(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Abstract/Posters Session. Dr. Clara Hwang presented the characteristics, treatment patterns, and outcomes of African American versus Caucasian patients with metastatic castration-resistant prostate cancer from a post hoc analysis of the TRUMPET registry.
Dr. Hwang emphasized that compelling evidence shows racial disparities in prostate cancer treatment in the US significantly impact a man's risk of death. African American patients receive less adequate care than their Caucasian counterparts, leading to notable differences in survival rates. Studies have also pointed out the low participation of Black patients in prostate cancer clinical trials, which hinders comprehensive analysis of outcomes by race.
There is a lack of robust data on racial disparities among patients with metastatic castration-resistant prostate cancer (mCRPC) in the US. The prospective, observational, multicenter (147 sites in the US) TRUMPET study, which enrolled patients with mCRPC from March 2015 to September 2019, aimed to assess treatment patterns and outcomes in this population. Dr. Hwang and colleagues present a post hoc analysis from this study, investigating racial disparities specifically among patients with mCRPC.
The inclusion criteria for the TRUMPET study were:
- Males (≥18 years old) with a confirmed diagnosis of M0 (nonmetastatic) or M1 (metastatic) castration resistant prostate cancer (CRPC) who presented for a routine visit and initiated treatment for CRPC
- Enrollment within 90 days from the time of decision to treat or first-line treatment initiation
- Second-line treatment enrollment was allowed if previous first-line CRPC treatments were restricted to first-generation antiandrogens (bicalutamide, flutamide, or nilutamide) or sipuleucel-T
