(UroToday.com)The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Bladder Cancer Course and the Session Muscle Invasive Bladder Cancer Part I. Dr. Sarah Psutka proposed a Personalized and Pragmatic Approach to (P)rehabilitation for Patients with Bladder Cancer.
Dr. Psutka began her presentation by emphasizing that radical cystectomy is a highly morbid procedure, with a 90-day mortality rate of 5-15% and 25-95% of patients experiencing complications related to the procedure. In the RAZOR study comparing open versus robotic radical cystectomy, the complication rates were 69% and 67%, respectively, with 24% of the complications being minor. Additionally, patients who require radical cystectomy have a high burden of risk, with a mean age at presentation of 73 years, a median of 8 chronic conditions, malnutrition rates ranging from 16-55%, sarcopenia in up to 69%, and frailty in 4-70%
The main problem we face in this population with a very high burden of risk is how we can improve outcomes for these vulnerable patients. We should take a proactive approach to optimizing patients with bladder cancer through prehabilitation.
Prehabilitation is a process of improving the functional capability of a patient prior to a surgical procedure/medical treatment so we increase the ability of the patient to withstand postoperative inactivity and treatment-associated functional decline.
The goal of prehabilitation is to identify modifiable risk factors and optimize the status of the patient to improve:
- Candidacy for treatment
- Post-treatment Outcomes
- Return to/better baseline
For these we should focus on three main pillars: physical, mental and nutritional as illustrated below:
Prehabilitation before surgery is associated with numerous benefits, including fewer complications, shorter hospital stays, improved body composition parameters, and lower costs. Additionally, patients often experience an enhanced quality of life and sustained improvements in mental health. These benefits are particularly pronounced when personalized prehabilitation interventions are implemented, tailoring the approach to the individual needs of each patient.1
Dr. Psutka moved on to discuss the 'Nuts and Bolts of Prehab' and the steps to starting a prehabilitation program. The first step, as outlined, is to build a multidisciplinary team. This team should include a physiatrist, physical therapist, pelvic floor muscle therapy specialist, occupational therapist, neuropsychologist, and nutritionist. Collaboration among these professionals is essential for developing a comprehensive and effective prehabilitation program.
The second step is to identify the specific problems that need to be addressed by characterizing a patient's risk profile. A critical point in this process is that a prehabilitation plan should start with a data-driven comprehensive risk assessment.
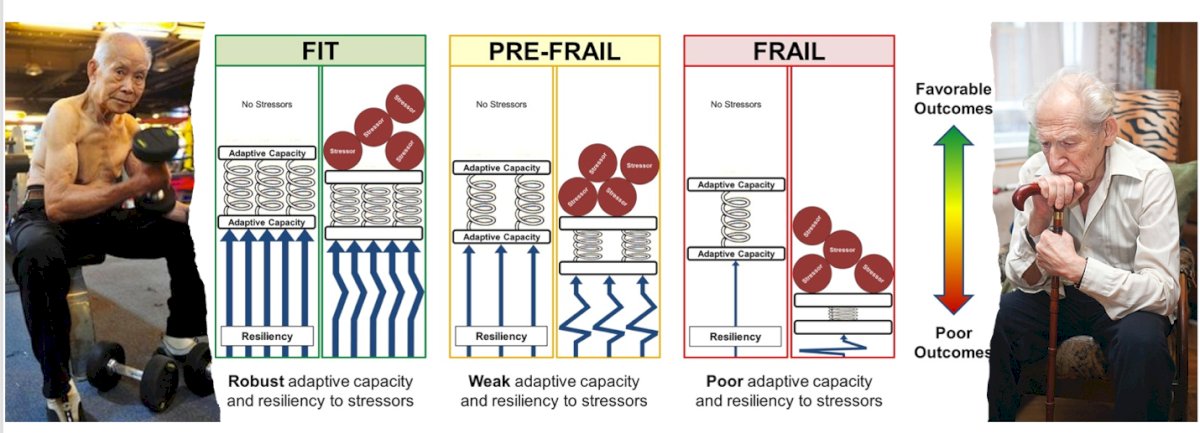
Dr. Psutka provided an example illustrating how different risk and reserve profiles can lead to varying outcomes when faced with the same level of stress, affecting the ability to withstand and recover from surgery.
