(UroToday.com) The 2024 SUO annual meeting included a session on smoking cessation, vaping, and e-cigarettes, featuring a presentation by Dr. Richard Matulewicz discussing implementing smoking cessation in the urologic oncology setting. Dr. Matulewicz started by emphasizing that we know that smoking either causes or exacerbates the severity of several urologic cancers, mostly notably kidney and bladder cancer.
The population attributable risk, which is defined as the percentage of bladder cancer cases that are caused directly from smoking, is approximately 50%. Compared to never smokers, those who are current or former smokers may be at a 2-5x greater risk of developing kidney and bladder cancer. Similarly, patients treated for prostate cancer that smoke have an increased risk of recurrence. Of note, the effect of smoking on urologic cancers is getting worse and is likely secondary to changes in the composition of cigarettes over time, despite lower tar content and the lower overall prevalence of smoking. Even among testicular cancer survivors, the 10-year overall survival is 92% in never smokers compared to 83% for current smokers (p < 0.005), with an age-adjusted hazard ratio for death of 1.85 (95% CI 1.29-2.66; p = 0.001):1
Cinciripini et al.2 recently published their assessment of the association between time of entry into a smoking cessation intervention following a cancer diagnosis and survival outcomes. This was a prospective cohort study design of patients with cancer who smoked and received cessation treatment who were assessed at 3 months, 6 months, and 9 months following tobacco treatment onset. Cessation treatment consisted of 6-8 personalized counseling visits and 10-12 weeks of pharmacotherapy, with the majority of visits (95%) provided via telemedicine. Among 4,526 currently smoking patients, survival over 15 years increased for those quitting smoking at 3 months (aHR 0.75, 95% CI, 0.67-0.83), 6 months (aHR 0.79, 95% CI, 0.71-0.88), and 9 months (aHR 0.85, 95% CI, 0.76-0.95) of follow-up. Notably, optimal survival outcomes were observed for patients who received tobacco treatment within 6 months of a cancer diagnosis. At the 75th percentile, their survival increased from 2.1 years among continuing smokers versus 3.9 years for patients who quit: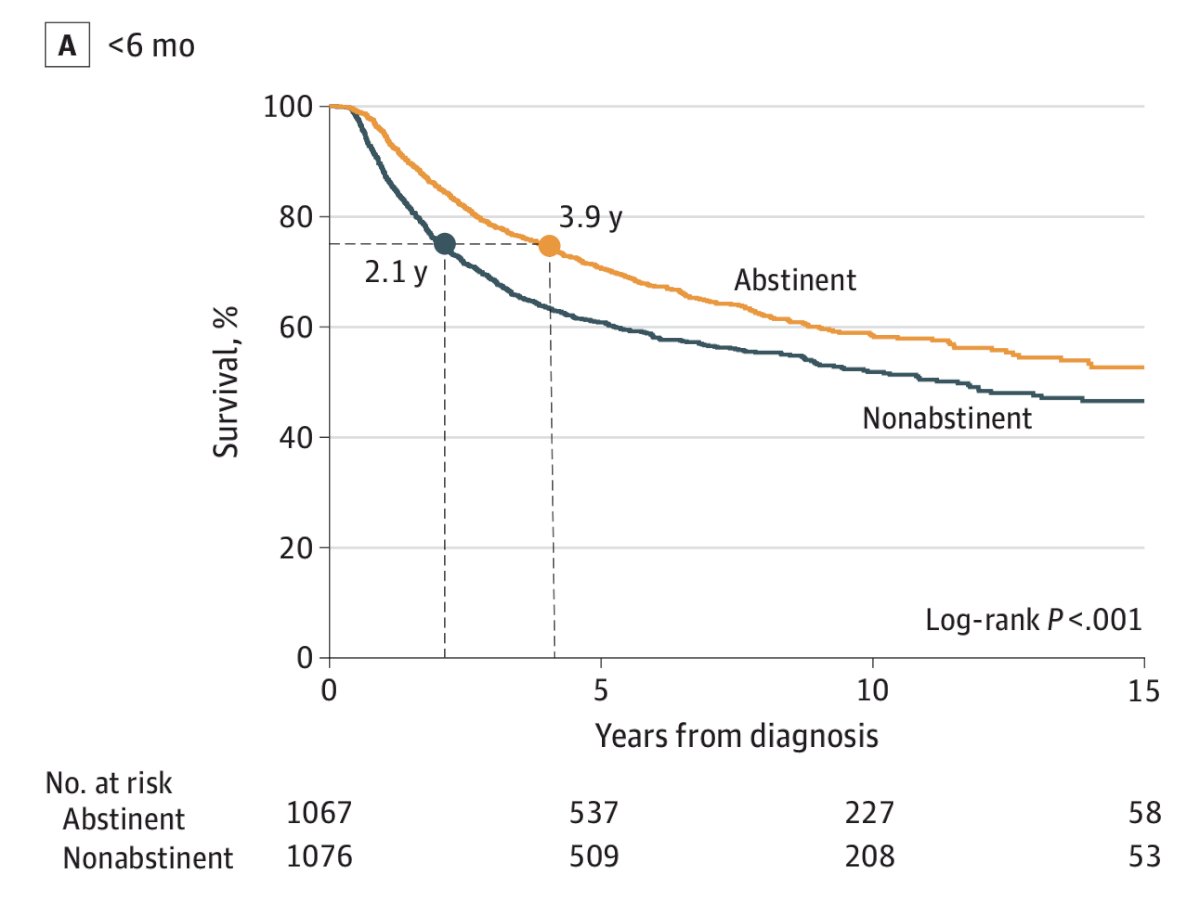
It is also important to note that smoking cessation improves many outcomes. This is most widely studied in bladder cancer, but we do know that smoking cessation is now widely recognized, in addition to surgery, systemic therapy, and radiation, as the fourth pillar of cancer care. As such, nearly all accrediting bodies recommend smoking cessation as an integral component of cancer care for all patients who smoke. Additionally, promoting smoking cessation reduces cost of care: there is a ~$3.4 billion incremental cost of treating cancer failures associated with continued smoking among patients with cancer in the US each year.