- Patients with mCRPC who self-identified as African American or Caucasian
Patients were excluded from this post-hoc analysis if they identified as other races (Asian, American Indian or Alaskan Native, Native Hawaiian, or Pacific Islander) or had non-metastatic CRPC at baseline.
A total of 794 patients were included in this analysis, of these 133 were African American and 661 of Caucasian race. Baseline characteristics are shown in the table below: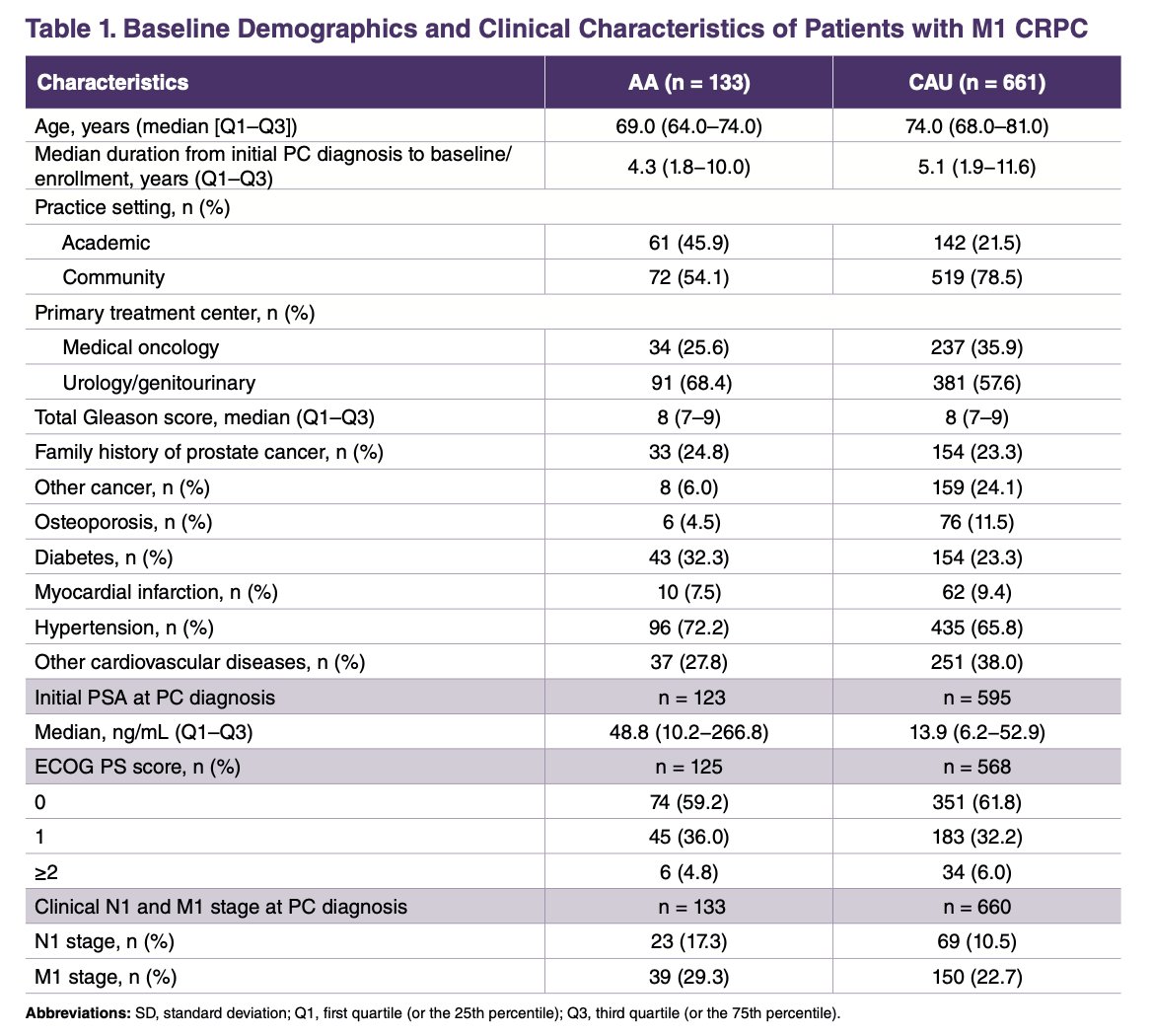
Notably, differences were observed in the primary treatments administered prior to mCRPC diagnosis. Active surveillance was offered to 12.0% of African American patients compared to 19.2% of Caucasian patients. Radical prostatectomy was performed in 18.0% of African Americans versus 36.3% of Caucasians, while adjuvant or salvage radiation therapy was given to 15.0% of African Americans and 17.7% of Caucasians. These disparities highlight the treatment differences between racial groups even before the progression to mCRPC.
As the initial treatment for mCRPC, a higher percentage of African American patients received androgen receptor pathway inhibitors (ARPIs) (62% vs. 57%) and chemotherapy (12% vs. 6%) compared to Caucasian patients. Interestingly, a greater proportion of Caucasian patients were treated with radionuclides and immunotherapy, as illustrated in the graphic below: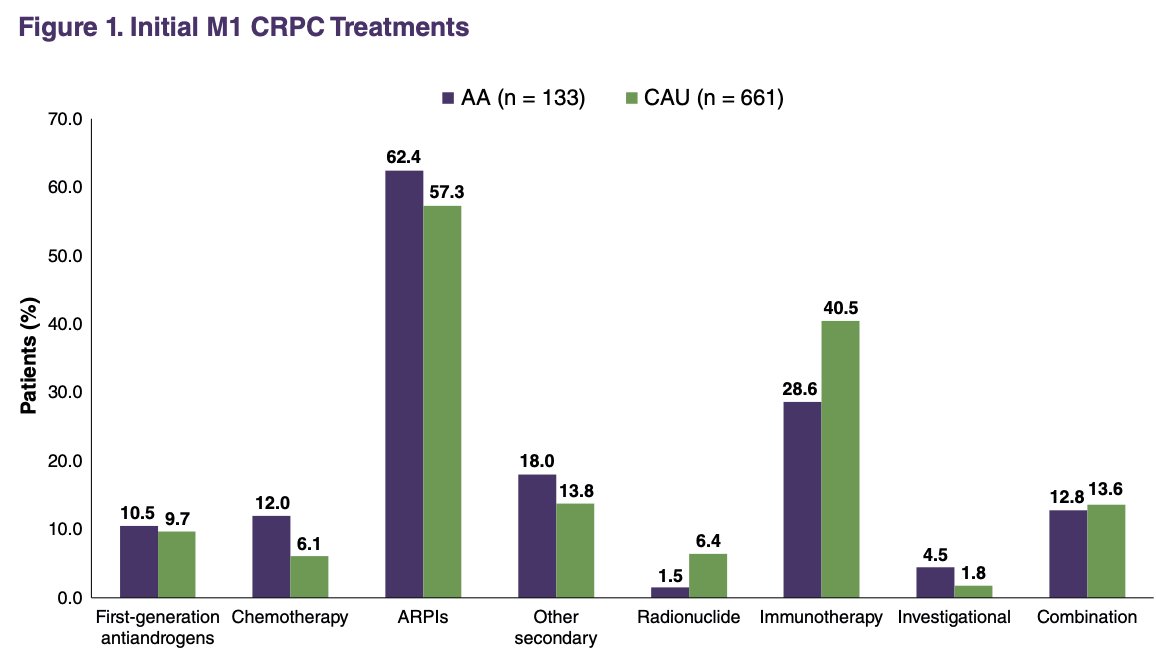
In terms of treatment pattern changes for mCRPC, the use of add-on therapy was 11.3% in African American patients compared to 14.4% in Caucasian patients. The rate of switching to a new treatment was also similar between the groups, with 52.6% of African Americans and 55.4% of Caucasians making the switch.
