(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Confederacion Americana de Urologia (CAU) Presentation. Dr. Francisco Rodriguez-Covarrubias discussed the evolving role of surgery in the treatment of advanced kidney cancer in Latin America.
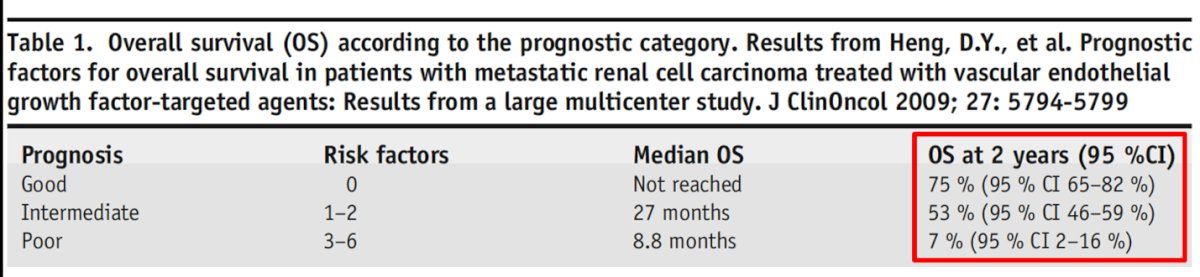
Dr. Rodriguez-Covarrubias began his presentation by emphasizing that, despite significant clinical advancements in the treatment of renal cell carcinoma (RCC), prognosis remains poor in advanced stages. He highlighted that 75% of patients in the IMDC (International Metastatic Renal Cell Carcinoma Database Consortium) good prognostic group are alive at two years, compared to only 53% in the intermediate prognostic group and just 7% in the poor prognostic group. Historically, patients in the poor prognostic group had a median overall survival (OS) of 8.8 months.
In Latin America, several barriers affect the treatment of advanced renal cell carcinoma (RCC). These barriers stem from variations in healthcare systems across different countries, which can limit access to different