(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Bladder Cancer Session II. Dr. Hadley Wyre discussed how to prevent and manage Long Term Complications of Radical Cystectomy.
Radical cystectomy (RC) is a morbid operation with a high rate of perioperative complications. If patients survive their cancer, long-term complications significantly impact their quality of life. Dr. Wyre divided his presentation into two main complications:
- Ureteroenteric anastomotic strictures
- Hernias (parastomal hernias or ventral hernias
Dr. Wyre mentioned that we should aim to prevent ureteroenteric anastomotic strictures by following standard anastomotic principles, which include a watertight closure, a tension-free anastomosis, and not handling the ureter with pickups at all—the "no touch technique." This is crucial considering that the microvascular anatomy of the ureter can be easily disrupted and damaged.
The blood supply to the ureter in the pelvis comes laterally from the iliac vessels and their branches. During RC, we sever all blood supply to the distal ureter by ligating the superior and inferior vesical pedicles and their branches. Consequently, we must rely solely on blood flow from the gonadal and renal arteries.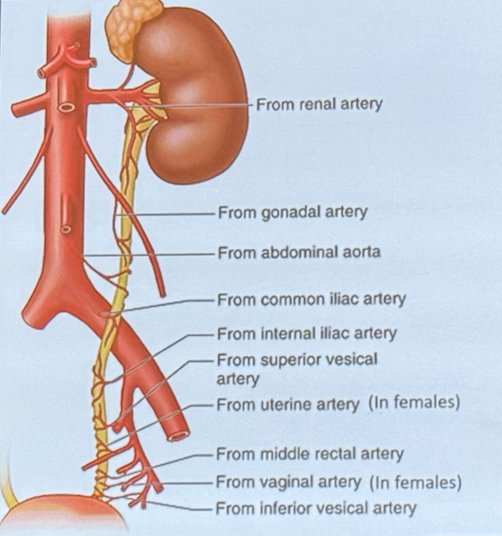
Moreover, a study exploring the length of the ureter resected and the stricture rate found that the longer the resected ureter, meaning the shorter the remaining ureter in the body, the higher the risk of anastomotic stricture.
Dr. Wyre mentioned that other tips for preventing ureteroenteric anastomotic strictures include making long conduits, which he considers easier for reconstruction and facilitates a tension-free anastomosis. While this is not data-driven, from a reconstructive urologist's perspective, it is preferable. Additionally, extensively spatulating the ureters and discarding the unused portion is advisable. Dr. Wyre likes to keep the stapler line to identify the end of the ileal conduit (IC), as shown in the photo (calcification spot). This helps him locate the ureteroenteric anastomosis and monitor the location of the conduit.
There are two options:
- Endoscopic treatments
- Redo anastomosis with similar principles
Dr. Wyre doesn’t offer his patients endoscopic treatments because he considers these to have poor outcomes. He believes that giving the ureter a period of rest (removing the stent and switching to a nephrostomy tube) before reconstructive surgery improves tissue quality and facilitates the reconstruction process. He briefly discussed a retrospective study showing that ureteral rest was associated with a higher success rate compared to those not undergoing ureteral rest (90.7% vs. 77.5%), and they were less likely to require a buccal mucosal graft.1
Parastomal HerniasDr. Wyre described the main problem with parastomal hernias: no one wants to take care of them. It is a grey area because general surgeons often do not understand the ileal conduit (IC) anatomy and the location of the ureters, and urologists are not typically trained to repair these hernias.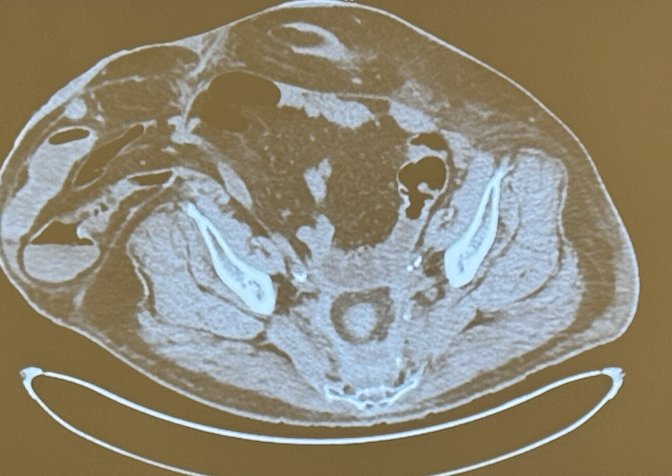
Dr. Wyre gave advice on how to prevent parastomal hernias. He emphasized that when planning for the stoma, it is crucial to position it higher. The higher the stoma, the better the outcome. Conversely, the lower the hernia, the more pressure will be transmitted to the hernia site, especially in patients with a high body mass index. He also raised the question of whether there is any role for prophylactic mesh placement.