Dr. Matulewicz emphasized that there is ample opportunity to intervene with smoking cessation for our patients. One third of all visits with urologists are for tobacco-related disease. In fact, work from Dr. Matulewicz’s group suggests that 1.3 million visits occur to urologists per year of which patients are active smokers:3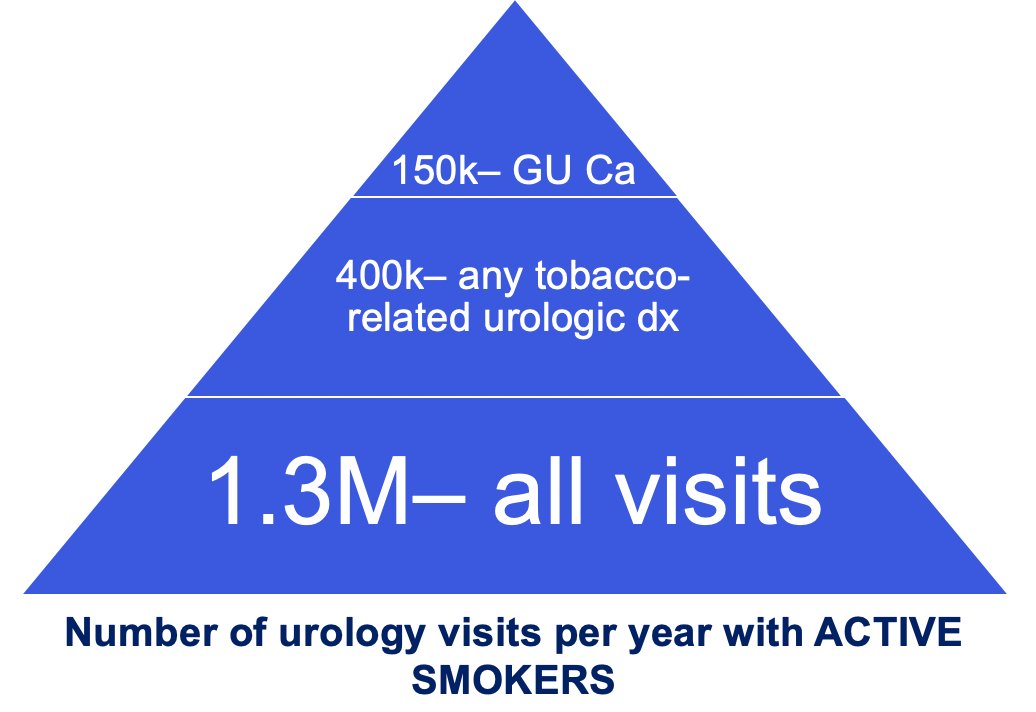
So, why don’t patients quit smoking? Dr. Matulewicz notes several hypotheses:
- Patients are generally unware about the connection between genitourinary cancers and smoking
- Education and physician (especially urologists) advice is helpful, but…
- Urologists are not doing their part in the outpatient or inpatient setting
- Accordingly, patients are not getting evidence-based treatment
Indeed, there is a profound lack of awareness of among patients. Work from Dr. Matulewicz’s group used the Population Assessment of Tobacco and Health (a longitudinal nationally representative survey) to ascertain that among the weighted estimate of 44 million US adult smokers, people are markedly less