therapies. Notably, there are disparities in access to pharmacological options, which often leads to a higher risk of treatment-related toxicities. Additionally, the financial burden associated with treatment is compounded by unfavorable currency conversion, further limiting patient access to care. Consequently, these challenges contribute to lower cure rates and increased surgical morbidity in the region.
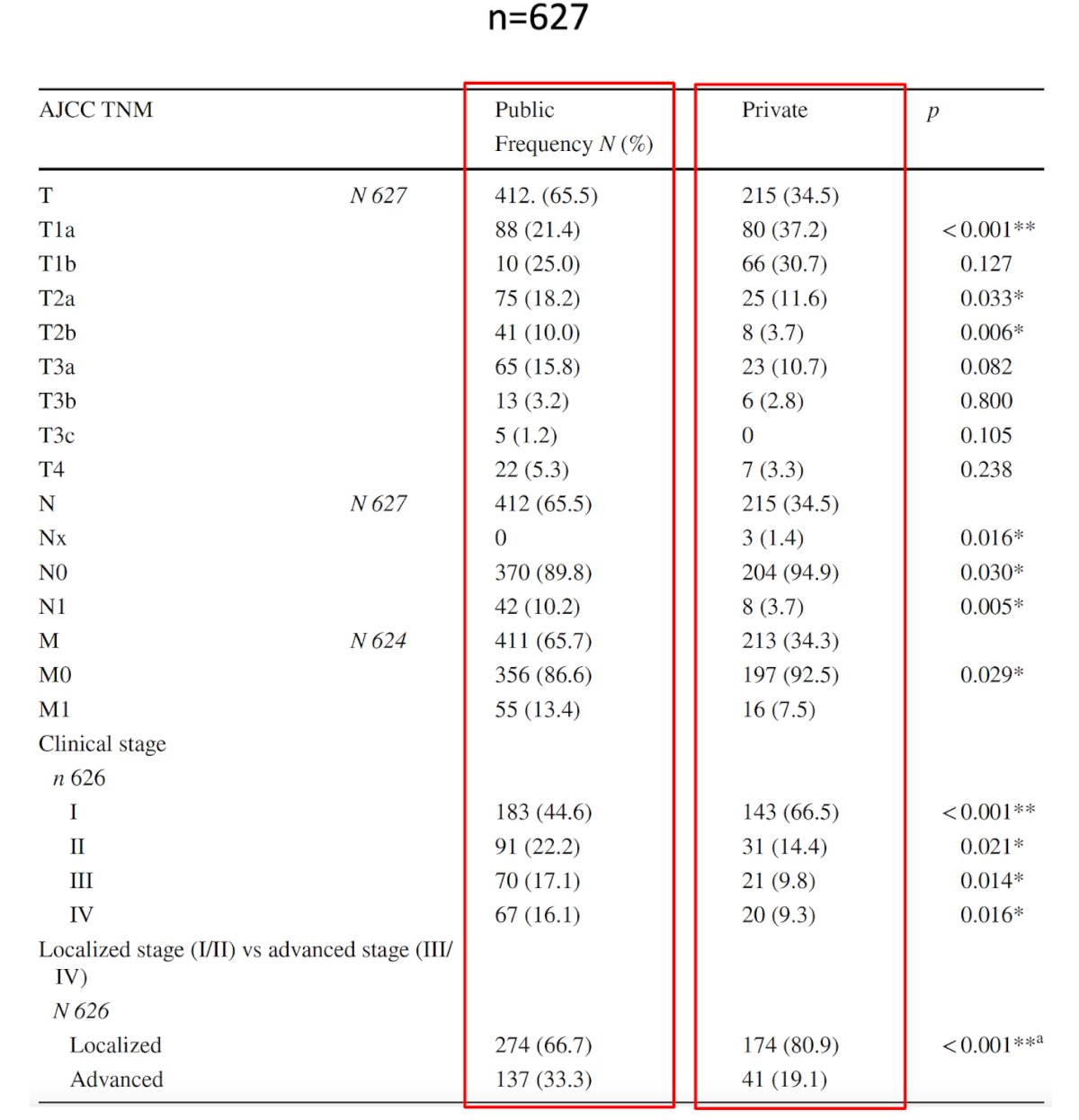
Dr. Rodriguez-Covarrubias briefly discussed a cross-sectional study conducted in Monterrey, Mexico. The study analyzed 627 patients with RCC treated surgically between 2011 and 2021. It compared patients from private and public healthcare settings. Results showed that patients in the public sector had larger tumors, a higher prevalence of advanced disease, and more risk factors, while the private sector had a higher proportion of patients treated with minimally invasive surgeries and a significantly lower number of patients with metastatic disease at the time of diagnosis (13.4% in the public sector vs. 7.5% in the private sector). Public