(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas was host to the Bladder Cancer Course and the Session Non-Muscle Invasive Bladder Cancer (NMIBC). Dr. Liao discussed the novel approaches to non-muscle invasive bladder cancer surgery.
Transurethral resection of bladder tumor (TURBT) is a common but technically challenging urologic procedure. Its primary objectives are to diagnose, stage, and treat non-muscle invasive bladder cancer (NMIBC). The goals of TURBT include the complete resection of all visible papillary tumors, biopsy of any suspicious flat lesions that might represent carcinoma in situ (CIS), and providing sufficient tissue for accurate pathological diagnosis. Achieving these goals is critical for effective patient management and treatment planning.
However, there are several recognized shortcomings associated with cystoscopy and TURBT, including operator dependency, missed tumors, and multifocal disease that can affect patient risk assessment and prognosis. Additionally, there are multiple indeterminate lesions that can mimic CIS. The quality of TURBT is critical, as incomplete resections can lead to under-staging and necessitate repeat procedures. Clinical documentation of cystoscopy or TURBT findings often remains suboptimal, with issues in text-based cystoscopy notes, operative reports, intravesical therapy treatment notes, and pathology reports. Enhanced cystoscopy technologies, such as blue light cystoscopy (BLC) and other emerging methods, aim to improve cancer detection and the quality of cystoscopy and TURBT. However, factors such as access, cost-effectiveness, and the impact on clinical workflow and morbidity must be considered.