aware of the connection between smoking and bladder cancer than other prevalent smoking-related disease such as lung cancer, mouth cancer, or heart disease:4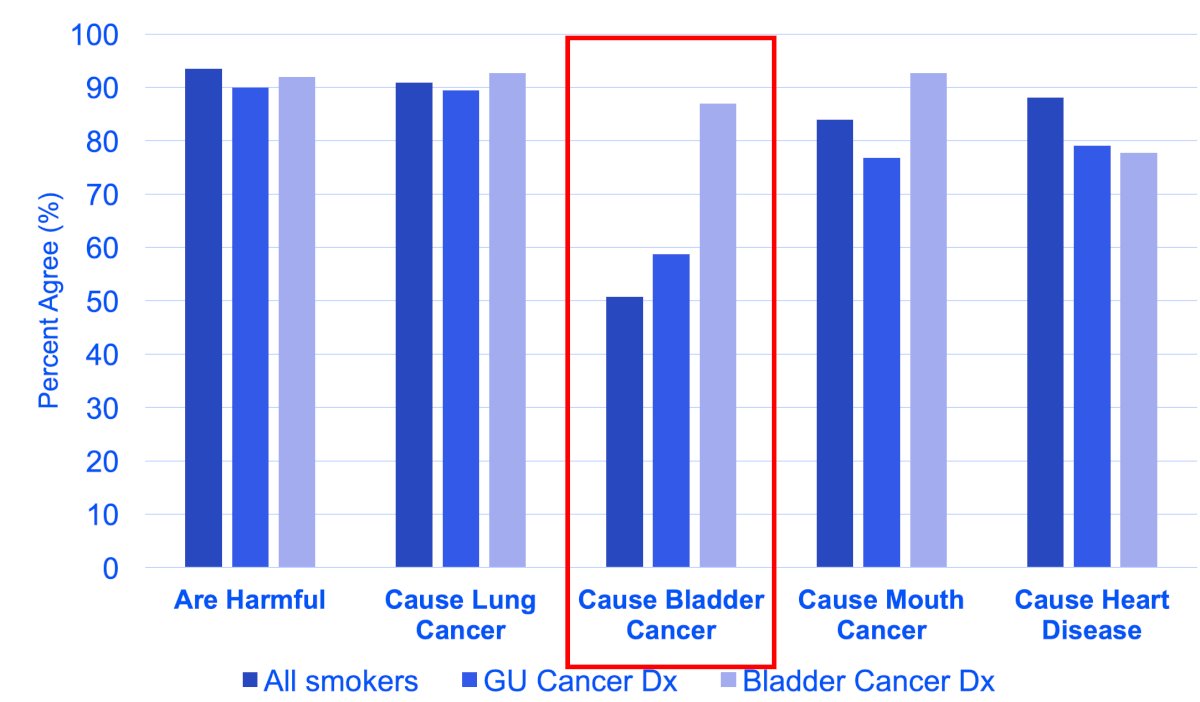
When they asked the same questions among patients who had a history of genitourinary cancer (and presumably those who had seen a urologist to tell them to quit smoking), the perceptions of harm where more congruent, but there were still significant knowledge gaps. To assess what urologists think of smoking cessation, Dr. Matulewicz and colleagues used the 2021 AUA census5 to assess responses from 1,742 urologists were weighted to represent the practicing adult urologist population (n = 12,852) in the US. Overall, although 98% of urologists agree that tobacco use contributes to urologic disease, only 58% agree that assessment/treatment by urologists is important. Moreover, they found significant variation in agreement among physician demographics/training and practice settings (location, type, ancillary staff support). Most urologists would like to “offload” to experts after advice to quit, noting that barriers include time, reimbursement, and lack of training/experience: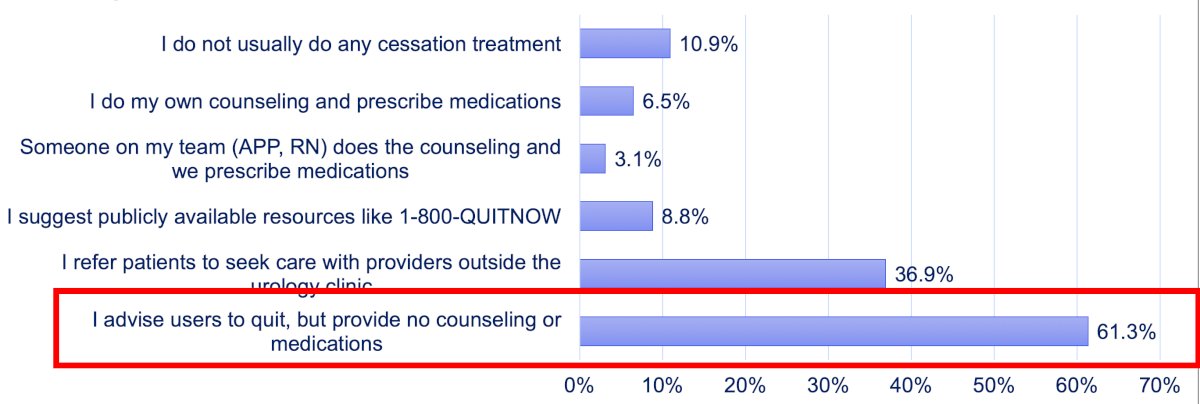
Importantly, a urologists’ advice is influential and patients listen to and are more likely to quit or attempt to quit if told to do so. Knowing that smoking is related to their diagnosis motivates quit attempts. In a study in collaboration with UCLA, Dr. Matulewicz and colleagues asked ~400 patients from the California Cancer Registry about sources of information, perceptions, and quit behaviors around the time of their bladder cancer diagnosis and compared them to population matched controls in the California Tobacco System. Urologists were the most trusted and utilized sources of information regarding the cause and smoking-related nature of the patient’s bladder cancer diagnosis: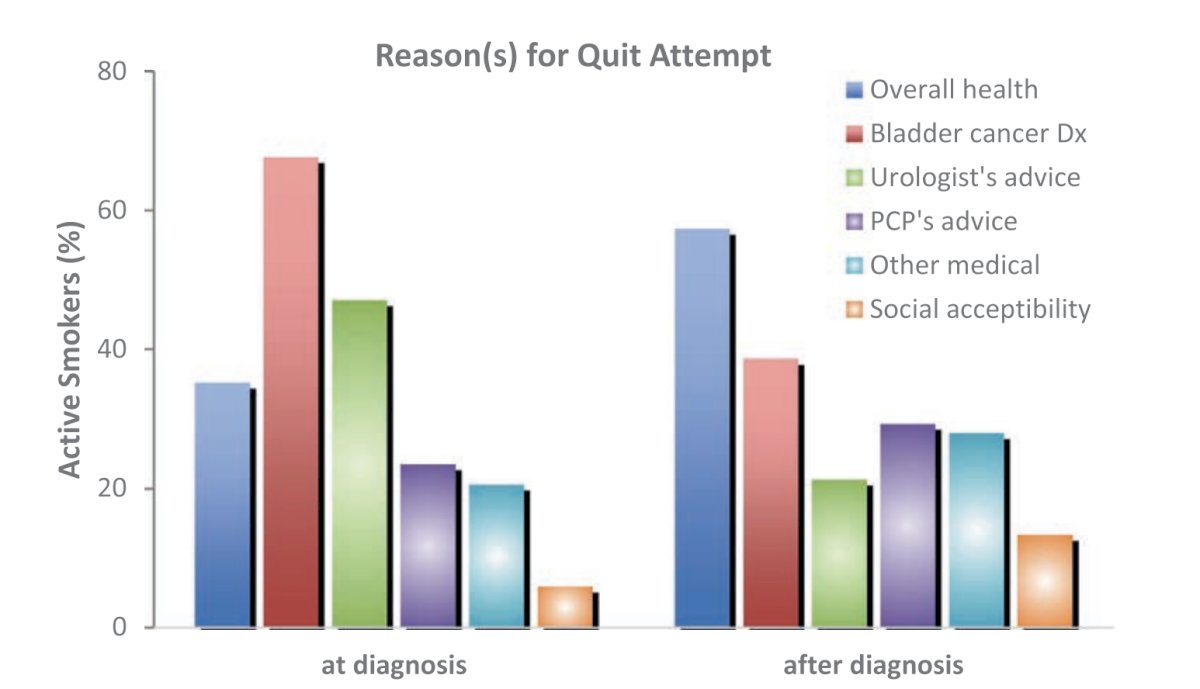
Additional findings from this study was that compared to population controls, smokers with bladder cancer were 5x more likely to quit than the general population.