sector patients also presented with more symptoms and lymphovascular invasion. The results of the study are summarized in the table below. The study highlights the critical need for improved health policies aimed at enhancing early detection of RCC in Mexico and improving access to treatment for patients in the public healthcare sector.2
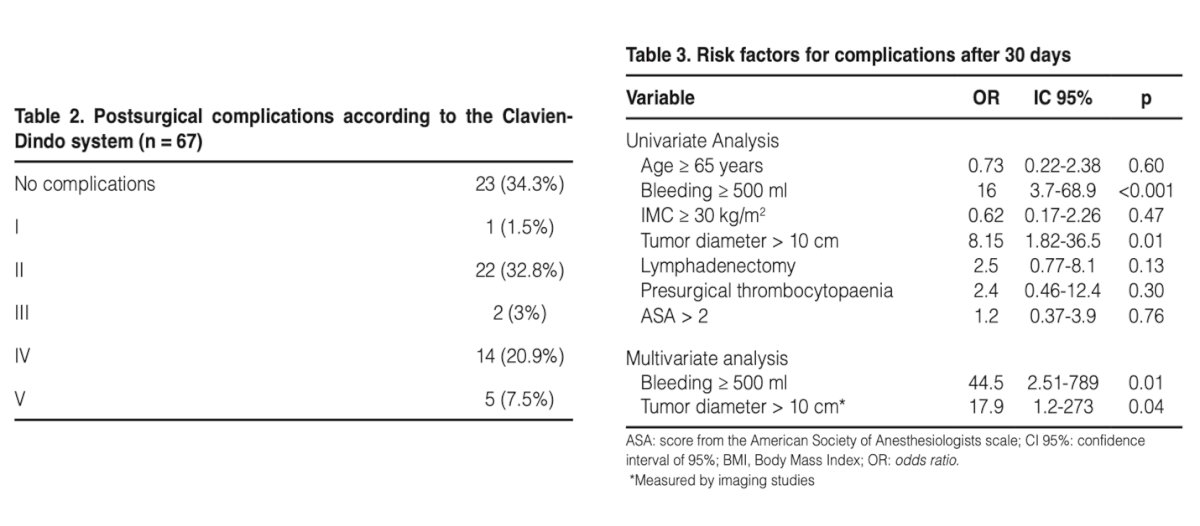
Moreover, Dr. Rodriguez-Covarrubias discussed risk factors for developing surgical complications in patients with advanced RCC who had been treated with cytoreductive nephrectomy. He presented a retrospective, study led by himself, in which the investigators analyzed 67 patients who underwent cytoreductive nephrectomy for metastatic renal cell carcinoma (mRCC), The study found that 89.7% of patients had symptoms, with weight loss being the most common (50.8%). The mean tumor diameter was 10.8 cm, and the postoperative complication rate was 65%, with 31.4% experiencing major complications (grades 3 or higher). Multivariate logistic regression analyses identified two risk factors for complications: estimated blood loss over 500 mL (odds ratio [OR] 44.5) and tumor diameter greater than 10 cm (OR 17.9).3