In terms of the quality of the first cystoscopy after TURBT, a collaborative study by the EORTC group analyzing 2,410 patients from seven EORTC phase III trials showed significant variation in recurrence rates at the first follow-up cystoscopy. In patients with multiple tumors who received adjuvant treatment, recurrence rates varied between 7.4% and 45.8%. This suggests that the quality of TURBT performed by individual surgeons was a critical factor influencing these outcomes.1
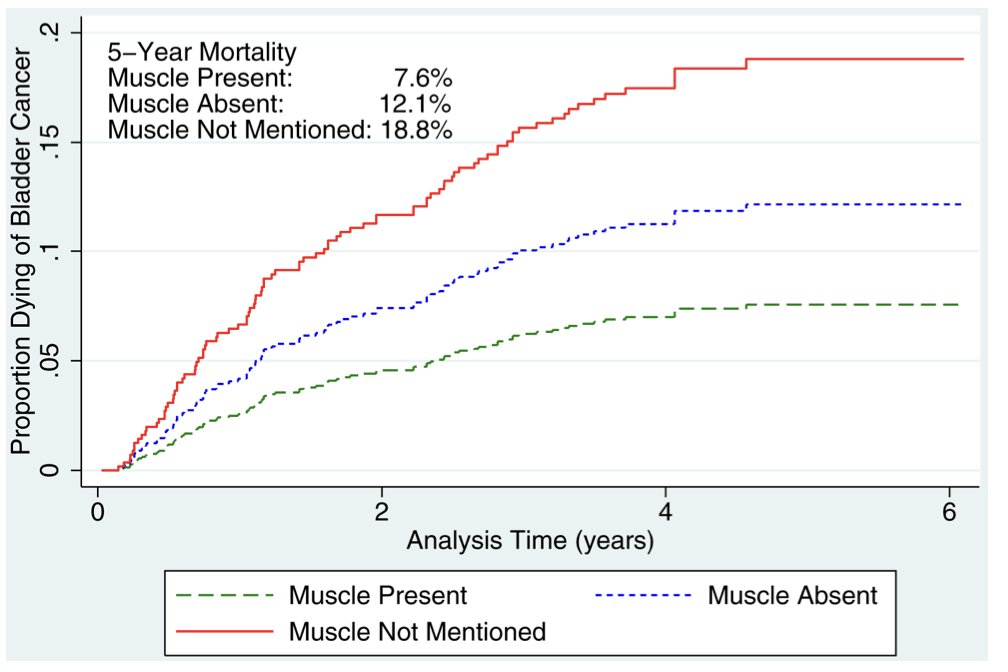
Similarly, a study using the Los Angeles SEER registry evaluated 1,865 patients, 335 urologists, and 27 pathologists. The study found that mortality was associated with staging quality. Among patients with high-grade disease, the 5-year cancer-specific mortality was 8.0% when muscle was present in the specimen, 13.0% when muscle was absent, and 21.5% when muscle presence was not mentioned. This highlights the critical importance of thorough and accurate TURBT for staging and treatment planning.2
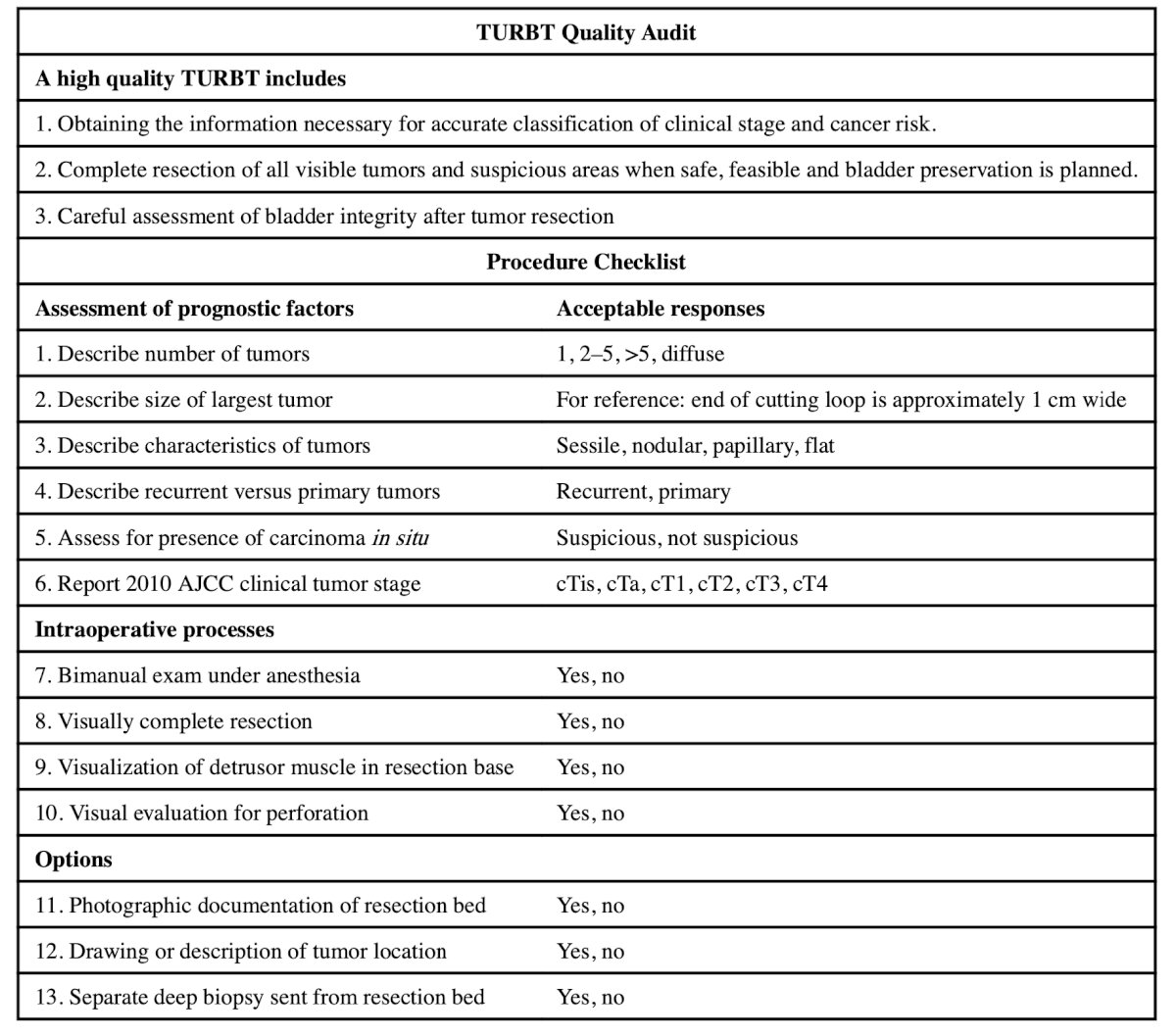
Dr. Liao presented a 10-item checklist designed to improve the reporting of critical elements during TURBT. This checklist, developed by a multi-institutional group, identifies important steps for high-quality TURBT. It focuses on prognostic factors such as the number and size of tumors, recurrence, the presence of carcinoma in situ (CIS), intraoperative processes, the achievement of visually complete resection, detrusor muscle in the resection bed, and any perforations, among others. These elements, illustrated in the table below, aim to standardize TURBT procedures and improve patient outcomes.
