(UroToday.com) The 2023 SUO annual meeting included a session on prostate cancer, featuring a presentation by Dr. Eric Li discussing factors associated with PSMA positivity at low PSA after radical prostatectomy. PSMA-based imaging is the preferred imaging modality recommended by NCCN guidelines for work-up of suspected recurrent or persistent prostate cancer after initial treatment with radical prostatectomy or prostate radiation and is increasingly being utilized in clinical practice.
However, there is currently sparse data on the relative yield of PSMA PET/CT at low PSA values at biochemical recurrence. Dr. Li and colleagues evaluated their institutional PSMA PET/CT cohort of post-radical prostatectomy patients which includes 251 men with PSAs under 0.5 ng/mL at the time of imaging, to identify clinical factors associated with scan positivity.
This study retrospectively identified men treated initially with radical prostatectomy who underwent Gallium-68 or F-18 piflufolastat (DCFPyL) PSMA PET/CT for work-up of recurrence across an 11 hospital system from July 2021 to March 2023. Patient characteristics, including demographic, baseline clinical, pathologic, and imaging variables, were obtained. PSMA positivity was determined based on radiology interpretation, and equivocal or likely benign lesions were considered negative. Exclusion criteria included those patients with a history of systemic therapy or known metastatic disease (n = 216), receipt of focal therapy only (n = 4), or those who had bladder outlet procedures only (n = 3). Clinical variables were compared with Wilcoxon Rank Test, Chi square, and Fishers’ exact test, and then with univariable and multivariable logistic regression. Additionally, PSA was log transformed given non-normal distribution for logistic regression.
The median PSA at time of PSMA PET/CT was 0.37 ng/mL (IQR 0.15 - 1.29 ng/mL), and 48.9% (210/429) of patients initially managed with radical prostatectomy were found to have PSMA positive finding suspicious for recurrence. The baseline characteristics in this cohort are as follows:
Rates of scan positivity among men with PSAs <0.5 ng/mL and those <0.2 ng/mL were both 37%. Among patients with suspicious PSMA positive findings, 14% had positivity within prostate bed only, 35% had N1 disease, and 51% had M1 disease. On multivariable analysis, age (OR 1.05, 95% CI 1.01, 1.08), PSA at PSMA scan (p < 0.001), and radical prostatectomy Gleason Grade Group (p = 0.03) were significantly associated with PSMA positivity: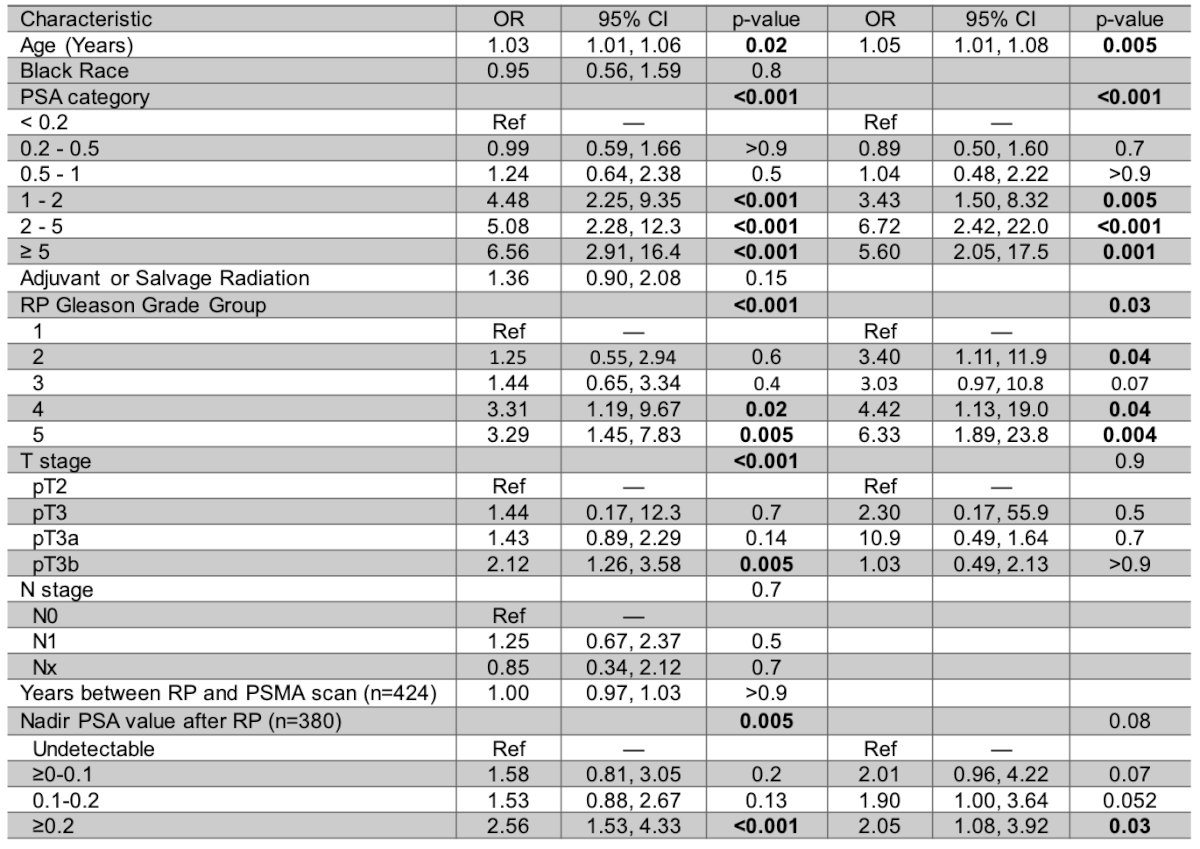
In a subset multivariable analysis for men with PSAs under 0.5 ng/mL at time of imaging, radical prostatectomy Gleason Grade group (p = 0.02) and history of post-operative radiation (OR 2.12, 95% CI 1.13, 4.00, p = 0.02) were associated with scan positivity.
Dr. Li concluded his presentation discussing factors associated with PSMA positivity at low PSA after radical prostatectomy with the following take-home points:
- PET PSMA/CT for recurrence after radical prostatectomy identifies locoregional or metastatic disease in ~49% of patients
- Though men with higher PSAs (≥ 1 ng/ml) have the highest probability of harboring PSMA positive disease, approximately 40% of men with PSAs <0.2 ng/ml had positive imaging findings concerning for recurrence
- These men harbored higher grade disease at prostatectomy and were more likely to have received post-operative radiation
- These findings suggest PET-PSMA imaging at low PSAs can be considered in selective individuals even at low PSA to inform salvage therapies
Presented by: Eric V. Li, MD, Northwestern University, Chicago, IL
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 Society of Urologic Oncology (SUO) Annual Meeting, Washington, D.C., Tues, Nov 28 – Fri, Dec 1, 2023.