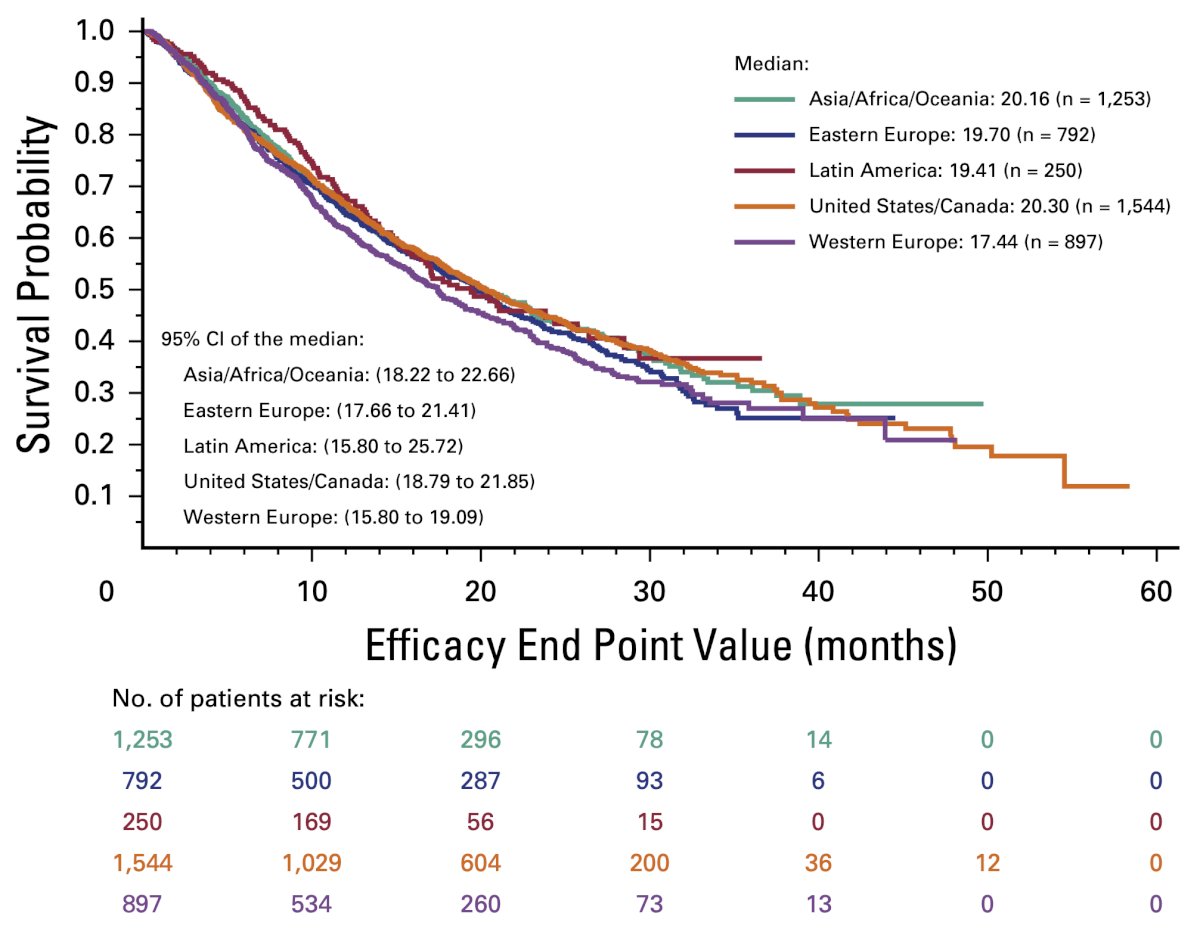
A pooled analysis of 4,736 patients with metastatic renal cell carcinoma treated in phase II or III clinical trials aimed to determine if geographic regions impacted survival outcomes was discussed by Dr. Rodriguez-Covarrubias. The investigators found no significant differences in overall survival (OS) between patients in the United States/Canada (USC) and those in Latin America, Asia/Oceania/Africa, and Eastern Europe. However, univariable analysis indicated a difference in OS between USC and Western Europe (20.3 vs. 17.4 months; p=0.015), which was not significant in multivariable analysis. The Kaplan-Meier graphic of OS is shown below.4
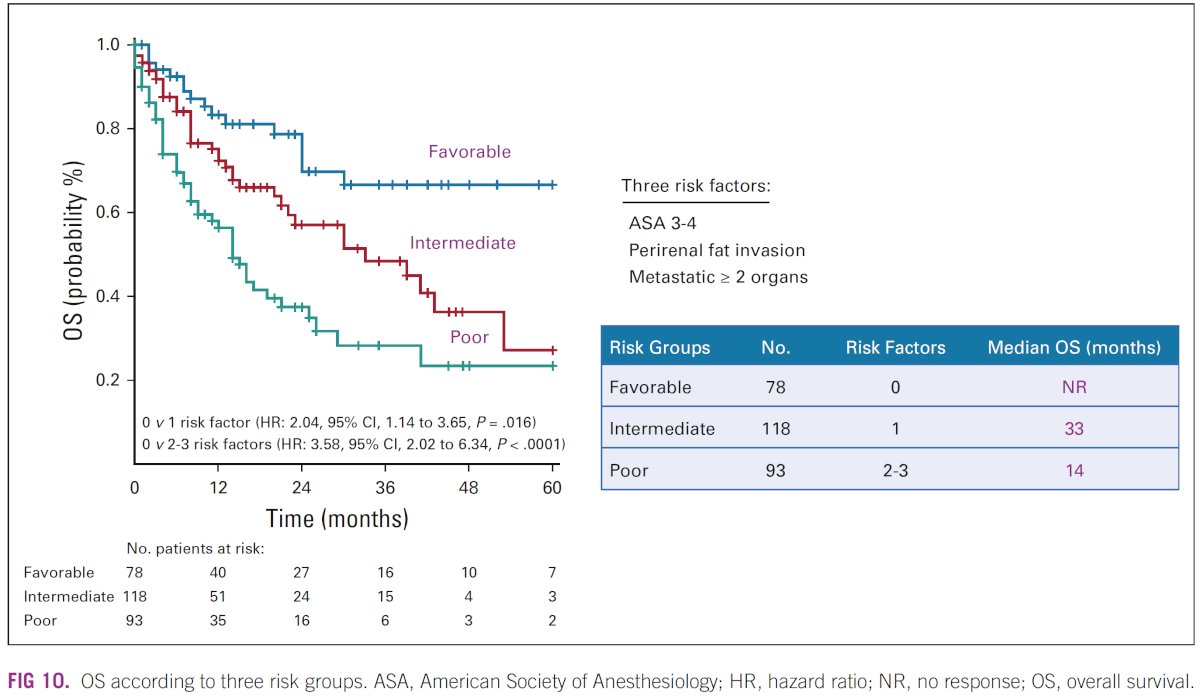
Dr. Rodriguez-Covarrubias presented a study by the Latin American Renal Cancer Group (LARCG) that evaluated prognostic factors in patients with synchronous metastatic renal cell carcinoma (mRCC). This study included 530 patients and