Dr. Liao moved on to discuss that BLC has Level 1 evidence supporting the detection of additional bladder tumors than white light cystoscopy (WLC) and it is recommended ('when available') by AUA and EAU NMIBC guidelines.
In a multicenter registry study involving 533 patients, the sensitivity of white light cystoscopy (WLC) was found to be 76%, whereas blue light cystoscopy (BLC) showed a significantly higher sensitivity of 91%. The combination of both methods increased the sensitivity to 98%. Specifically, BLC improved cancer detection by 12% for papillary tumors and 43% for carcinoma in situ (CIS). Additionally, BLC identified 25% more lesions in cases where WLC results were negative. This enhanced detection capability led to a 6% migration in AUA risk groups and a 14% change in patient management strategies. Notably, the false positive rates between WLC and BLC were comparable, with WLC at 25% and BLC at 30%.4
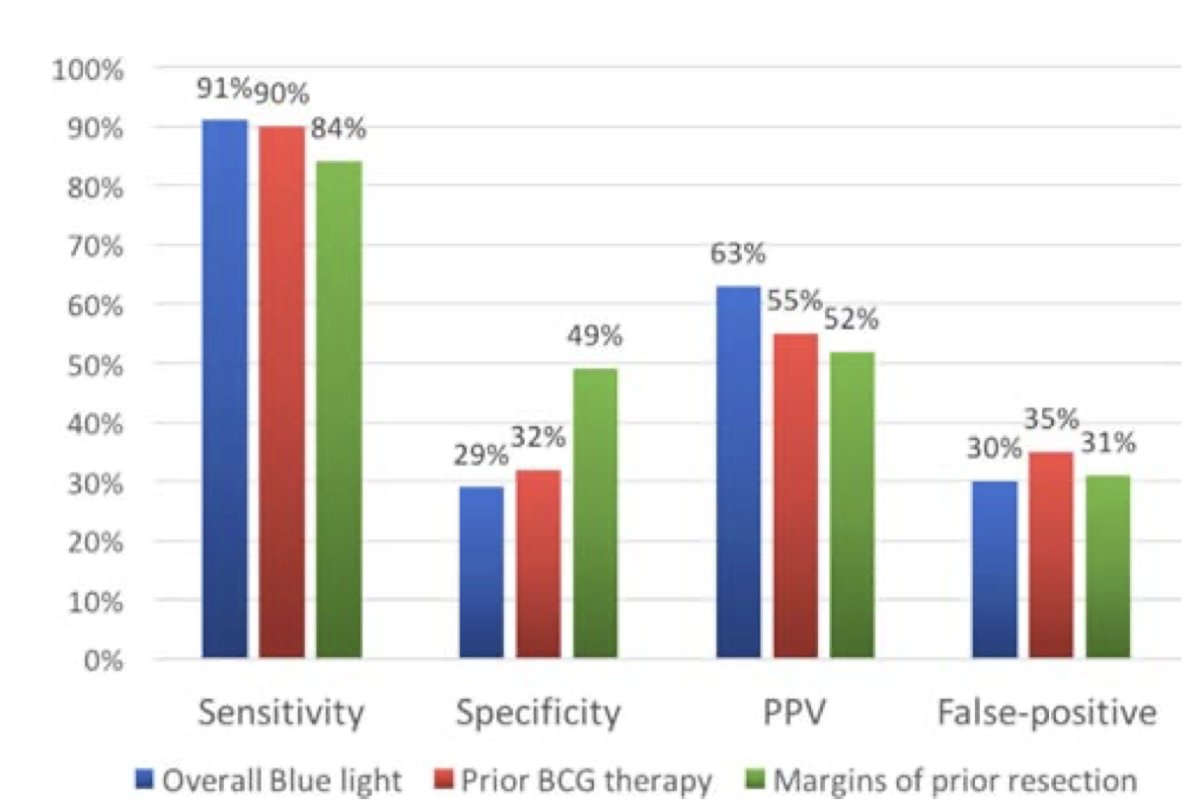
To minimize false-positive findings in BLC, several technical considerations are essential. Tangential fluorescence can occur in areas such as bladder side walls, bladder neck, trigone, trabeculations, and the rim of diverticula. It's important to differentiate these from true positive findings. Inflammation