The International Classification of Abdominal Wall Planes (ICAP) describes various planes and spaces for placing mesh in the treatment of ventral hernias. These planes are critical for both prophylactic mesh placement and for treating parastomal hernias and are illustrated in the figure below.2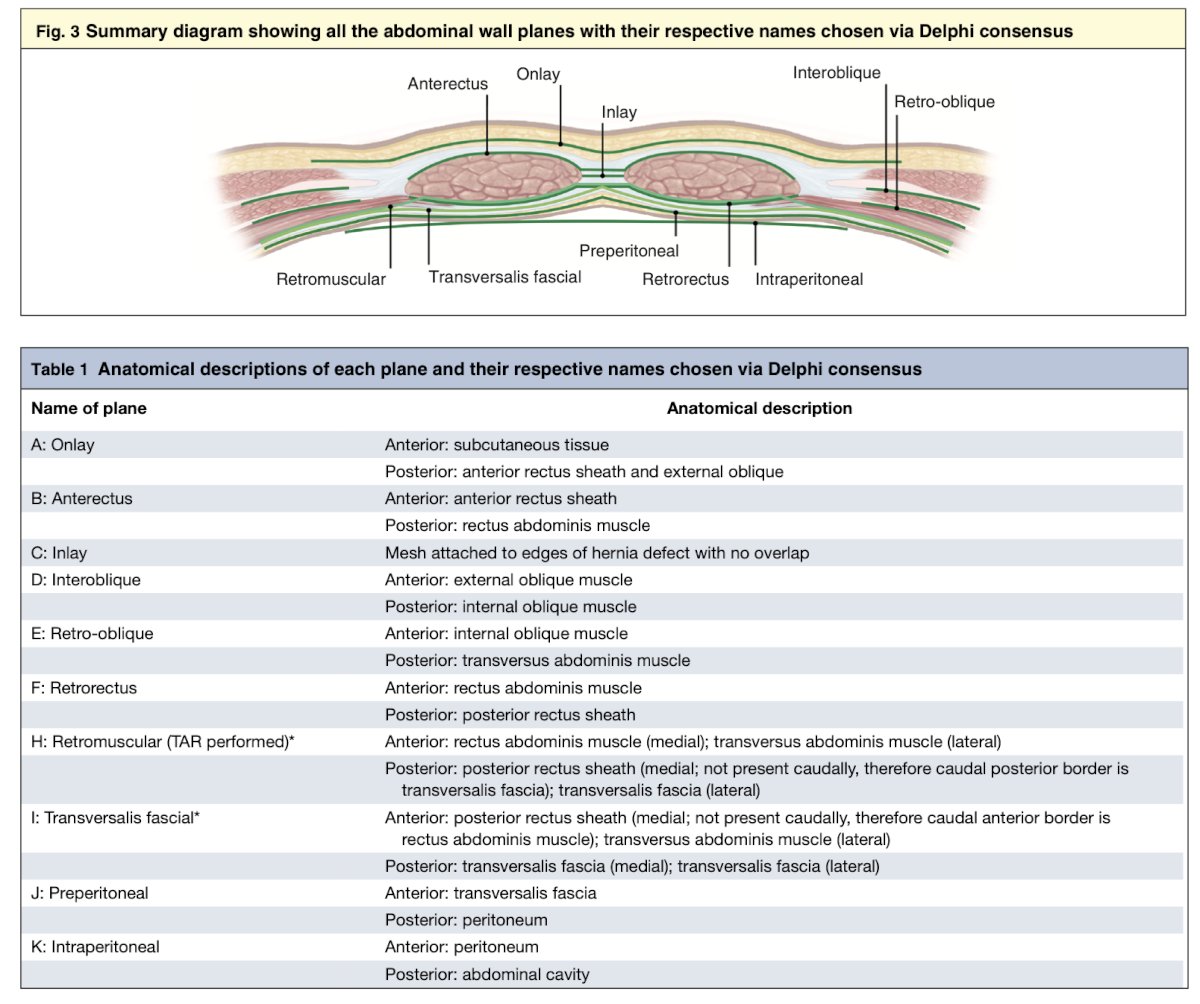
A phase 3, randomized, controlled trial at the University of Southern California (USC) included 146 patients who underwent RC and IC. They randomized patients to receive prophylactic biological mesh at the time the ileal conduit was created, with the mesh placed intraperitoneally. The study reported no higher complications in the prophylactic mesh group, but also found no change in hernia rates within 2 years following surgery.3