identified several independent prognostic factors for 5-year overall survival (OS) in multivariable analyses. These factors were the American Society of Anesthesiology (ASA) classification 3-4 vs. 1-2 (HR: 1.64), perirenal fat invasion (HR: 2.02), and having two or more metastatic organ sites (HR: 2.19). The investigators used these variables to create a risk group stratification: no adverse risk factors (favorable group), with a median OS not reached; one adverse factor (intermediate group), with a median OS of 33 months (HR: 2.04); and two or three adverse factors (poor risk group), with a median OS of 14 months.5 The findings are illustrated in the figure below.
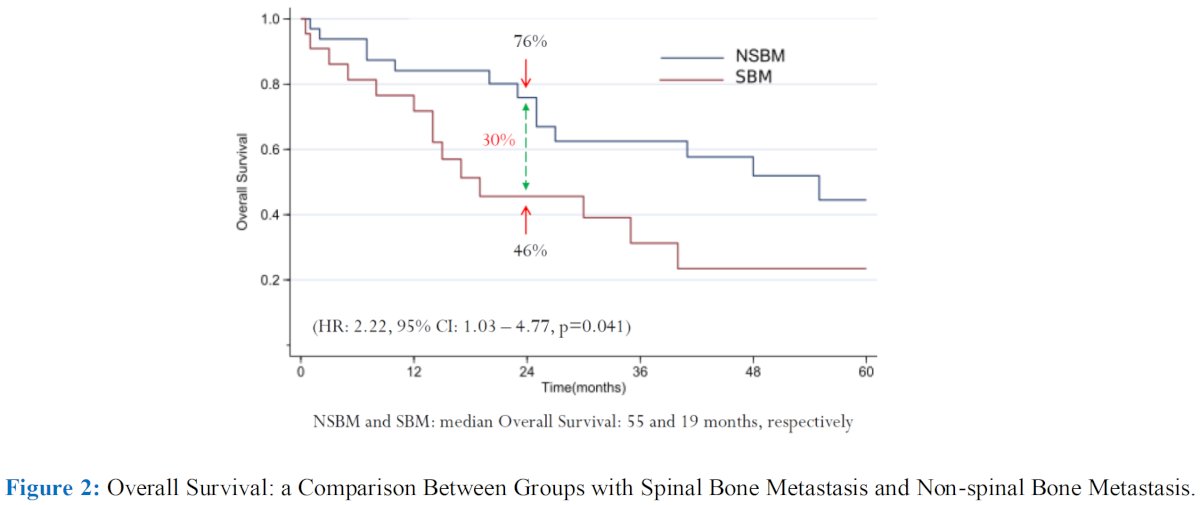
Dr. Rodriguez-Covarrubias also highlighted the impact of bone metastasis location on overall survival in mRCC patients. In a retrospective analysis of 4,060 mRCC patients from the LARCG database, it was found that the presence of spinal bone metastases significantly worsened overall survival compared to non-spinal bone metastases (HR 2.22, 95% CI 1.03-4.77, p=0.041).