and urinary tract infections (can also cause false positives, so it is crucial to document if the patient has had recent intravesical therapy, a recent transurethral resection (TUR), or a stent. The "scrap" test, which involves scraping the urothelium, can help verify suspicious areas.5
Can we overcome the shortcomings of cystoscopy and TURBT integrating artificial intelligence? Dr Liao briefly mentioned a novel system named CystoNet. This program utilizes a YOLO platform image analysis technology to investigate videos captured during cystoscopy. The program worked in several steps to screen individual frames and outline suspicious growths/tumors using convolutional neural networks. AI has shown to improve the sensitivity of WLC and demonstrates great potential to objectively facilitate diagnosis in real time. Current applications of AI in bladder cancer detection include frame-level classification, tumor localization, tumor segmentation, and digital staining as shown below:
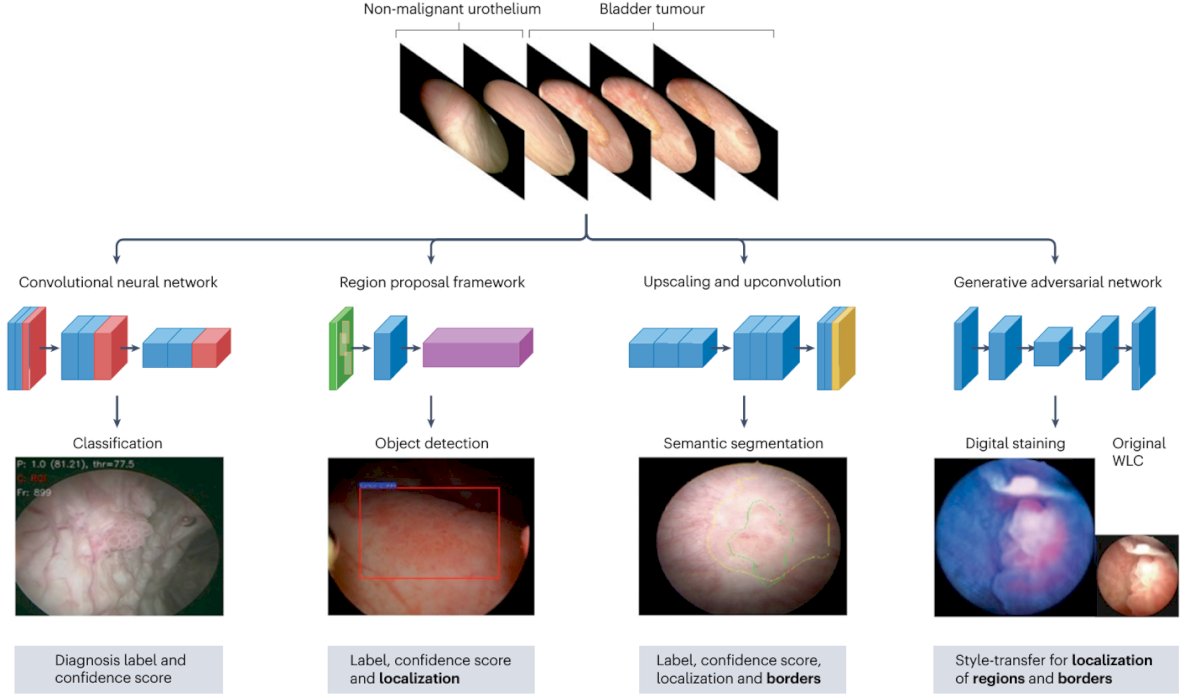
The CystoNet was developed using data from 100 patients, with 95 patients in the training set and 5 in the test set. The system achieved a per-frame sensitivity of 90.9%, per-frame specificity of 98.6%, and per-tumor sensitivity of 95.5%.