How do we approach improvement? Although ideally interventions would take place along the entire continuum of medical care, when it comes to preventative medicine, the focus of urologists is on the secondary and tertiary prevention stages: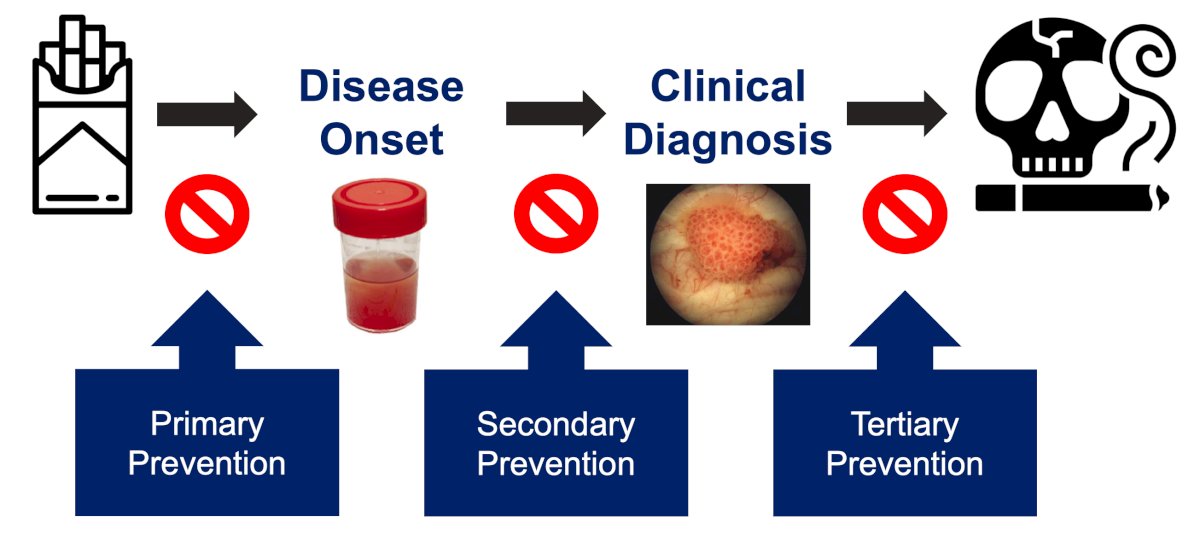
One framework for delivering care is the AAR “Ask, Advise, Refer” model for tobacco cessation: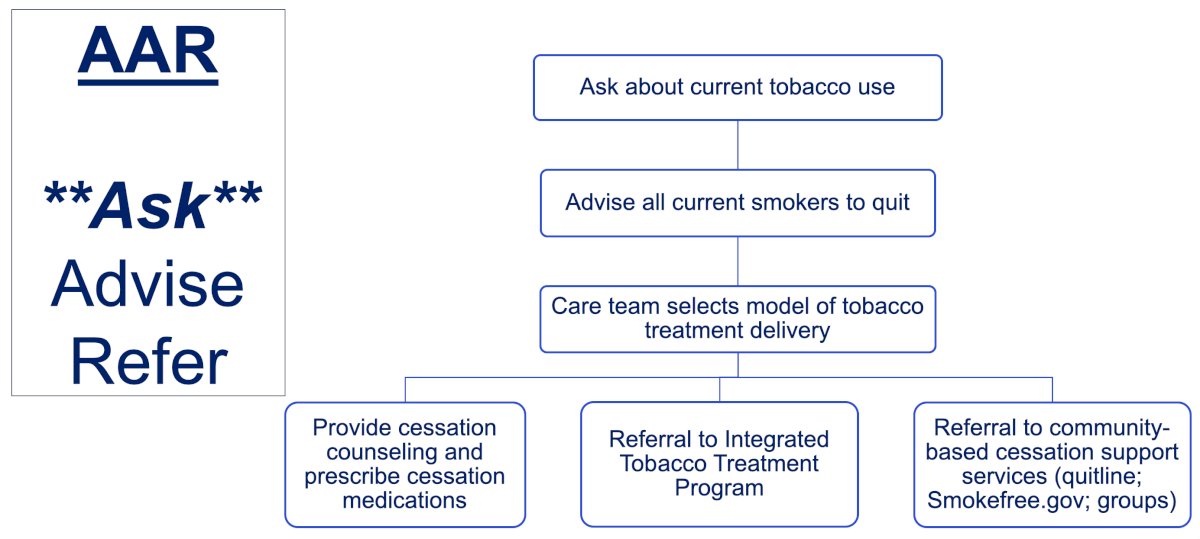
Dr. Matulewicz emphasized that when determining when tobacco cessation can be done, it is important to (i) assess your own institutional practices, and (ii) identify resources at the system level. For patients with urothelial carcinoma, there are five specific targeted intervention points for counseling patients:7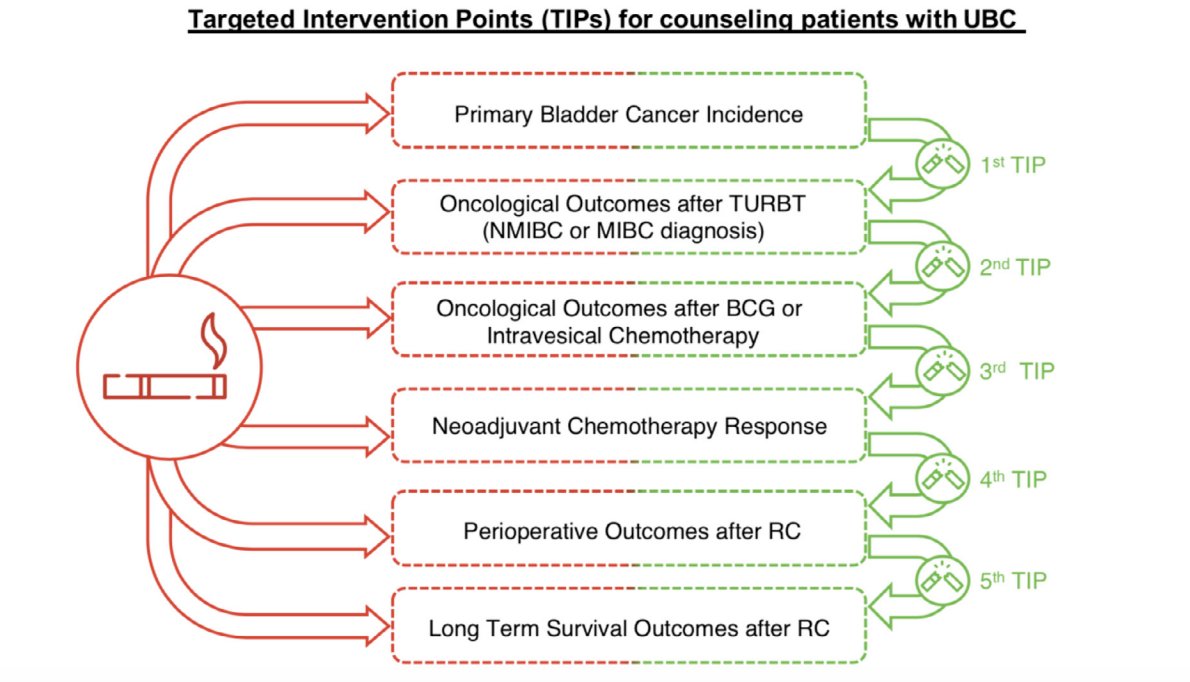
Undoubtedly, the biggest key is to ask the patient about quitting tobacco. This can be done via screening protocol by the MA/RN in the clinic and can be included during the vital