On the other hand, a Swedish randomized study included 242 patients who were randomized 1:1 to either conventional stoma construction (n = 124) or prophylactic mesh (n = 118). They used a Vypro mesh (10x10 cm), which is a synthetic mesh, placed in the retrorectus space (Illustrated below). This study reported a 55% reduction in parastomal hernia risk in the prophylactic mesh group.4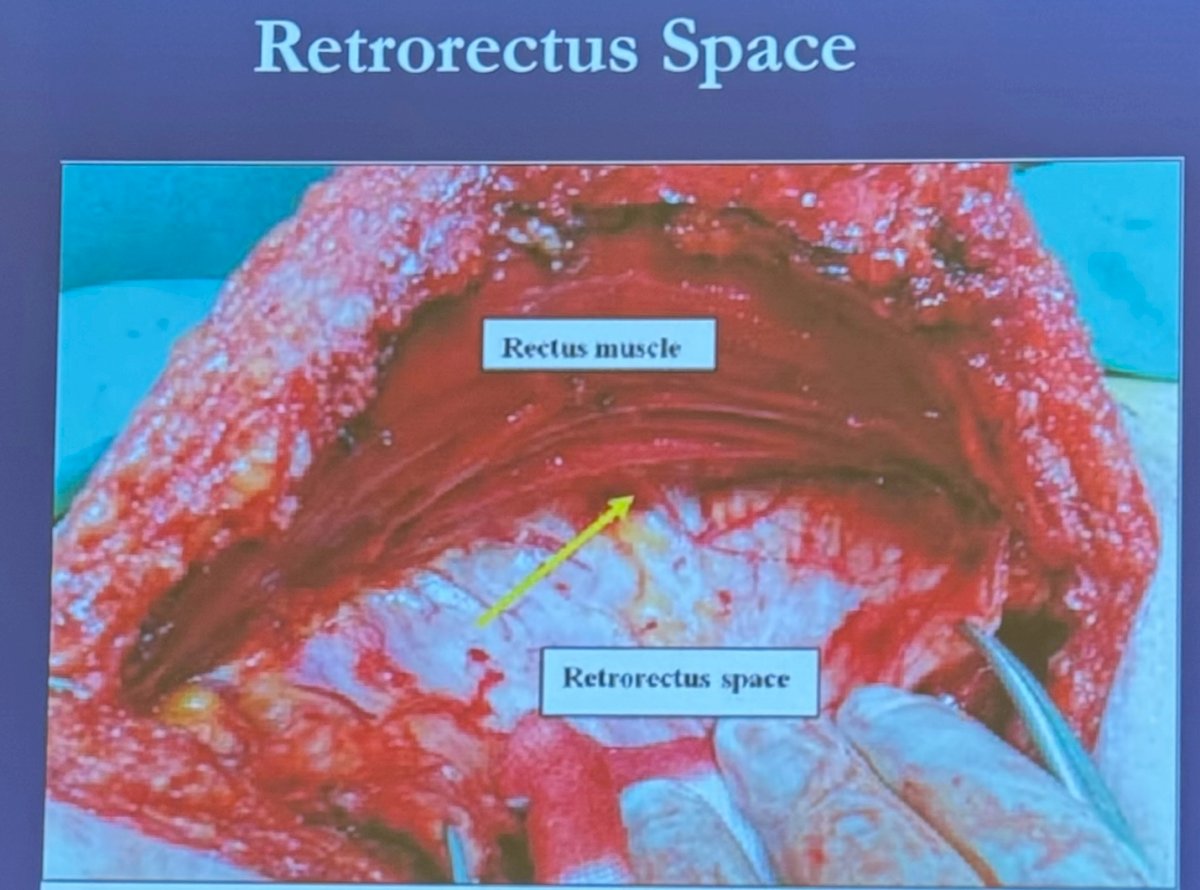
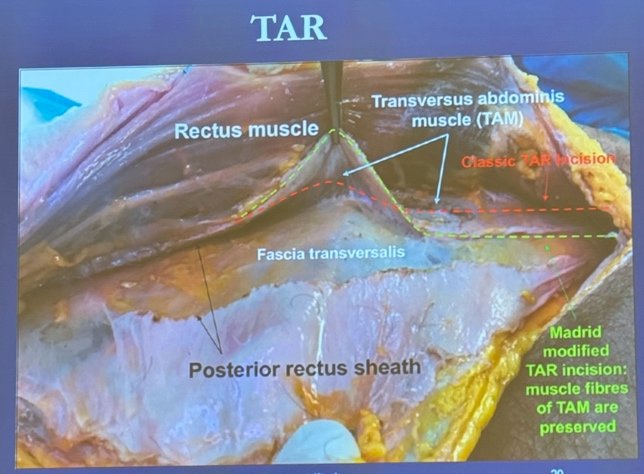
Dr. Wyre briefly discussed the transversus abdominis release (TAR) technique, which is primarily indicated for the repair of large and complex ventral hernias, including incisional hernias. This technique involves accessing the plane of the transversalis fascia and developing the space posterior to the transversus abdominis muscle, allowing for very wide mesh placement, as illustrated below.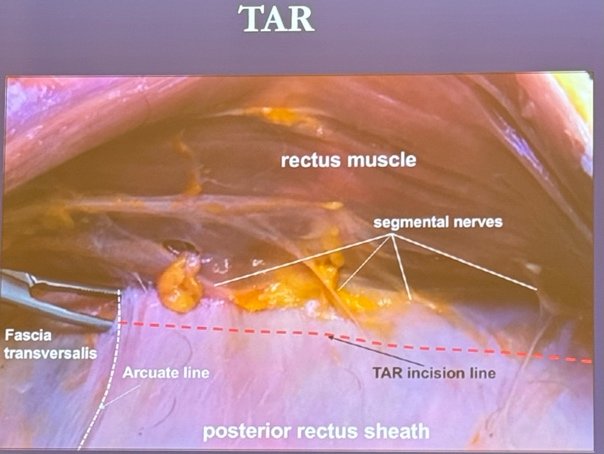