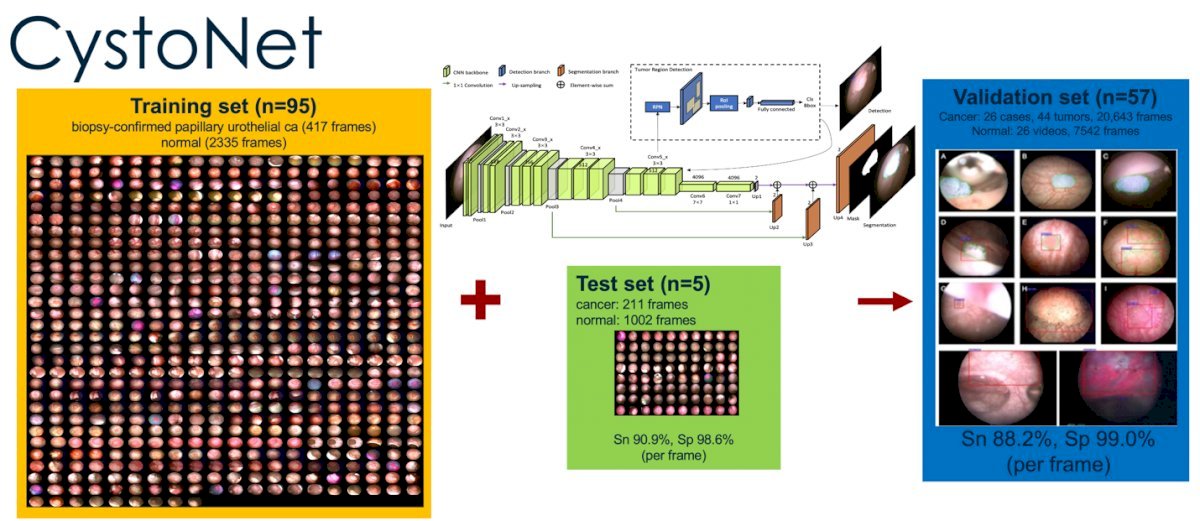
However, applicability in real-time remains a challenge. Dr. Liao noted that they tested using a gaming computer to support CystoNet during a TURBT procedure, and it worked perfectly fine. Nevertheless, further integration between industry and researchers is needed to carry this innovation into clinical practice across different settings.
Other applications of AI in cystoscopy include diagnosing conditions such as follicular cystitis, UPUMP (urothelial proliferation of uncertain malignant potential), melanosis, malakoplakia, and low-grade urothelial proliferation. These AI tools can aid in the identification and differentiation of these conditions, enhancing diagnostic accuracy and potentially improving patient outcomes. Integrating AI in diagnostic cystoscopy could help facilitate the diagnosis of rare conditions.
Standard TURBT vs. En bloc resection of bladder tumor (ERBT)En bloc resection of bladder tumors has been proposed as an alternative to conventional TURBT. This technique aims to remove the tumor in one piece, potentially reducing the risk of tumor reimplantation or dissemination. Additionally, complete tumor resection can be confirmed histologically, as clear resection margins are achieved in 94–99% of cases. This method enhances the precision of tumor removal and may improve patient outcomes by ensuring more accurate staging and potentially reducing recurrence rates.
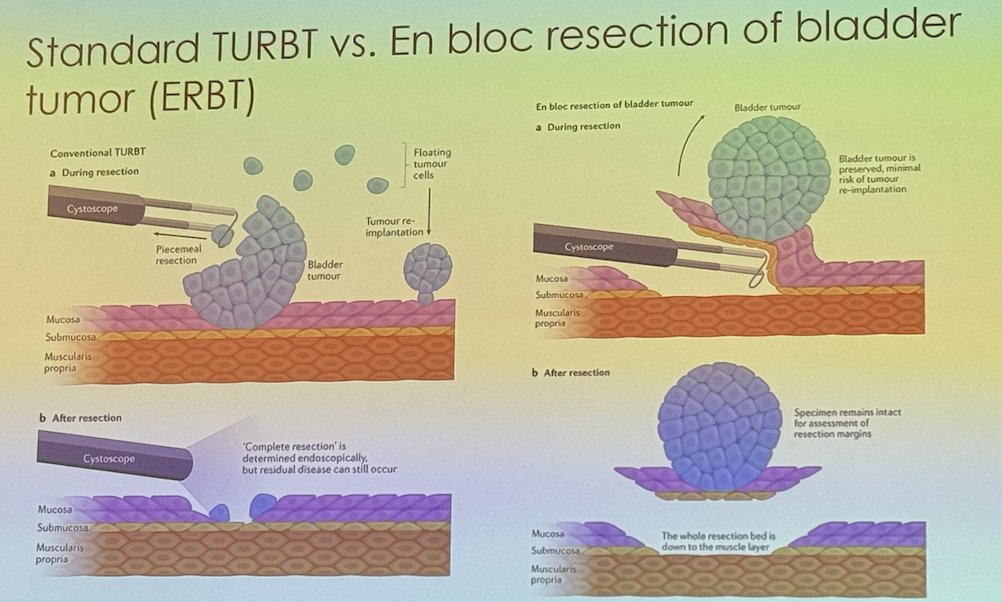
In a phase 3, multicenter, randomized trial led by Jeremy Teoh in China, 350 patients with bladder tumors ≤ 3 cm were recruited from 13 centers to compare ERBT to conventional transurethral resection of bladder tumor TURBT. The study found that the 1-year recurrence rate for ERBT was 29% compared to 38% for conventional TURBT, indicating a significant benefit for the en bloc technique in reducing recurrence rates within the first-year post-surgery.