signs assessment. Alternatively, it can be done as part of the intake summary/survey (EPIC “MyChart” in the waiting area) and can be integrated into pre-surgical testing.
If a urologist’s advice is important and education is critical, taken together with most patients wanting to quit, how are we doing as clinicians? The first step in tobacco cessation treatment is screening. In their study assessing tobacco screening and treatment during outpatient urology office visits in the United States,3 Dr. Matulewicz and colleagues used a national data set to provide population-estimates of outpatient clinic practices for urologists. Among an estimated 64 million outpatient urology visits over a 3 year period, they found that urologists are often screening, but there was considerable variation in physician-level practice: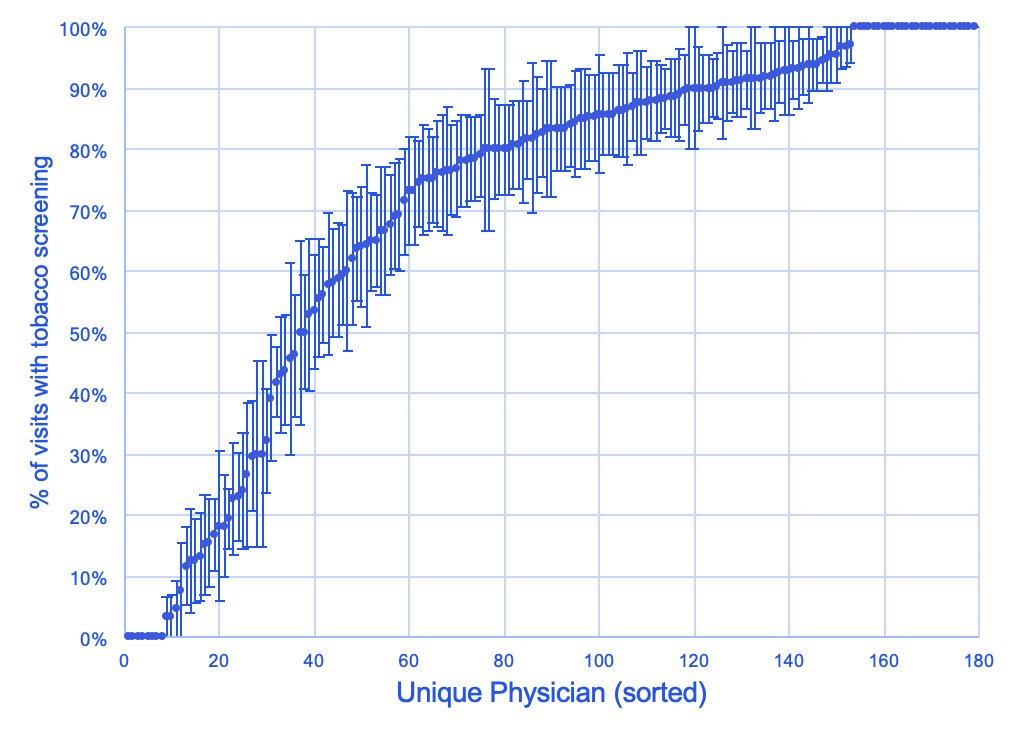
What is not happening is treatment initiation and facilitation after screening takes place.