Most hernias don’t need to be treated. However there are some absolute and relative indications for treatment:
Absolute
- Obstruction of GI tract
- Obstruction of Urinary tract
Relative
- Pain
- Pouching problems
- Skin breakdown
- Cosmetic
There are essentially two techniques for treating parastomal hernias (shown below): the keyhole technique for parastomal mesh placement and the Sugarbaker technique for parastomal mesh placement. However, the Sugarbaker technique was originally described for colostomies, and it can be challenging to lateralize the ileal conduit in this approach.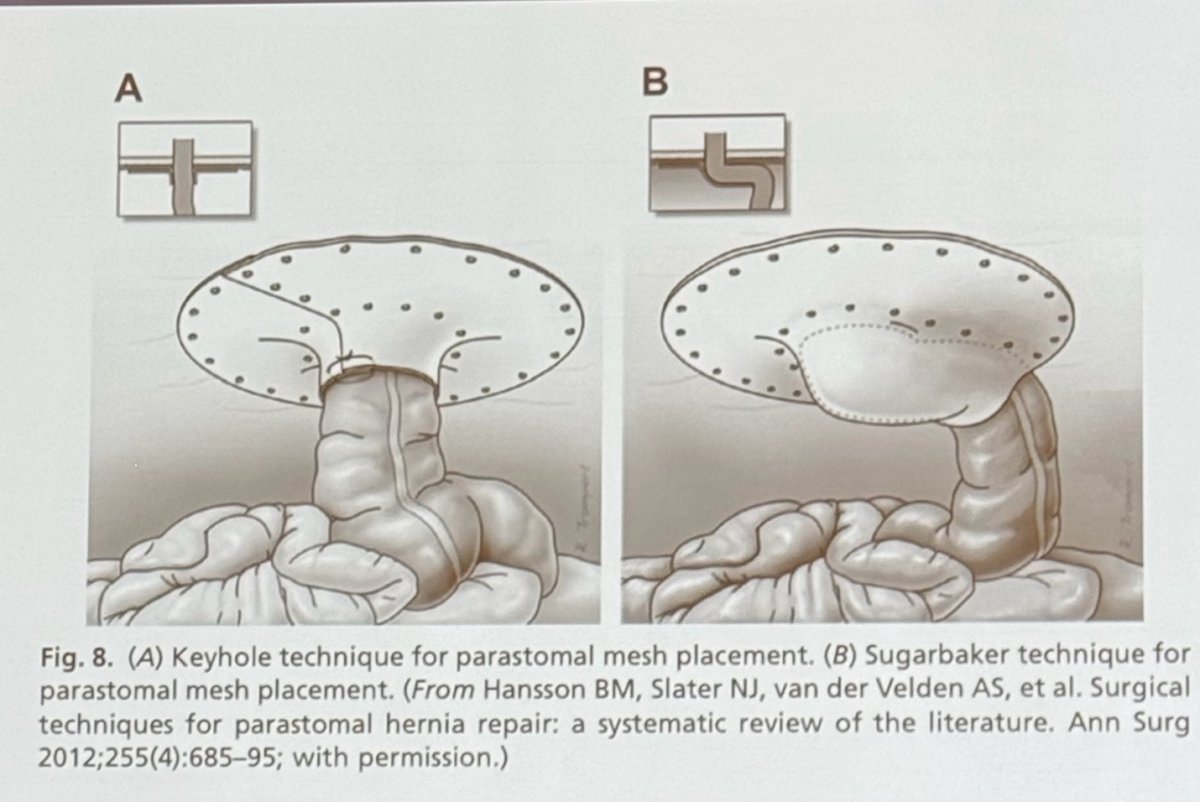
Below there is a CT scan of a patient with a parastomal hernia repair with the modified sugar baker technique: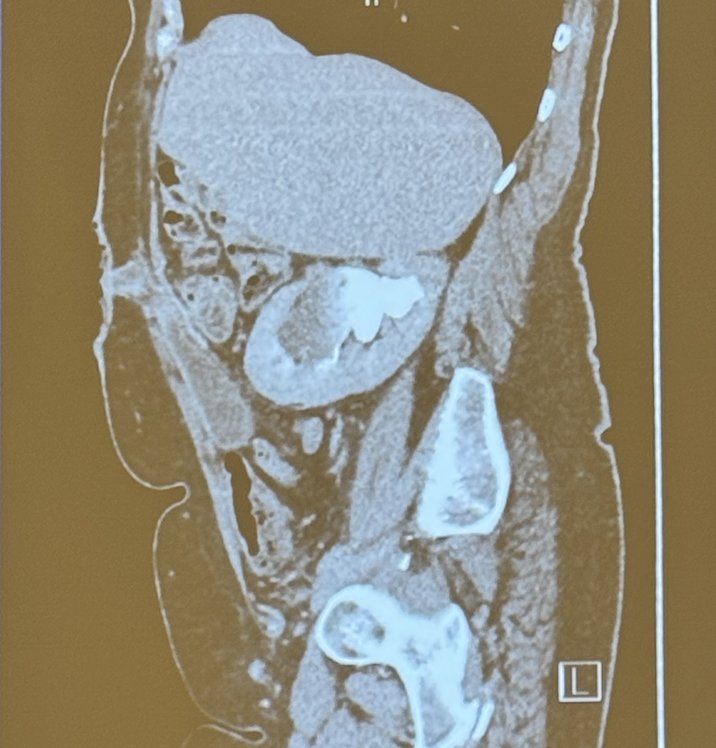