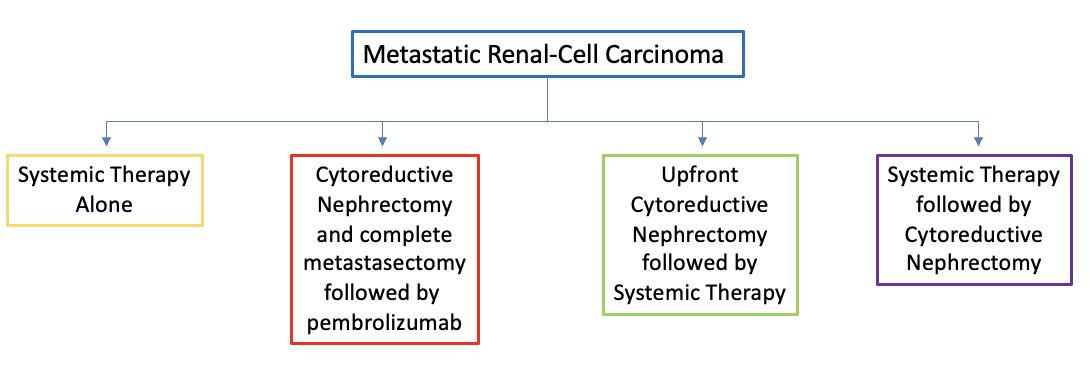
The treatment landscape of mRCC has evolved significantly in recent years. Currently, there are four primary treatment options for patients with mRCC: systemic therapy alone, cytoreductive nephrectomy and complete metastasectomy (resulting in no evidence of disease, or NED) followed by Pembrolizumab, upfront cytoreductive nephrectomy followed by systemic therapy, or systemic therapy followed by cytoreductive nephrectomy Dr. Rodriguez-Covarrubias provided this algorithm for management of mRCC:
However, how is the treatment landscape in Latin America? The Latin American Renal Cancer Group (LARCG) and the Latin American Cooperative Oncology Group (LACOG) have released expert panel recommendations for the treatment of mRCC. They advise that the decision between systemic therapy and surgery should be made by a multidisciplinary team. They recommend upfront cytoreductive nephrectomy when clinically feasible for low-risk and selected intermediate-risk patients who have good performance status, a low metastatic burden, are candidates for metastasectomy or surveillance after surgery, and do not require immediate systemic therapy.6
Dr. Rodriguez-Covarrubias highlighted that he, along with the CAU has worked together with NCCN and served as international reviewers for the NCCN guidelines framework for kidney cancer. The 2023 NCCN guidelines now distinguish between clinical care settings with basic resources, core resources, and enhanced resources. Based on these classifications, they recommend different treatment options for patients with both clear cell and non-clear cell histology.
To conclude his presentation, Dr. Rodriguez-Covarrubias emphasized several key points:
- Cytoreductive nephrectomy still plays a crucial role in the management of mRCC.
- In Latin America, due to limited access to novel pharmacological agents, cytoreductive nephrectomy remains a cornerstone of initial therapy.
- Refined patient selection is essential to achieve better outcomes, especially considering the significant surgical adverse events associated with the procedure.
- Collaboration between Latin American urological organizations and their North American and European counterparts has increased rapidly, providing high-quality information to improve decision-making and patient counseling.