There are a wide array of tools available for frailty screening, including the Vulnerable Elders Survey-13 (VES-13), the Geriatric-8 (G-8) questionnaire, and other tools such as the Abbreviated Comprehensive Geriatric Assessment (CGA), Fried Frailty Criteria, Groningen Frailty Index, and the Senior Adult Oncology Program assessment. Additionally, a simple yet effective screening question is, 'Have you fallen in the past three months?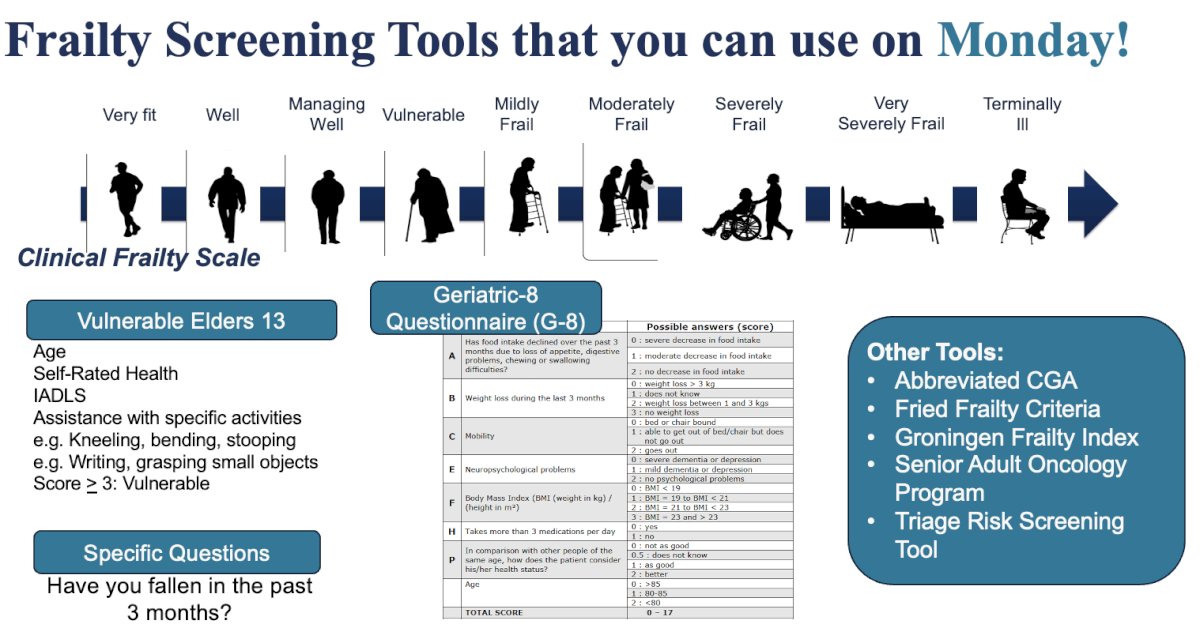
The problem is that simply identifying 'frailty' does not provide an actionable target. Dana Cavanaugh explored correlations between different domains of geriatric assessment and found that each data point offers discrete and valuable information about each patient, helping us understand why they are frail, how they are frail, and how we can improve their condition. However, the correlation between different domains is low for most patients.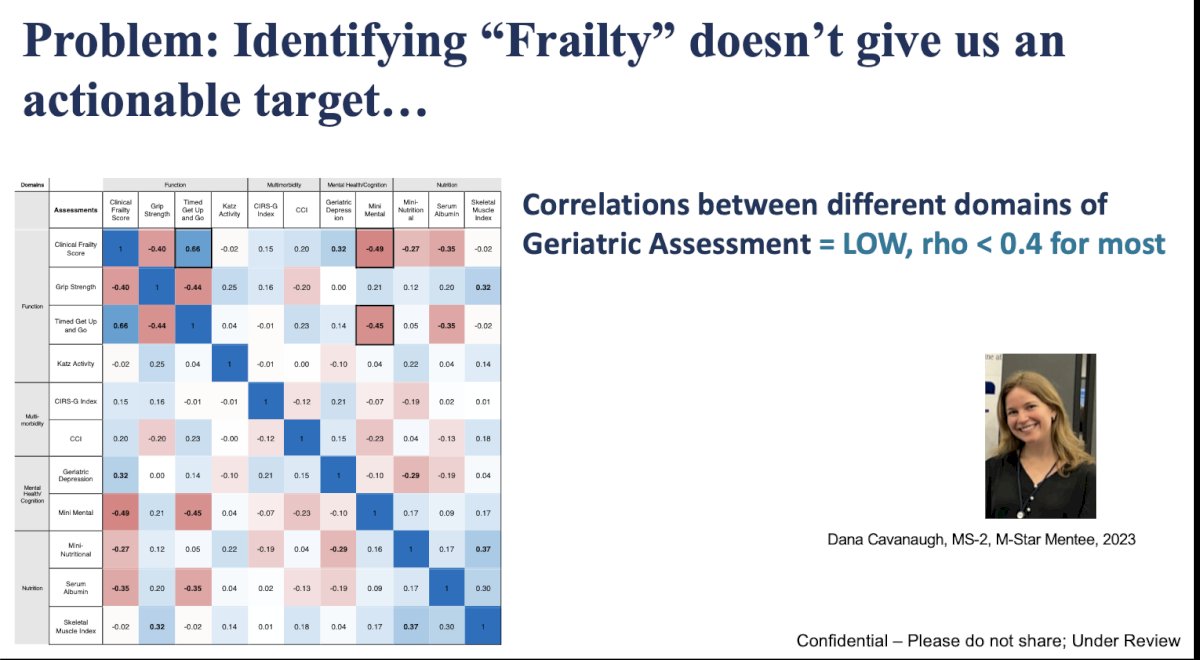
SIOG, NCCN, ASCO, and EAU guidelines recommend the use of comprehensive geriatric assessment (GA) for all patients aged 70 years or older receiving treatment. The results of GA should be applied to develop an integrated and individualized plan that informs treatment recommendations and selection and estimates risks for adverse outcomes.