Another parastomal hernia repair technique is the Pauli technique, which involves dissection of the retromuscular space, transversus abdominis release, and lateralization of the stoma with the placement of a retromuscular mesh. Dr. Wyre reserves this technique only for large ventral hernia repairs.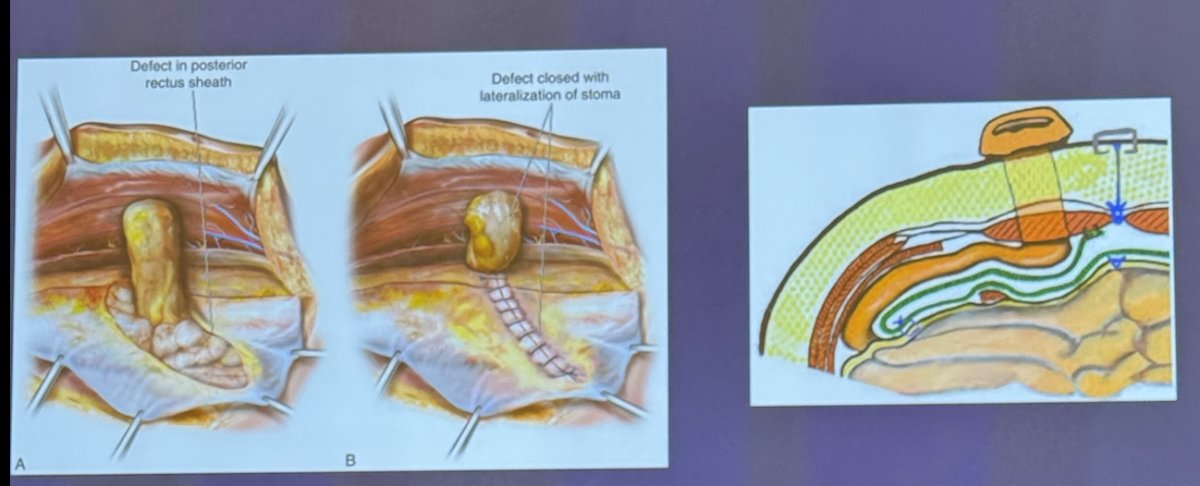
Dr. Wyre concluded his presentation by showing an algorithm for parastomal hernia repair that works for him and is illustrated below: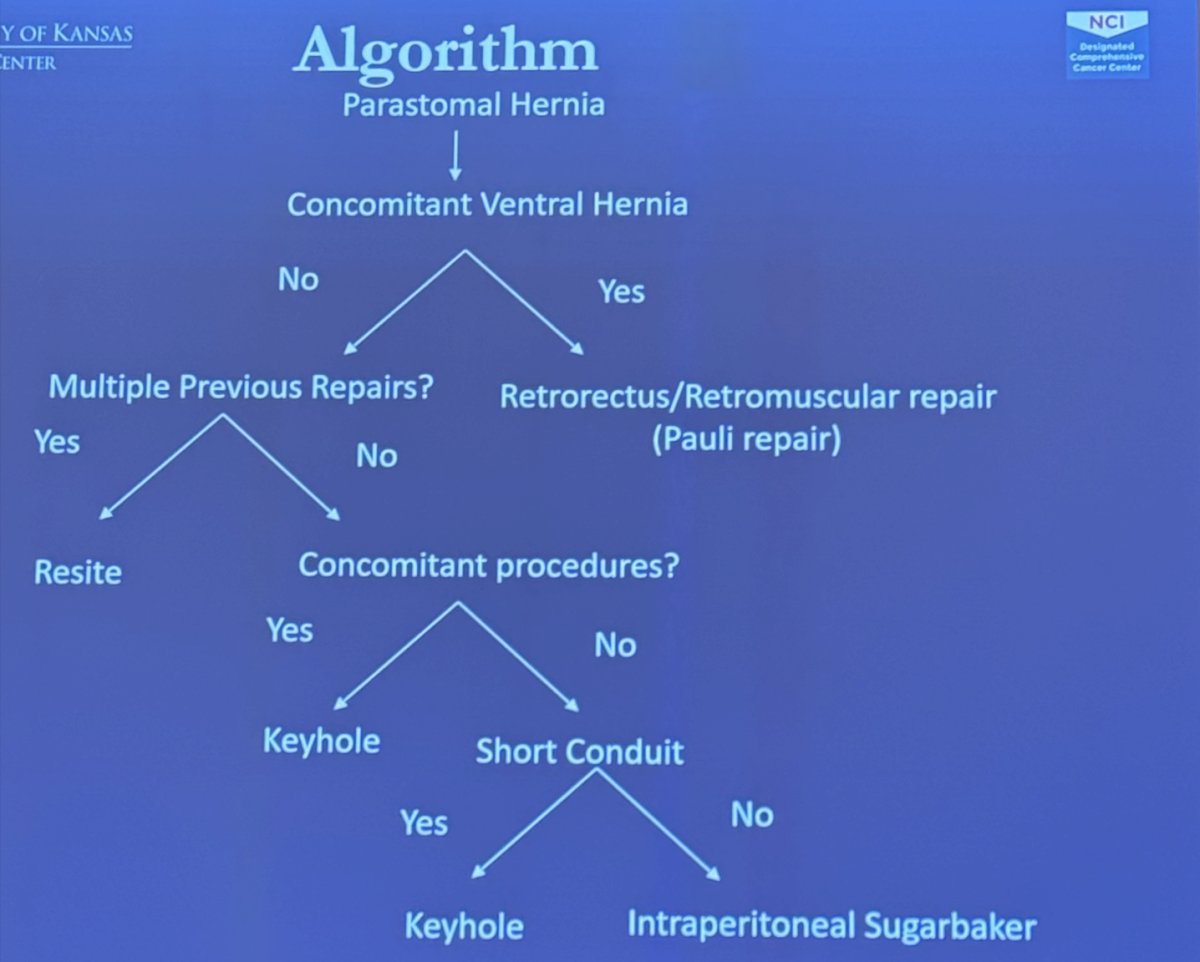
Presented by: Hadley Wyre, MD, Associated Professor of Urologic Surgery at the University of Kansas Medical School, Kansas City, KS.