ADVISE
Advising patients should be made part of the counseling process in a “motivational interviewing” type format. This can be integrated into the treatment plan and phrased to the patient as “part of your cancer/disease treatment plan.” For patients that are prepping for surgery, tobacco cessation can be used as motivation for a quit date. From a billing perspective, Dr. Matulewicz has created “dot phrases” for his tobacco cessation counselling. For example “I spent an additional 10 minutes counseling the patient about the importance of smoking cessation, discussing the role of pharmacotherapy and behavioral counseling, and providing resources - both public (1-800-QUIT-NOW) and private (MSK Tobacco Treatment Program). I discussed the important of smoking cessation on perioperative outcomes as well as the benefits in cancer specific and overall survival. I placed an order for referral to our TTP here at MSK and reiterated the importance of getting involved with this program. The patient is motivated to quit and has determined they wish to quit before their upcoming procedure on XYZ.” The corresponding billing codes are as follows: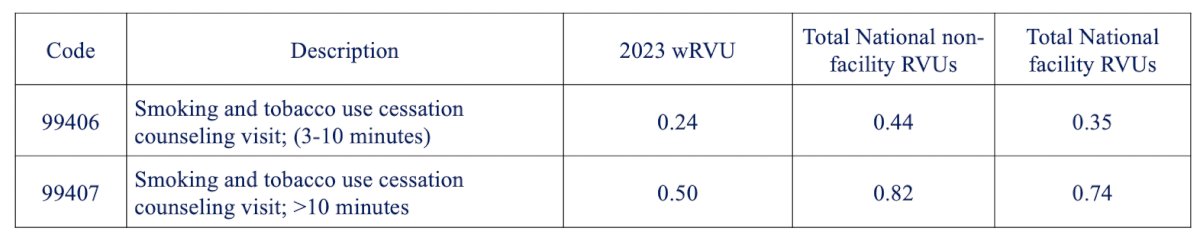
REFER
Referrals should ideally be made for local assistance, but if not feasible, public health services are the next best option. Dr. Matulewicz also notes that it is also not unreasonable for the urologist to write the tobacco cessation medications. Importantly, we must always follow up and ask how cessation is going at the next clinic visit. The NCCN Clinical Practice Guidelines in Oncology states that smoking cessation should include counseling/behavioral + pharmacotherapy:
Dr. Matulewicz also listed several cessation support partners for everyday practice: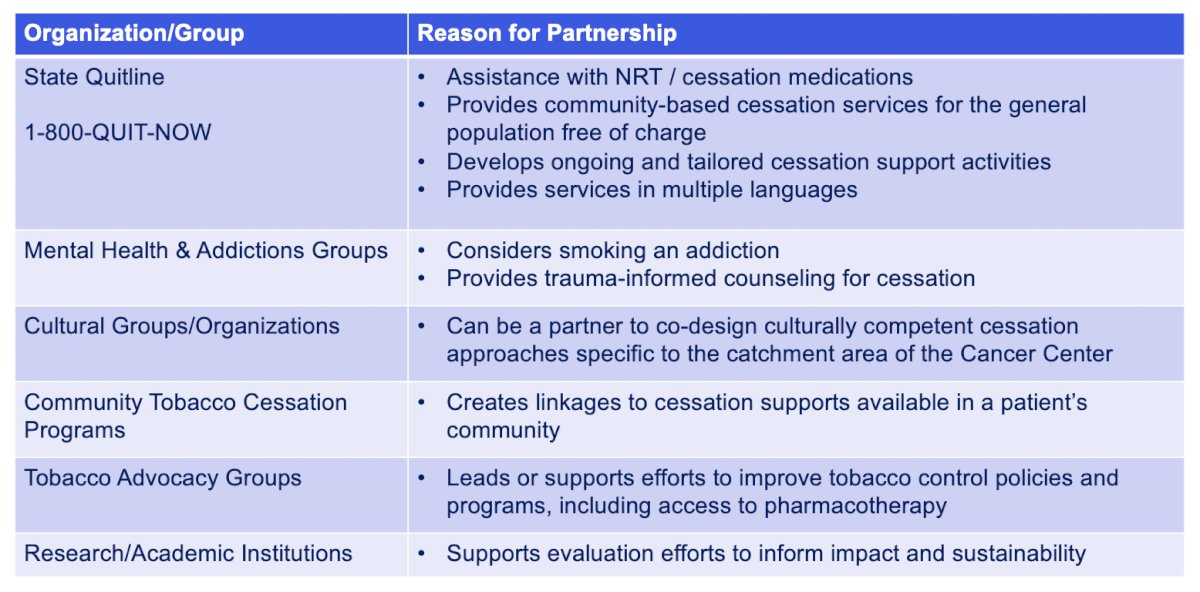
To make improvements, it is important to do a local assessment at each provider’s site. This should include:
- Understanding the current practices: EPIC slicer/dicer, TTP available?