Dr. Psutka discussed that a better way to characterize risk and resources is through a Comprehensive Geriatric Assessment, which involves a multidimensional evaluation (figure below) of a patient's health. This approach can identify potentially modifiable risk factors to improve outcomes. The goal is to enhance the assessment of biological and functional age while identifying actionable needs. However, it is not commonly used in urologic practice due to challenges such as time constraints, limited resources, and lack of education or awareness.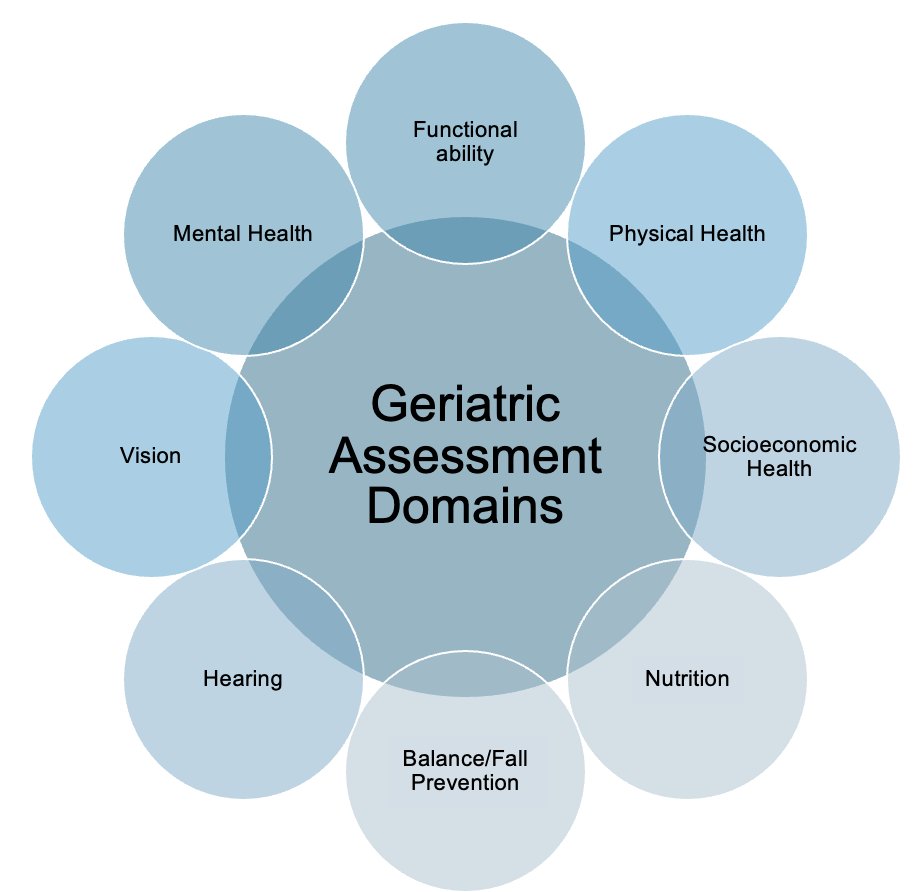
- 0-0.2 = Robust
- 0.2 – 0.35 = Pre-Frail
- >0.35: Frail
In addition, the Short Physical Performance Battery (SPPB) is a very practical tool that takes less than 4 minutes, requires no equipment, and includes tests such as a 10-second balance test (standing, tandem, tightrope walk), a 3–4-meter gait speed test, and five repetitions of the sit-to-stand movement. This further emphasizes that functional age, rather than chronological age, is key to identifying actionable needs.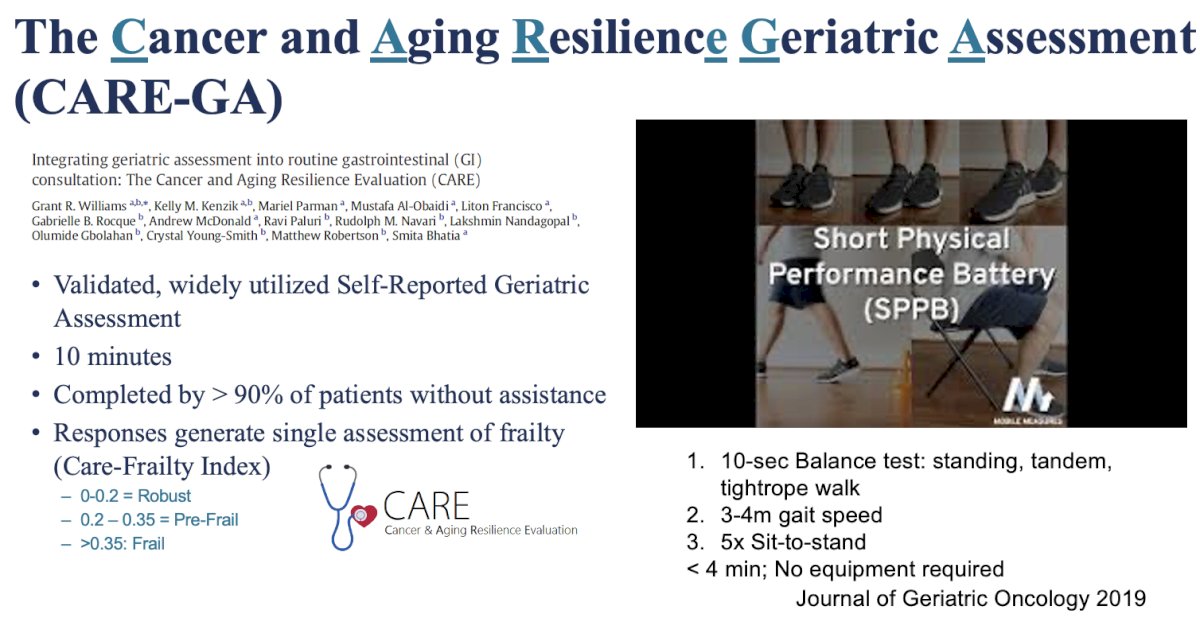