A trend toward better clinical outcomes was observed in African American patients compared to Caucasian patients, particularly in terms of clinical progression and time to skeletal-related events. However, these differences did not reach statistical significance, as shown in the forest plot below.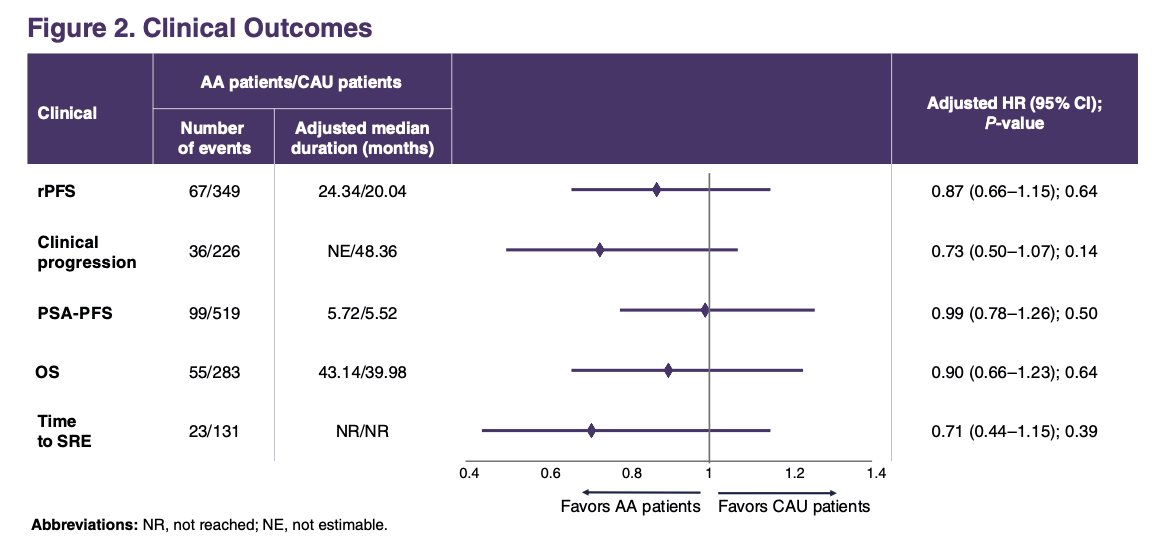
In the exploratory analysis of patients who received ARPIs as the initial treatment, African American patients demonstrated a trend toward improved overall survival (OS) compared to Caucasian patients. However, this difference was not statistically significant (HR 0.71, 95% CI 0.45–1.14; p=0.707). Additionally, no survival differences were observed between the two groups when both started mCRPC treatment with non-ARPIs, as indicated by the superimposed Kaplan-Meier curves below.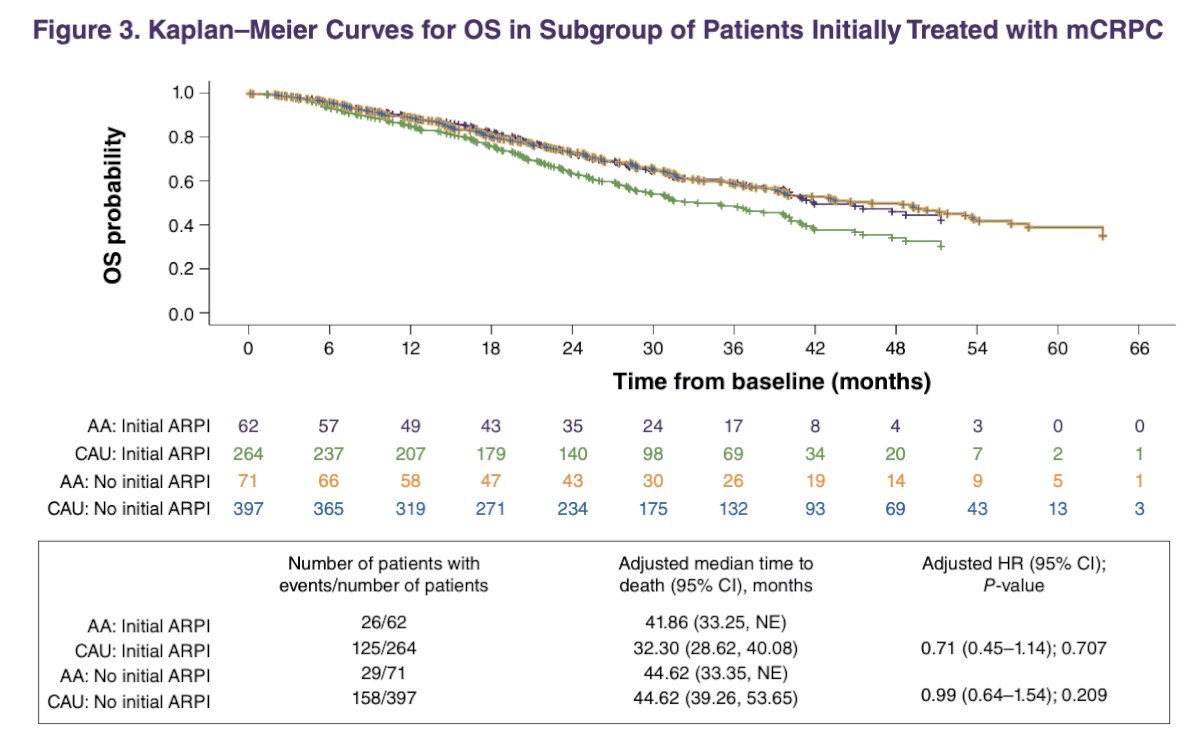
In terms of healthcare resource utilization, fewer Caucasian patients experienced prostate cancer-related hospitalizations and emergency room visits compared to African American patients. The frequency of visits to primary care physicians and other specialists was similar between the two groups (57.9% vs. 60.6%). However, African American patients had fewer visits to the urologist per person-year (2.54 vs. 3.25) but saw oncologists at a comparable rate (3.39 vs. 3.90).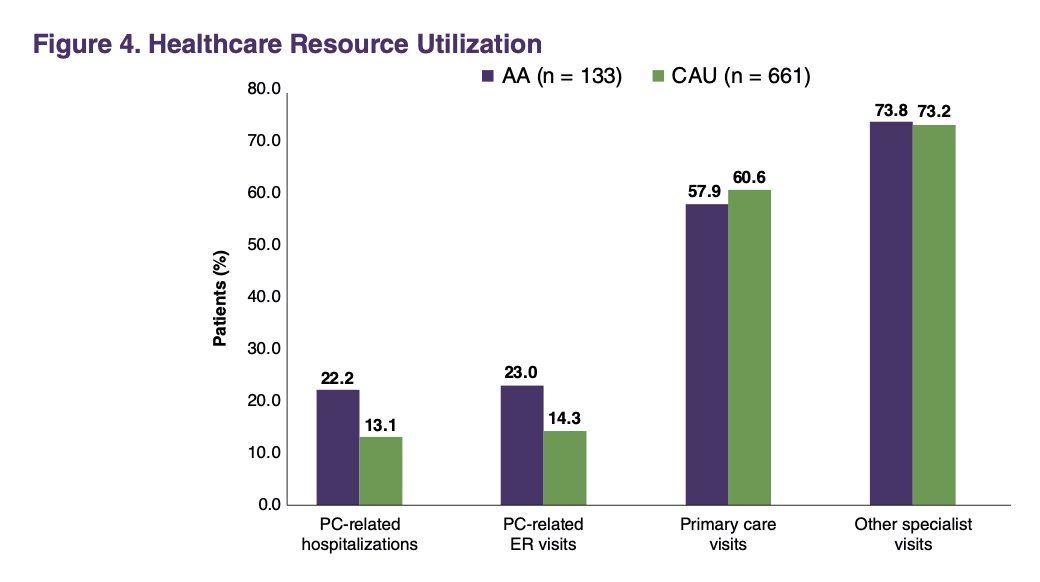
Dr. Hwang concluded her poster presentation with the following key messages:
- African American patients with metastatic castration-resistant prostate cancer tend to be younger and have higher rates of comorbidities and more aggressive disease than Caucasian patients in this post-hoc analysis of TRUMPET
- A higher proportion of African American patients received ARPIs or chemotherapy as initial treatments, while more Caucasian patients were treated with radionuclide therapy and immunotherapy.
- There was a trend suggesting better clinical outcomes in African American patients, including improved overall survival in those treated with ARPIs. However, this was not significant.
- Both racial groups visited oncologists and primary care or other specialist physicians at similar rates, but African American patients had fewer visits to the urologist.
Presented by: Clara Hwang, MD, Medical Oncologist at Henry Ford Health System, Detroit, MI.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:
- Vickers AJ, Mahal B, Ogunwobi OO. Racism Does Not Cause Prostate Cancer, It Causes Prostate Cancer Death. J Clin Oncol. 2023 Apr 20;41(12):2151-2154. doi: 10.1200/JCO.22.02203. Epub 2023 Jan 24. PMID: 36693227; PMCID: PMC10448930.