Presented by: Francisco Rodriguez-Covarrubias, MD, Urologist at Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ) and at Médica Sur Hospital in Mexico City.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:- Puente Vázquez J, Alonso Gordoa T, Moreno J, Poma L, Diaz Rubio E, Gomez A, Blazquez J, Gonzalez Larriba JL. New challenges in kidney cancer management: integration of surgery and novel therapies. Curr Treat Options Oncol. 2015 Mar;16(3):337. doi: 10.1007/s11864-015-0337-5. PMID: 25782687.
- Barrera-Juarez E, Halun-Trevino AN, Ruelas-Martinez M, Madero-Frech A, Camacho-Trejo V, Estrada-Bujanos M, Bojorquez D, Uribe-Montoya J, Rodriguez-Covarrubias F, Villarreal-Garza C. Prognosis impact and clinical findings in renal cancer patients: comparative analysis between public and private health coverage in a cross-sectional and multicenter context. Cancer Causes Control. 2024 Nov 8. doi: 10.1007/s10552-024-01891-3. Epub ahead of print. PMID: 39514146.
- Hernández-Pañeda H, Garza-Gangemi AM, Manzanilla-Romero HH, Hernández-Gaytán CA, Gabilondo-Navarro F, Rodríguez-Covarrubias F. Risk factors for the development of postoperative complications in patients with metastatic kidney cancer treated with cytoreductive nephrectomy. Cir Cir. 2021;89(5):632-637. English. doi: 10.24875/CIRU.20000871. PMID: 34665165.
- Fay AP, McKay RR, Lin X, Simantov R, Choueiri TK. Impact of Geographic Regions on Overall Survival in Patients With Metastatic Renal Cell Carcinoma: Results From an International Clinical Trials Database. J Glob Oncol. 2018 Sep;4:1-14. doi: 10.1200/JGO.17.00119. PMID: 30241151; PMCID: PMC6223429.
- Abreu D, Carvalhal G, Gueglio G, Tobia I, Garcia P, Zuñiga A, Meza L, Bengió R, Scorticati C, Castillejos R, Rodriguez F, Autran AM, Gonzales C, Gadu J, Nolazco A, Ameri C, Zampolli H, Langenhin R, Muguruza D, Machado MT, Mingote P, Yandian J, Clavijo J, Nogueira L, Clark O, Secin F, Rovegno A, Vilas A, Barrios E, Decia R, Guimarães G, Glina S, Pal SK, Rodriguez O, Palou J, Spiess P, Lara PN Jr, Linehan WM, Pastore AL, Zequi SC. Prognostic Factors in De Novo Metastatic Renal Cell Carcinoma: A Report From the Latin American Renal Cancer Group. JCO Glob Oncol. 2021 May;7:671-685. doi: 10.1200/GO.20.00621. PMID: 33974442; PMCID: PMC8162501.
- Soares A, Monteiro FSM, da Trindade KM, Silva AGE, Cardoso APG, Sasse AD, Fay AP, Carneiro APCD, Alencar Junior AM, de Andrade Mota AC, Santucci B, da Motta Girardi D, Herchenhorn D, Araújo DV, Jardim DL, Bastos DA, Rosa DR, Schutz FA, Kater FR, da Silva Marinho F, Maluf FC, de Oliveira FNG, Vidigal F, Morbeck IAP, Rinck Júnior JA, Costa LAGA, Maia MCDF, Zereu M, Freitas MRP, Dias MSF, Tariki MS, Muniz P, Beato PMM, Lages PSM, Velho PI, de Carvalho RS, Mariano RC, de Araújo Cavallero SR, Oliveira TM, Souza VC, Smaletz O, de Cássio Zequi S. Advanced renal cell carcinoma management: the Latin American Cooperative Oncology Group (LACOG) and the Latin American Renal Cancer Group (LARCG) consensus update. J Cancer Res Clin Oncol. 2024 Apr 9;150(4):183. doi: 10.1007/s00432-024-05663-z. PMID: 38594593; PMCID: PMC11003910.