Prehabilitation should focus on identifying both strengths and resources, as well as vulnerabilities and risks. By doing so, we can bolster resources and mitigate vulnerabilities. Strategies should be developed to mitigate personalized risk profiles, using Geriatric Assessment-based, vulnerability-directed prehabilitation prescriptions.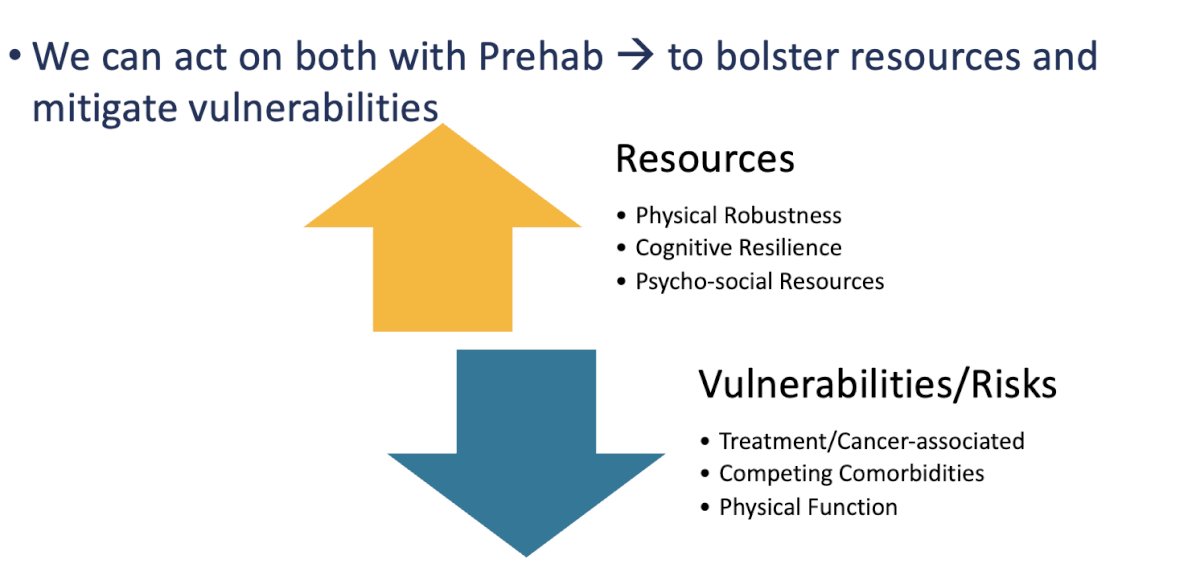
Below is a comprehensive list of vulnerability-directed interventions before, during, and after treatment that we should consider when evaluating our bladder cancer patients: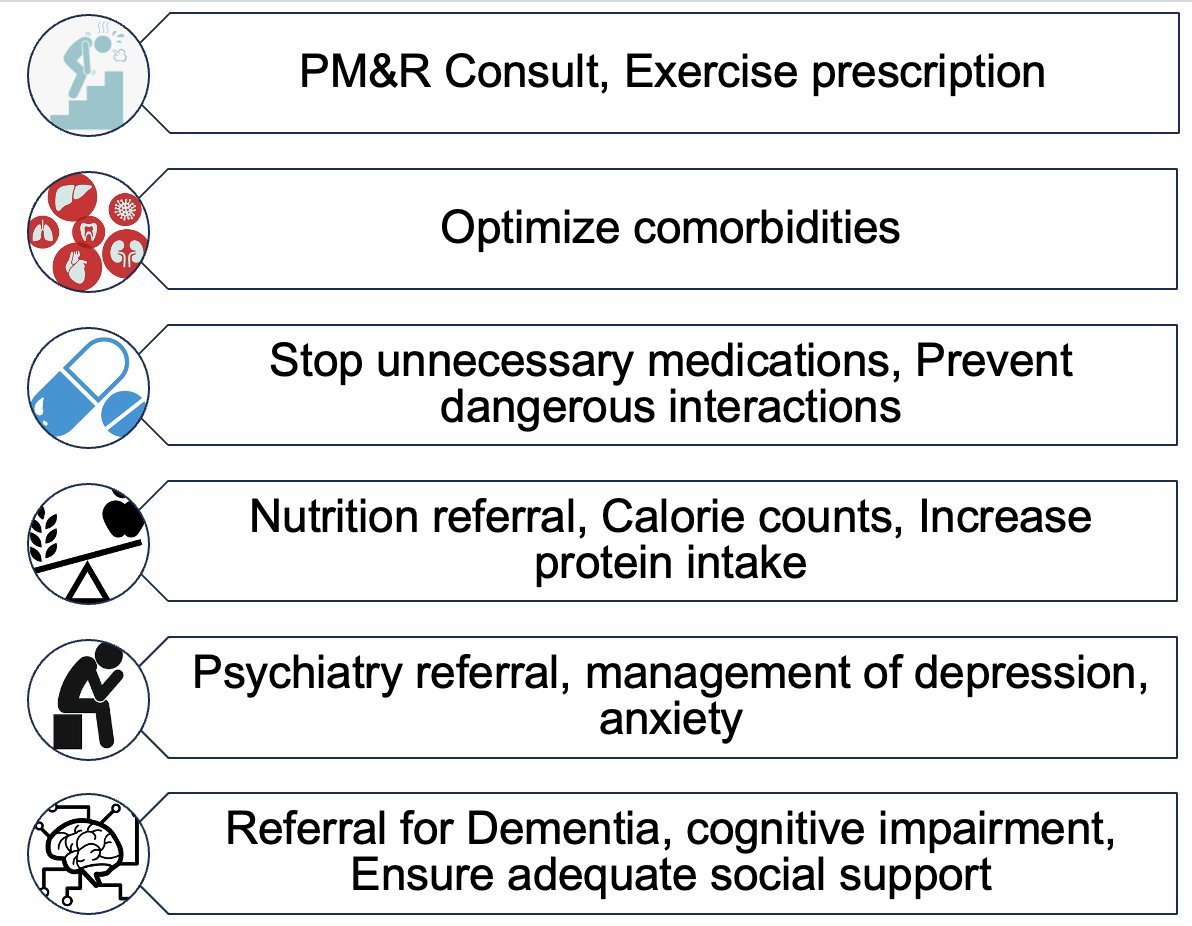
In terms of exercise prescriptions, the ASCO guideline recommends that oncology providers advocate for both aerobic and resistance exercise during active treatment to mitigate the side effects of cancer therapy. This is highly beneficial for us as healthcare providers, and we should all strive to be more active. Exercise improves cardiovascular health, bone health, fatigue, sleep, functional status, and anxiety/depression, while also decreasing the risk of falls. This is crucial to help our patients withstand the physiological stress of prolonged anesthesia and surgical trauma.