- Assess context and resources, starting with system-level changes:
- Outpatient clinic visit workflow
- Post-op order sets
- Referral process to TTP (automatic versus MD initiated)
- Standard post visit summary inclusion
- Use validated instruments (C-TUQ) and structured data in the notes
- Long term, it is important to have a multilevel strategy developed with stakeholders
Similarly, given the known gap in knowledge among even urologists, another avenue to approach dissemination and awareness is through clinical treatment guidelines. Dr. Matulewicz and colleagues compared recommended practices among bladder and lung cancer guidelines, demonstrating substantial differences:8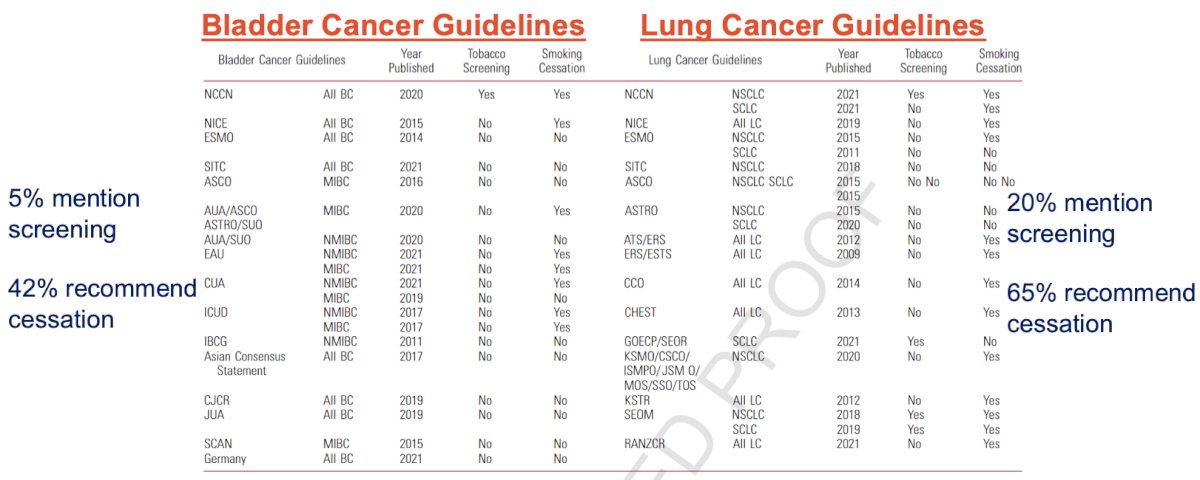
Dr. Matulewicz concluded his presentation discussing implementing smoking cessation in the urologic oncology setting with the following take home messages:
- Urologists manage smoking related disease often and their advice is impactful
- Helping a patient quit smoking is perhaps the most impactful intervention available in urologic oncology/urology
- Evidence-based practices are established and infrequently used
- Creative multi-level solutions specific to your setting can overcome barriers and bridge “quality chasm” – make it easy
- First, we need to recognize the importance as a specialty
- Quite simply, optimizing tobacco treatment is precision cancer care using an effective biobehavioral treatment
Presented by: Richard Matulewicz, MD, MSCI, MS, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
Related Content: Smoking Cessation as a Precision Cancer Care Intervention in Urologic Oncology - Richard Matulewicz
References:
- Bandak M, Nielsen KS, Kreiberg M, et al. Smoking as a prognostic factor for survival in patients with disseminated germ cell cancer. J Natil Cancer Inst. 2023 Jun 8;115(6):753-756.
- Cinciripini PM, Kypriotakis G, Blalock JA, et al. Survival Outcomes of an Early Intervention Smoking Cessation Treatment after a Cancer Diagnosis. JAMA Oncol. 2024 Oct 31 [Epub ahead of print].
- Bernstein AP, Bjurlin MA, Sherman SE, et al. Tobacco screening and treatment during outpatient urology office visits in the United States. J Urol. 2021 Jun;205(6):1755-1761.
- Myrie AK, Matulewicz RS. Perceptions of the link between smoking and bladder cancer among United States adults. J Urol. 2021 Feb;205(2):324-326.
- Matulewicz RS, Meeks W, Mbassa R, et al. Urologists’ Perceptions and Practices Related to Patient Smoking and Cessation: A National Assessment from the 2021 American Urological Association Census. Urology. 2023 Oct:180:14-20.
- Bassett JC, Matulewicz RS, Kwan L, et al. Prevalence and Correlates of Successful Smoking Cessation in Bladder Cancer Survivors. Urology. 2021 Jul:153:236-243.
- Cacciamani GE, Matulewicz RS, Kumar R, et al. Fighting the ‘tobacco epidemic’ – A call to action to identify Targeted Intervention Points (TIPs) for better counseling patients with urothelial cancer. Urol Oncol. 2021 Dec;39(12):793-796.
- Michael J, Matulewicz RS, Bjurlin MA. Assessment of tobacco screening and smoking cessation recommendations among bladder cancer guidelines: A call to action. J Urol. 2022 Mar;207(3):490-492.