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:- Lee Z, Lee M, Lee R, Koster H, Cheng N, Siev M, Jun M, Munver R, Ahmed M, Zhao LC, Stifelman MD, Eun DD; Collaborative of Reconstructive Robotic Ureteral Surgery (CORRUS). Ureteral Rest is Associated With Improved Outcomes in Patients Undergoing Robotic Ureteral Reconstruction of Proximal and Middle Ureteral Strictures. Urology. 2021 Jun;152:160-166. doi: 10.1016/j.urology.2021.01.058. Epub 2021 Feb 25. PMID: 33639184.
- Parker SG, Halligan S, Liang MK, Muysoms FE, Adrales GL, Boutall A, de Beaux AC, Dietz UA, Divino CM, Hawn MT, Heniford TB, Hong JP, Ibrahim N, Itani KMF, Jorgensen LN, Montgomery A, Morales-Conde S, Renard Y, Sanders DL, Smart NJ, Torkington JJ, Windsor ACJ. International classification of abdominal wall planes (ICAP) to describe mesh insertion for ventral hernia repair. Br J Surg. 2020 Feb;107(3):209-217. doi: 10.1002/bjs.11400. Epub 2019 Dec 25. PMID: 31875954.
- Djaladat H, Ghoreifi A, Tejura T, Miranda G, Cai J, Sheybaee Moghaddam F, Aldana I, Sotelo R, Gill I, Bhanvadia S, Schuckman A, Desai M, Aron M, Daneshmand S, Duddalwar V. Prophylactic Use of Biologic Mesh in Ileal Conduit (PUBMIC): A Randomized Clinical Trial. J Urol. 2024 Jun;211(6):743-753. doi: 10.1097/JU.0000000000003902. Epub 2024 Apr 15. PMID: 38620056.
- Liedberg F, Kollberg P, Allerbo M, Baseckas G, Brändstedt J, Gudjonsson S, Hagberg O, Håkansson U, Jerlström T, Löfgren A, Patschan O, Sörenby A, Bläckberg M. Preventing Parastomal Hernia After Ileal Conduit by the Use of a Prophylactic Mesh: A Randomised Study. Eur Urol. 2020 Nov;78(5):757-763. doi: 10.1016/j.eururo.2020.07.033. Epub 2020 Aug 13. PMID: 32800407.