Dr. Pstuka discussed that there are four P’s of prehabilitation:
- Personalized
- Pragmatic
- Preparation
- Pacing
When we prescribe exercise as medicine, it’s important to personalize the exercise prescription by assessing factors such as the type of exercise, frequency, intensity, and potential side effects. Every time we give a prescription, we should ask ourselves these questions, and the same approach applies to prehabilitation. For example, if I’m performing a midline incision, I need to focus on bolstering the patient’s core strength to facilitate easier recovery. Exercises in prehab should focus on general conditioning and impairment-specific strength training and this conditioning exercises should be manageable on good days and bad days.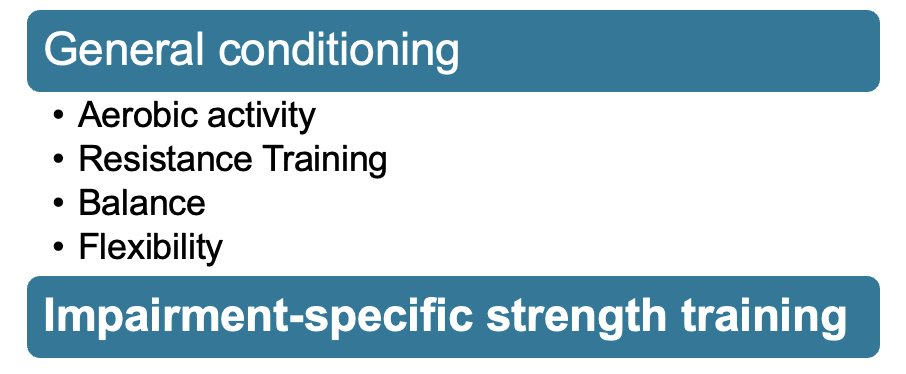
Moreover, nutrition is a crucial pillar of prehabilitation. We should detect nutritional deficiencies early through nutritional screening, with routine evaluation of intake, weight changes, and BMI. If malnutrition is identified, patients should be referred for formal nutritional consultation. Protein is vital for maintaining muscle mass, with a recommended intake of 1 to 1.5 g/kg/day for patients.
Specialized immunonutrition (SIM), also known as pharmaconutrition, uses ingredients such as arginine, omega-3 fatty acids, glutamine, and nucleotides. SIM has been shown to improve postoperative outcomes by enhancing immune and inflammatory responses, protecting muscle mass, promoting wound healing, and reducing complications, particularly ileus and infection. It has demonstrated a 33% reduction in postoperative complications and a 39% reduction in infections. However, many patients cannot afford expensive nutritional supplements. Dr. Viraj Master and Dr. Psutka highlighted a cost-effective alternative, available on the website FrailPatient, where a shake can be prepared for less than 3 dollars and has proven to be very effective.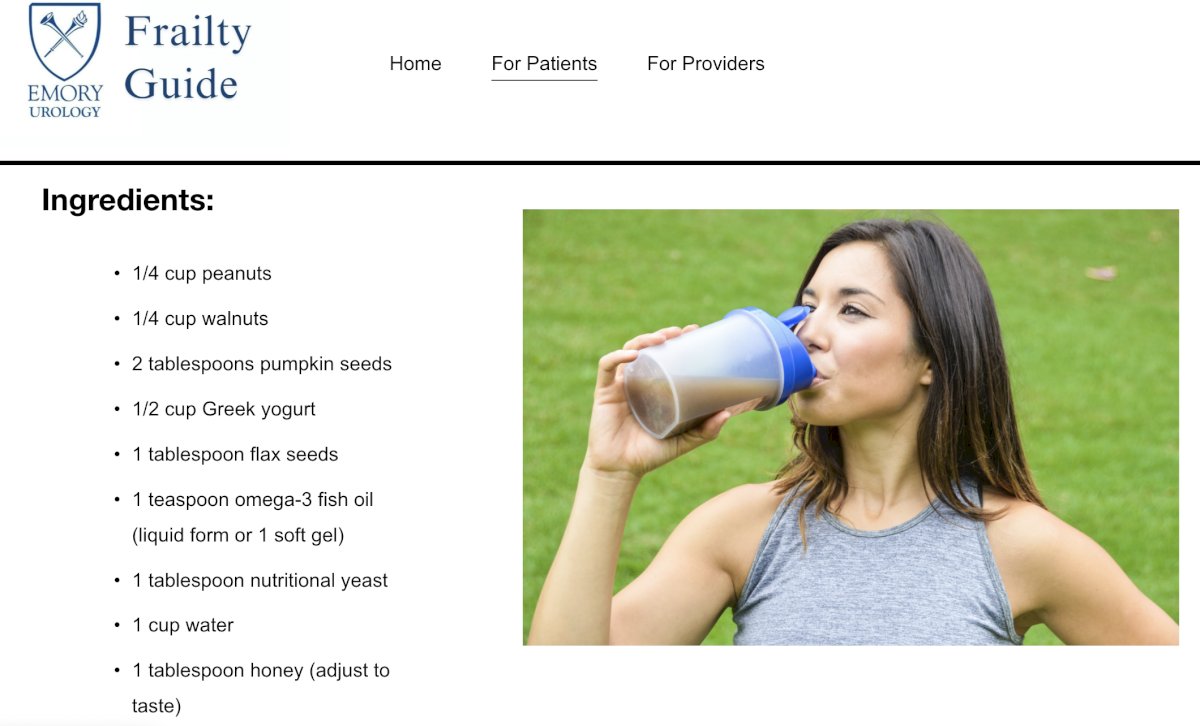