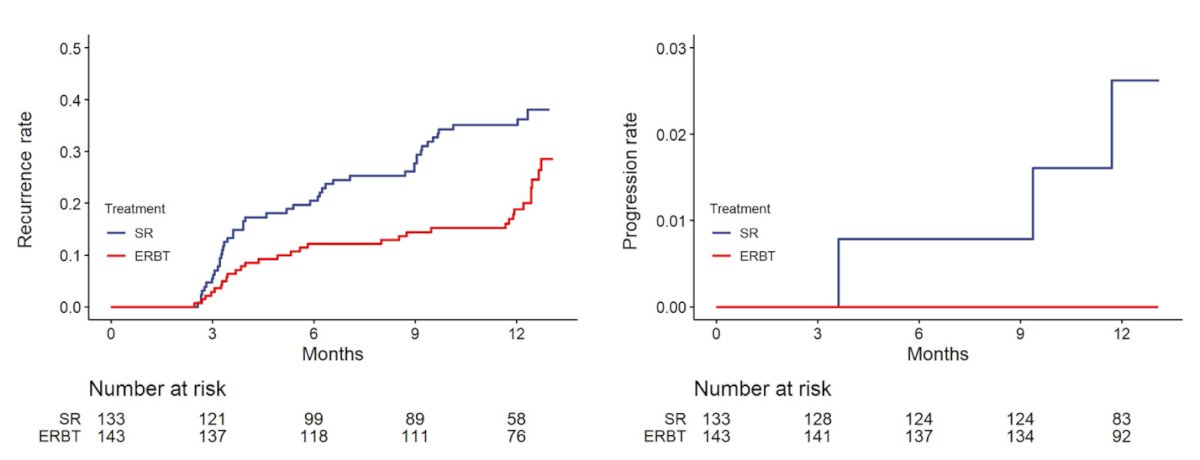
Notably, the operative time was longer in the ERBT group, with a median of 28 minutes compared to 22 minutes for the TURBT group. The benefits of ERBT were particularly significant in patients with tumors measuring 1-3 cm, single tumors, Ta stage tumors, and those classified as EAU intermediate risk.
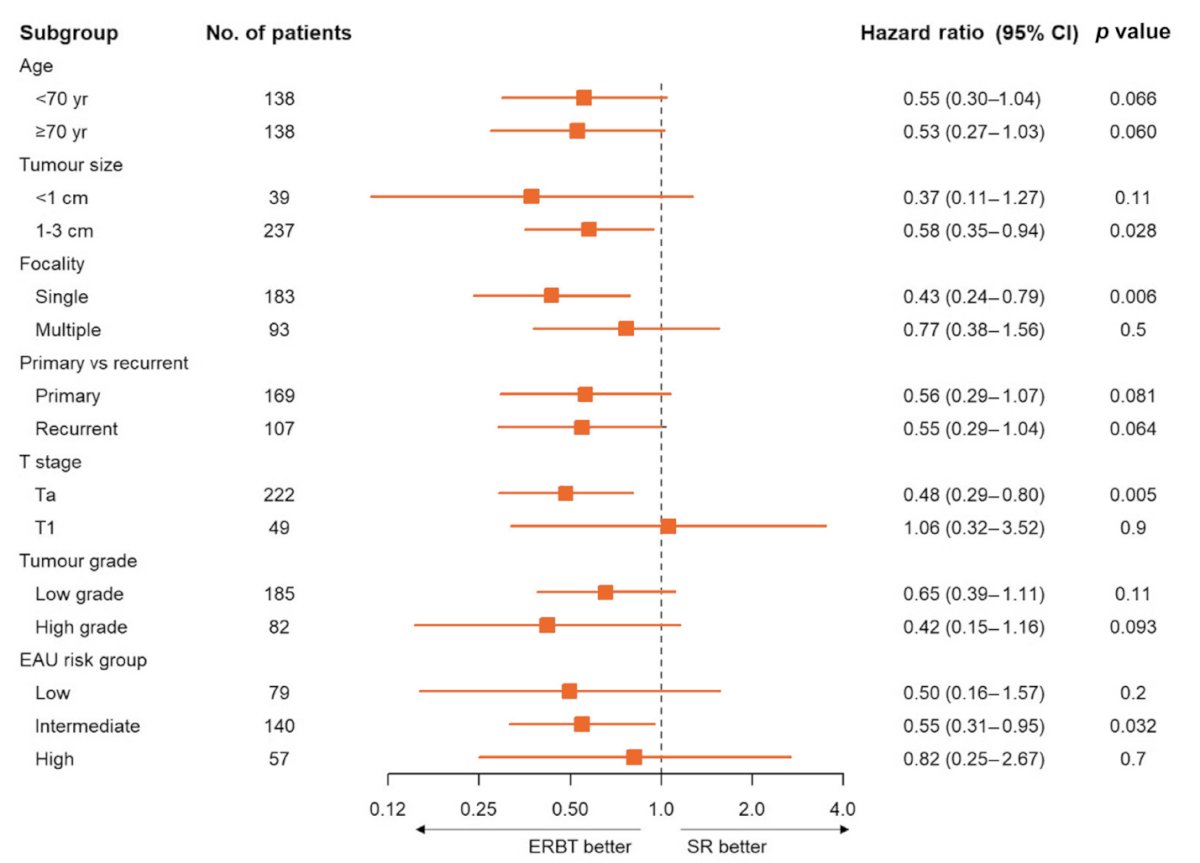
However, several outstanding questions remain. Why is there a discrepancy between the results of this trial and those of other studies? What is the impact of intravesical therapy and the use of enhanced imaging technologies? Can improvements in the quality of the resected tissue lead to better selection of appropriate adjuvant treatments? Additionally, what are the outcomes for tumors larger than 3 cm? Further research is needed to address these questions and fully understand the implications of en bloc resection for bladder cancer treatment.
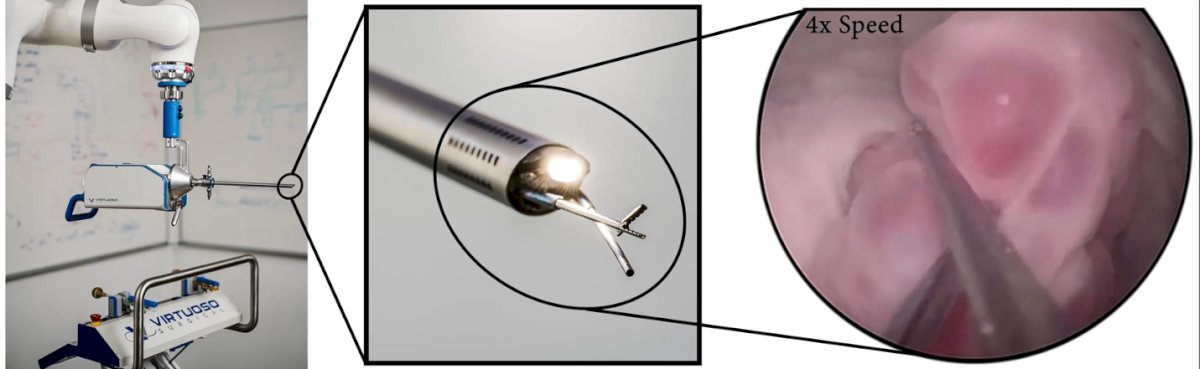
Dr. Liao briefly mentioned the Virtuoso Surgical system, a robotic-assisted surgery technology developed by Vanderbilt investigators. This system offers advanced capabilities for rigid endoscopic surgery through two needle-sized, interchangeable manipulators. These tools allow for precise tissue lifting and retraction, potentially improving the precision of procedures such as ERBT. This technology is still in development but holds promise for enhancing endoscopic surgery by offering more controlled and flexible surgical movements.
The key points highlighted in Dr. Liao's presentation were:
- TURBT quality is crucial as it directly impacts oncologic outcomes
- Blue light cystoscopy (BLC) has Level 1 evidence supporting its use to improve detection of papillary tumors and CIS
- Augmented cystoscopy demonstrates promising potential in advancing tumor detection and offering intraoperative clinical decision support
- There is ongoing work on AI algorithms continues to focus on optimizing training using video sequences, integration into real-time clinical practice, and improving user interfaces.
