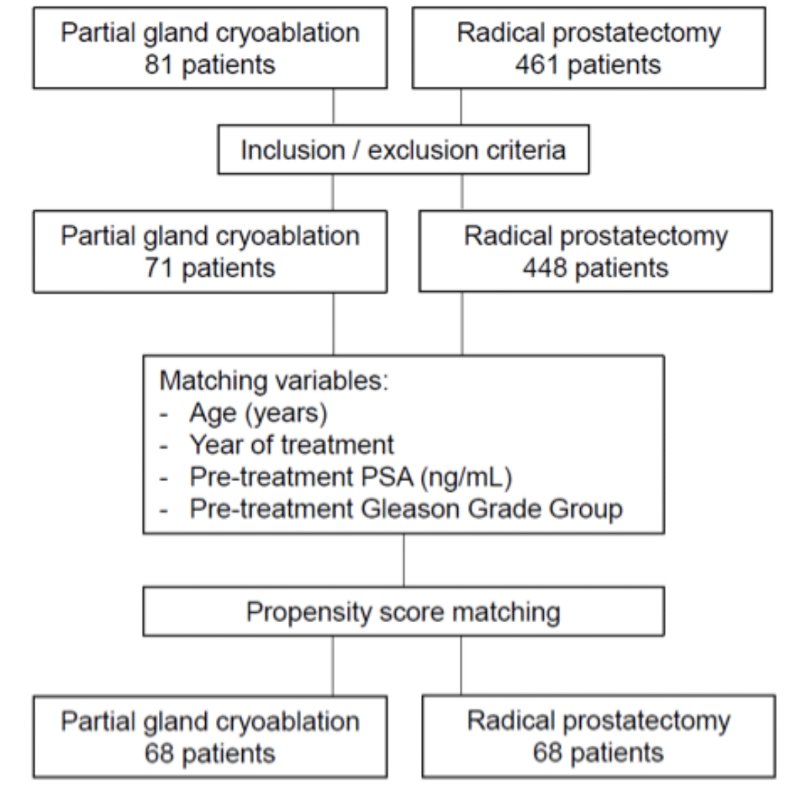
He noted that treatment failure was significantly higher with partial gland cryoablation (52% versus 9%; HR: 7.6, p<0.001).
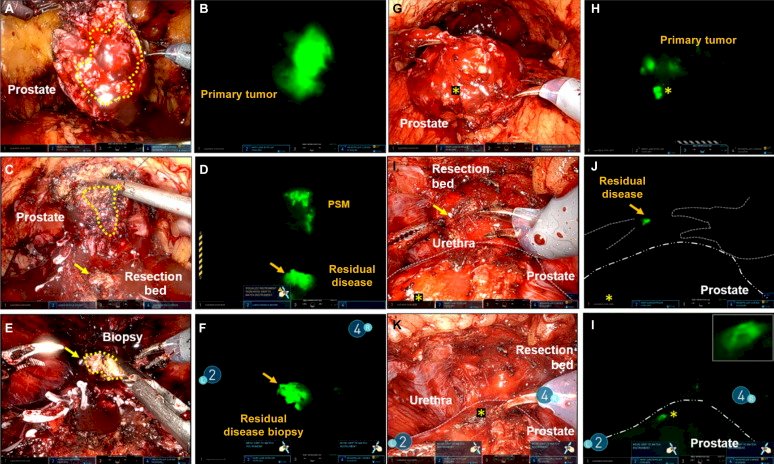
Another exciting development in this field has been the use of a near-infrared, Prostate Specific Membrane Antigen (PSMA)-targeted fluorescence imaging agent, designed for intraoperative prostate cancer visualization. This is particularly useful for men with high-risk prostate cancer undergoing surgery likely to recur due to failure to completely excised regional and/or local disease. In a phase one trial, Nguyen et al. demonstrated the safety and tolerability of this agent (IS-002).11 This agent is currently being evaluated in an ongoing multicenter, phase 2 trial.
Dr. Hu concluded his presentation with the following take home messages:
- Same day radical prostatectomy saves 20% of surgery-related expenses, with similar outcomes
- Patient age should not determine treatment choice
- Less energy used during nerve-sparing improves erectile function outcomes
- There appears to be a patient preference for single port approaches
- PSMA-targeted robotic radical prostatectomy may have future applications for cT3 or worse disease
- Focal therapy has almost 6-fold higher failure rate compared to radical prostatectomy
Presented by: Jim Hu, MD, MPH, Professor, Ronald P. Lynch Professor of Urologic Oncology, Department of Urology, Weill Cornell Urology, New York, NY
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 Society of Urologic Oncology (SUO) annual meeting held in Washington, D.C. between November 28th and December 1st, 2023
References:
- Hu JC, Gold KF, Pahsos CL, et al. Temporal trends in radical prostatectomy complications from 1991 to 1998. J Urol. 2003;169:1443-1448.
- Cheng E, Gereta S, Zhang TR, et al. Same-Day Discharge vs Inpatient Robotic-Assisted Radical Prostatectomy: Complications, Time-Driven Activity-Based Costing, and Patient Satisfaction. J Urol. 2023;210(6):856-864.
- Barakat B, Othman H, Gauger U, et al. Retzius Sparing Radical Prostatectomy Versus Robot-assisted Radical Prostatectomy: Which Technique is More beneficial for Prostate Cancer Patients (MASTER Study)? A Systematic Review and Meta-analysis. Eur Urol Focus. 2022;8:1060-1071.
- Kowalczyk KJ, Davis M, O’Neill J, et al. Impact of Retzius-sparing Versus Standard Robotic-assisted Radical Prostatectomy on Penile Shortening, Peyronie's Disease, and Inguinal Hernia Sequelae. Eur Urol Open Sci. 2020;22:17-22.
- Vickers A, Savage C, Bianco F, et al. Cancer control and functional outcomes after radical prostatectomy as markers of surgical quality: analysis of heterogeneity between surgeons at a single cancer center. Eur Urol. 2011;59(3):317-322.
- Ma R, Ramaswamy A, Xy J, et al. Surgical gestures as a method to quantify surgical performance and predict patient outcomes. NPJ Digit Med. 2022;5(1):187.
- Basourakos SP, Zhu A, Lewicki PJ, et al. Clipless Robotic-assisted Radical Prostatectomy and Impact on Outcomes. Eur Urol Focus. 2022;8(5):1176-1185.
- Huang MH, Schwen ZR, Biles MJ, et al. A Comparative Analysis of Surgical Scar Cosmesis Based on Operative Approach for Radical Prostatectomy. J Endourol. 2021;35(2):138-143.
- Vigneswaran HT, Schwarzman LS, Francavilla S, Abern MR, Crivellaro S. A Comparison of Perioperative Outcomes Between Single-port and Multiport Robot-assisted Laparoscopic Prostatectomy. Eur Urol. 2020;77(6):671-674.
- Kaouk JH, Ferguson EL, Bekac AT, et al. Single-port Robotic Transvesical Partial Prostatectomy for Localized Prostate Cancer: Initial Series and Description of Technique. Eur Urol. 2022;82:551-558.
- Nguyen HG, van den Berg NS, Antaris AL, et al. First-in-human Evaluation of a Prostate-specific Membrane Antigen-targeted Near-infrared Fluorescent Small Molecule for Fluorescence-based Identification of Prostate Cancer in Patients with High-risk Prostate Cancer Undergoing Robotic-assisted Prostatectomy. Eur Urol Oncol. 2023:S2588-9311(23)00146-3.