Lastly, cognitive prehabilitation is very important. There are multiple factors that impact cognitive functioning in patients undergoing cancer treatment, as illustrated in the graphic below: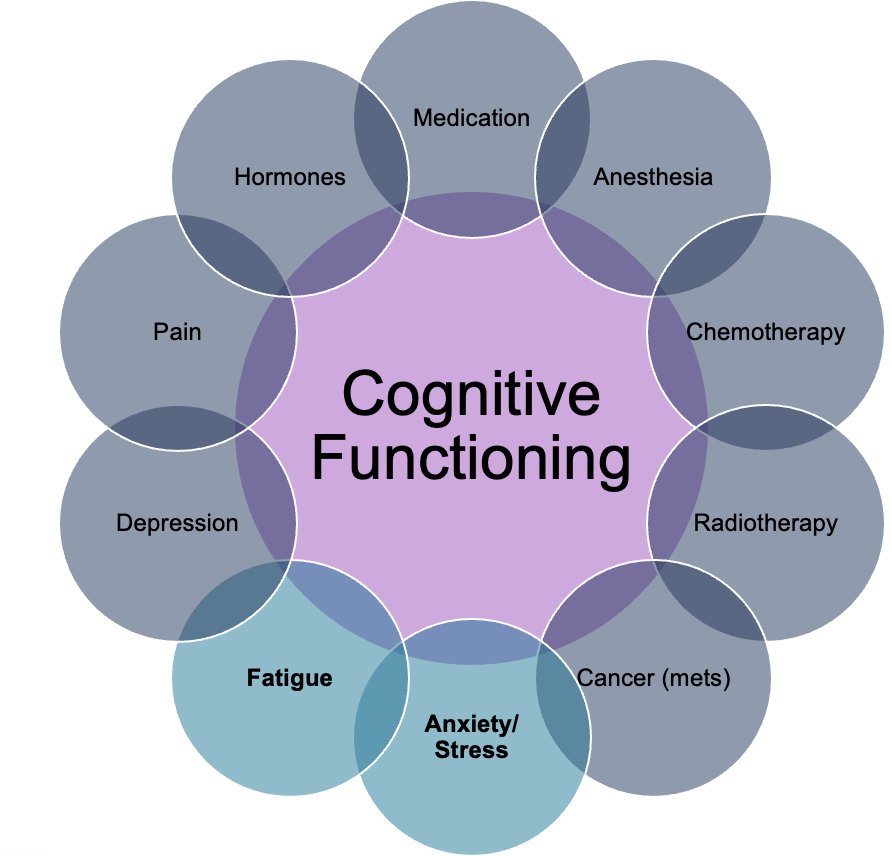
When aiming to improve cognitive function in patients, two main strategies are effective: restoration and compensation. Restoration focuses on improving or restoring natural cognitive abilities through brain and mental training exercises. Compensation, on the other hand, aims to minimize the interference of cognitive difficulties in daily life by using tools like alarms, calendars, to-do lists, and routines, as well as creating a central memory station for essential items such as keys and phones. Compensation strategies have been shown to enhance real-world cognitive function more effective.
Lastly, stress and fatigue management strategies play a critical role in improving patient outcomes. These strategies include diaphragmatic breathing, paced breathing, and other relaxation techniques to reduce stress. Meditation and mindfulness practices can help enhance mental clarity and focus, while yoga and chair yoga provide gentle physical activity to support both physical and emotional well-being. Regular physical activity is crucial for improving overall stamina and mood. Additional treatments, such as psychotherapy, can address emotional health, while sleep hygiene strategies promote restful and restorative sleep. Incorporating these approaches into the prehabilitation plan can significantly improve resilience and recovery during the treatment process.