- En bloc resection of bladder tumors adheres to oncological principles, especially in tumors smaller than 3 cm, and may improve oncologic outcomes by providing clear resection margins and minimizing tumor reimplantation risks.
Presented by: Joseph Liao, MD, Professor of Urology at Stanford University, Palo Alto, CA, USA.
Written by: Julian Chavarriaga, MD – Staff Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:- Brausi M, Collette L, Kurth K, van der Meijden AP, Oosterlinck W, Witjes JA, Newling D, Bouffioux C, Sylvester RJ; EORTC Genito-Urinary Tract Cancer Collaborative Group. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: a combined analysis of seven EORTC studies. Eur Urol. 2002 May;41(5):523-31. doi: 10.1016/s0302-2838(02)00068-4. PMID: 12074794.
- Chamie K, Ballon-Landa E, Bassett JC, Daskivich TJ, Leventhal M, Deapen D, Litwin MS. Quality of diagnostic staging in patients with bladder cancer: a process-outcomes link. Cancer. 2015 Feb 1;121(3):379-85. doi: 10.1002/cncr.29071. Epub 2014 Oct 22. PMID: 25339141; PMCID: PMC6209593.
- Anderson C, Weber R, Patel D, Lowrance W, Mellis A, Cookson M, Lang M, Barocas D, Chang S, Newberger E, Montgomery JS, Weizer AZ, Lee CT, Kava BR, Jackson M, Meraney A, Sjoberg D, Bochner B, Dalbagni G, Donat M, Herr H. A 10-Item Checklist Improves Reporting of Critical Procedural Elements during Transurethral Resection of Bladder Tumor. J Urol. 2016 Oct;196(4):1014-20. doi: 10.1016/j.juro.2016.03.151. Epub 2016 Apr 1. PMID: 27044571; PMCID: PMC5460769.
- Daneshmand S, Bazargani ST, Bivalacqua TJ, Holzbeierlein JM, Willard B, Taylor JM, Liao JC, Pohar K, Tierney J, Konety B; Blue Light Cystoscopy with Cysview Registry Group. Blue light cystoscopy for the diagnosis of bladder cancer: Results from the US prospective multicenter registry. Urol Oncol. 2018 Aug;36(8):361.e1-361.e6. doi: 10.1016/j.urolonc.2018.04.013. Epub 2018 May 30. PMID: 29859728.
- Ghoreifi A, Daneshmand S. Technical Considerations to Minimize False-Positive Findings in Blue Light Cystoscopy for Nonmuscle-Invasive Bladder Cancer. Journal of Urology [Internet]. [cited 2024 Dec 3];0(0). Available from: https://doi.org/10.1097/JU.0000000000004250
- Shkolyar E, Zhou SR, Carlson CJ, Chang S, Laurie MA, Xing L, Bowden AK, Liao JC. Optimizing cystoscopy and TURBT: enhanced imaging and artificial intelligence. Nat Rev Urol. 2024 Jul 9. doi: 10.1038/s41585-024-00904-9. Epub ahead of print. PMID: 38982304.
- Yuen-Chun Teoh J, Cheng CH, Tsang CF, Kai-Man Li J, Kwun-Chung Cheng B, Hoi-Chak Chan W, Kwun-Wai Chan W, Churk-Fai Li T, Chiu Y, Law MC, Lok-Hei Leung C, Sze-Ho Ho B, Yue-Kit Lee C, Cheong-Kin Chan R, Shu-Yin Chan E, Chan MT, Hok-Leung Tsu J, Tam HM, Lam KM, So HS, Cho CL, Ng CM, Chan CK, Liu PL, Wing-Hong Chu R, Tsui-Lin Ng A, Chu SK, Yee CH, Yiu MK, Lo KL, Au WH, Ma WK, Ka-Fung Chiu P, Sze-Wan Kwok H, Yip SY, Leung CH, Ng CF; EB-StaR Study Group. Transurethral En Bloc Resection Versus Standard Resection of Bladder Tumour: A Randomised, Multicentre, Phase 3 Trial. Eur Urol. 2024 Aug;86(2):103-111. doi: 10.1016/j.eururo.2024.04.015. Epub 2024 Apr 30. PMID: 38692956.