The next steps in prehabilitation science, we need to work in four areas that we are falling a little bit short and we need them to Develop a prehab program: Availability, effect, pragmatism, and cost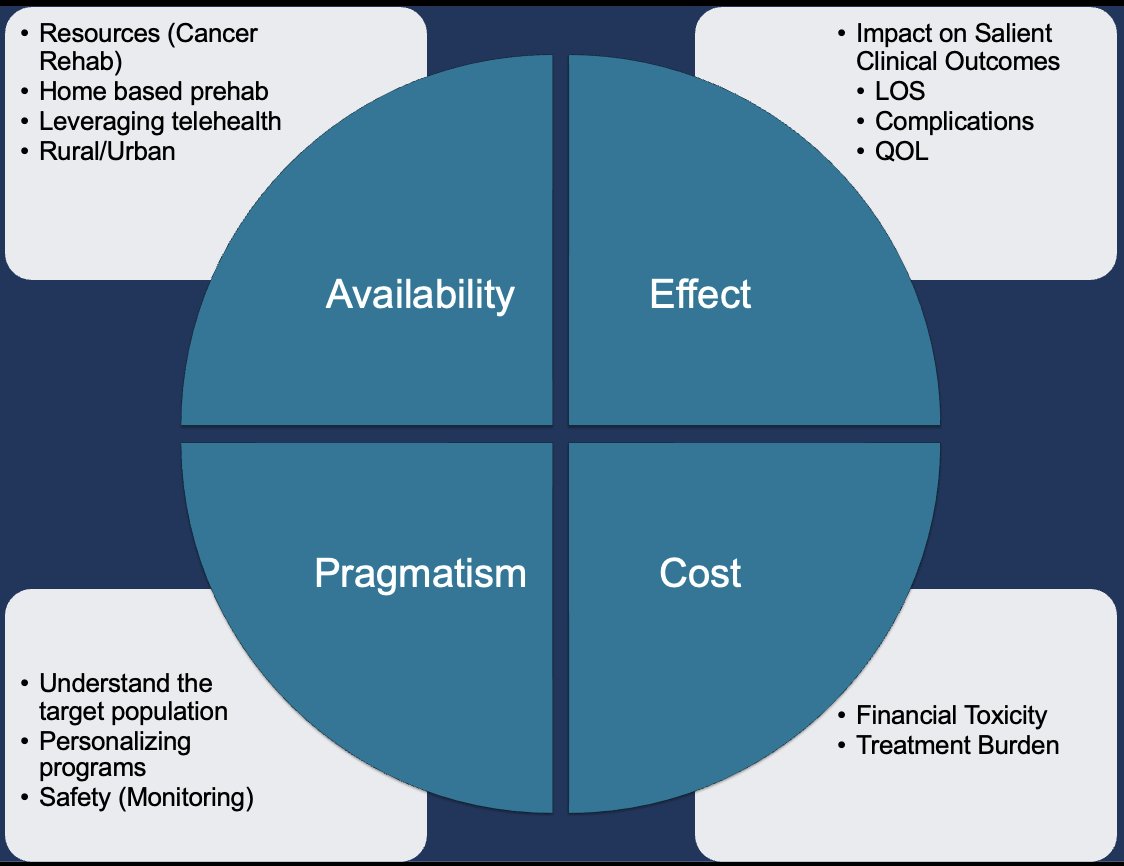
She emphasized that while many strategies have been tested, there is a need for more pragmatic and simplified approaches to prehabilitation. This includes personalized programs tailored to individual needs, supervised home-based exercises, and the incorporation of wearable devices to track progress. Additionally, bringing artificial intelligence into prehab could help optimize treatment plans and improve patient outcomes through data-driven insights. These approaches could make prehabilitation more accessible, pragmatic, and effective for patients.
Dr. Psutka briefly discussed the ENHANCE trial conducted in Belgium, which randomized 154 patients into a control group and an intervention group. The intervention group received an enhanced treatment approach, which included augmenting existing ERAS (Enhanced Recovery After Surgery) pathways with additional components such as nutritional support, psychological counseling, smoking cessation, a supervised physical therapy training program, and integration of neurocognitive and mindfulness activities. This comprehensive approach aimed to improve overall patient outcomes by addressing physical, psychological, and cognitive aspects of recovery.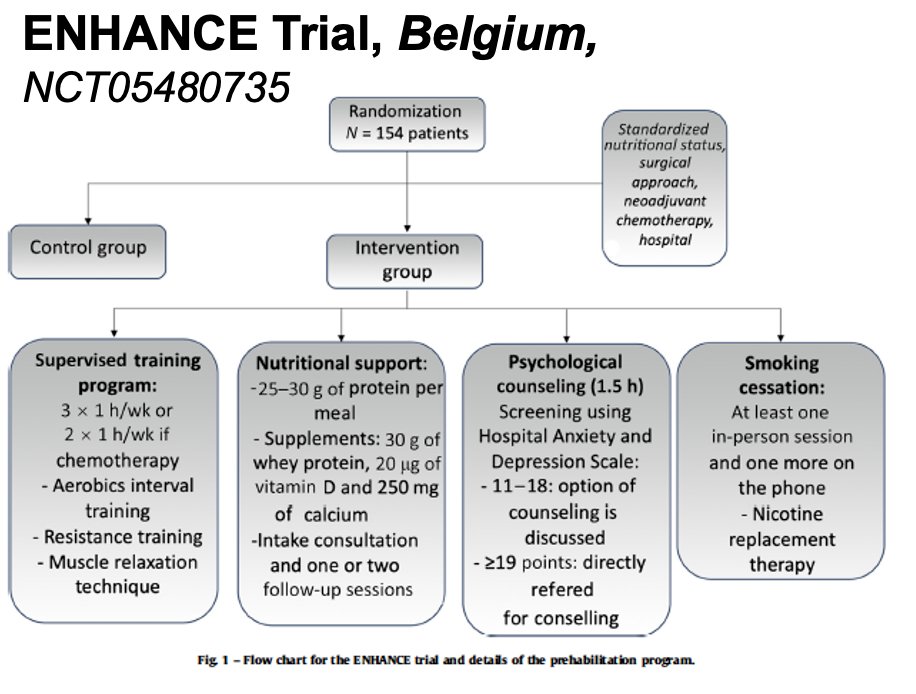
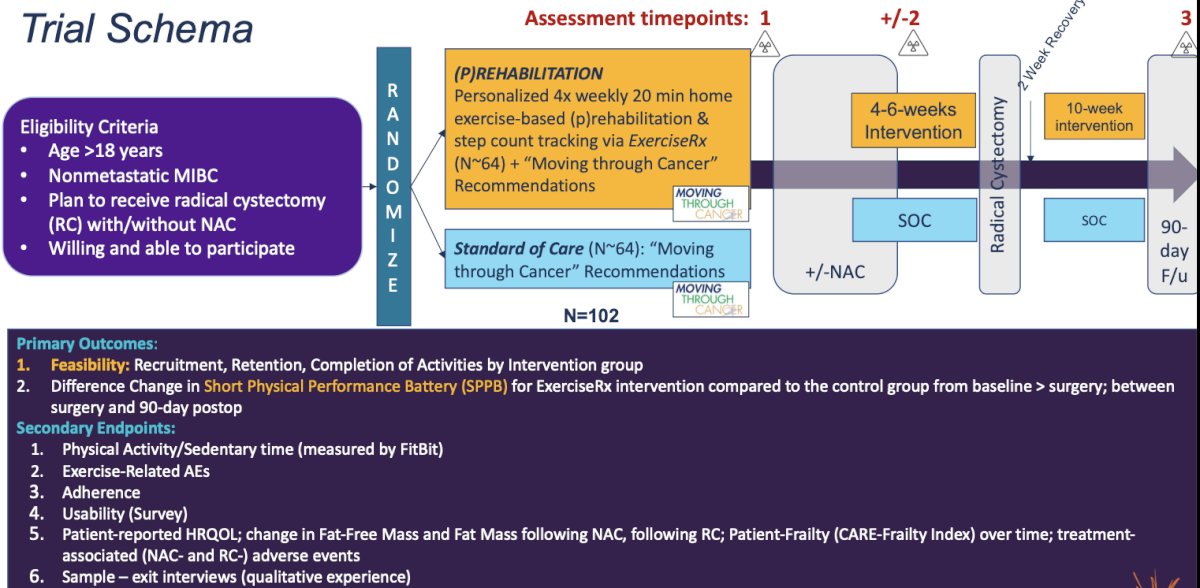
The GetMoving trial is a Phase I/II randomized controlled trial evaluating home-based prehabilitation (PRehab) with ExerciseRx in patients with localized urothelial cancer undergoing surgery. The trial is currently ongoing, and its primary outcomes include feasibility measures such as recruitment, retention, and completion of activities by the intervention group. Additionally, the trial will assess the difference in the change of Short Physical Performance Battery (SPPB) scores between the ExerciseRx intervention group and the control group, both from baseline to surgery and between surgery and 90-day postoperative follow-up. This study aims to evaluate the impact of home-based exercise interventions on patient physical performance in the perioperative period.
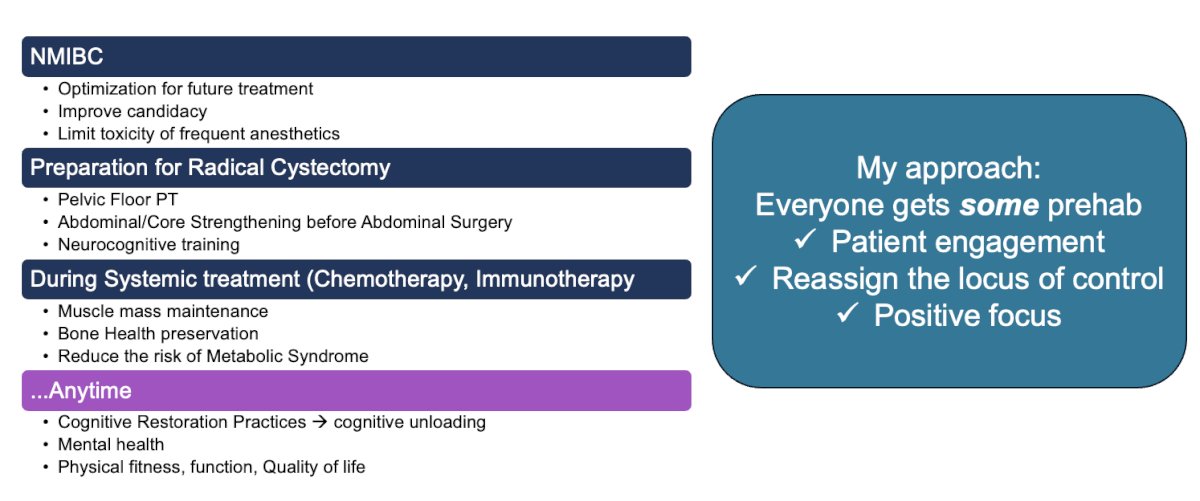
Dr. Psutka emphasizes that prehabilitation can benefit all patients, not only older individuals or those with baseline frailty. She advocates for incorporating prehabilitation into the care of all patients undergoing cancer treatment. She presented her approach, in which prehabilitation is provided universally across the spectrum of bladder cancer care. Rather than reserving it for those with specific risk factors, her approach ensures that every patient receives some form of prehabilitation, focusing on improving physical, nutritional, and cognitive health to optimize treatment outcomes, enhance recovery, and improve quality of life throughout the treatment process.
Dr. Psutka concluded her presentation with the following conclusions:
- Prehabilitation requires a personalized approach, assessing both the resources and vulnerabilities of each patient, rather than using a one-size-fits-all strategy.
- Prehabilitation offers significant potential benefits for patients, including improving engagement, candidacy for treatment, overall well-being, and ultimately, better outcomes.
- Prehabilitation should be multifaceted, involving various disciplines and approaches, to address the comprehensive needs of the patient.
- Prehabilitation can benefit all patients, not just those who are frail or older. It provides positive impacts before and after treatment.
- For prehabilitation to be effective, it needs to be accessible, scalable, and pragmatic while still maintaining its effectiveness.
Presented by: Sarah Psutka, MD, MSc, Associate Professor of Urology in the Department of Urology at the University of Washington and Fred Hutchinson Cancer Center
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:- Briggs LG, Reitblat C, Bain PA, Parke S, Lam NY, Wright J, Catto JWF, Copeland RJ, Psutka SP. Prehabilitation Exercise Before Urologic Cancer Surgery: A Systematic and Interdisciplinary Review. Eur Urol. 2022 Feb;81(2):157-167. doi: 10.1016/j.eururo.2021.05.015. Epub 2021 May 29. PMID: 34074558.


