(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Abstract/Posters Session. Dr. Umar Ghaffar presented a Comparative Analysis of PSMA-PET Imaging in Detecting Radio-recurrent Prostate Cancer Above and Below Phoenix Criteria Thresholds.
External beam radiotherapy (EBRT) is a standard curative treatment for localized prostate cancer. However, around 8–13% of patients treated with EBRT and androgen deprivation therapy (ADT) experience biochemical recurrence (BCR) within five years, defined by the Phoenix criteria (a PSA rise ≥ 2 ng/ml above the nadir).
There are concerns about the Phoenix criteria, which were developed using conventionally fractionated EBRT, as newer radiation techniques may have different PSA kinetics that have yet to be explored. Additionally, while periodic PSA testing is cost-effective, it cannot reliably distinguish between local and distant recurrences. Moreover, conventional imaging also has limitations at lower PSA levels.
PSMA-ligand PET/CT, however, shows higher sensitivity and detection rates, even for PSA values below 0.5 ng/ml, enhancing its role in evaluating BCR. Dr. Ghaffar mentioned that the aim of this study was to assess the performance of PSMA-ligand PET/CT in patients with rising PSA following radiotherapy, comparing those with PSA levels above and below the Phoenix threshold (PSA ≥ 2 ng/ml above the nadir).
The investigators conducted a retrospective review of PSMA-PET scans in patients with biochemical recurrence following RT. The primary outcome of the study was the lesion detection rate, which was defined as any positive finding on PSMA-PET. Local and oligometastatic recurrences identified on imaging were considered potentially salvageable, meaning they could be suitable for focal salvage therapies.
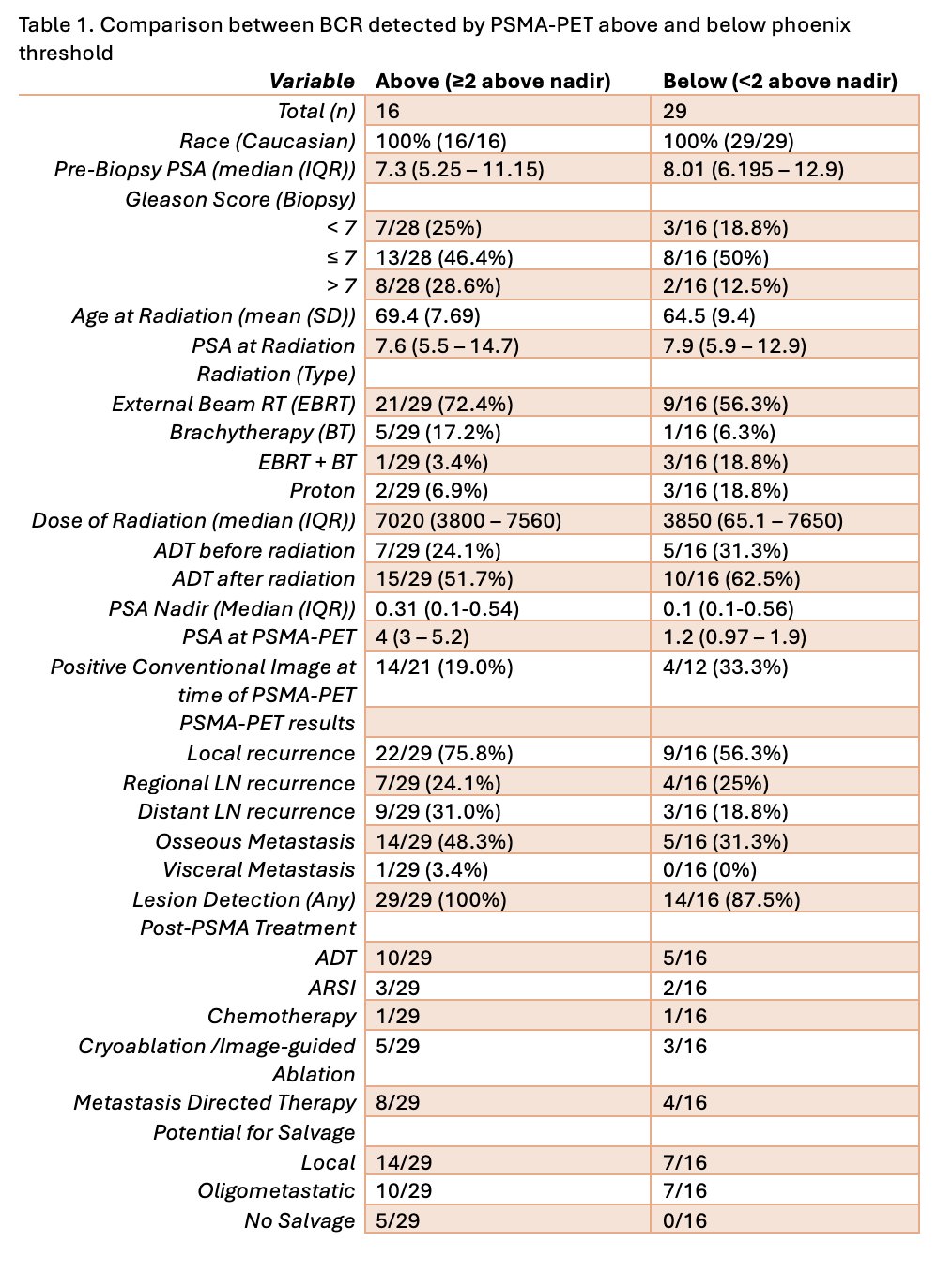
A total of 45 patients with BCR after RT were identified, among this, 29 above Phoenix threshold and 16 below the threshold for BCR were assessed by PSMA-PET. Prebiopsy PSA and age at radiation were comparable in both groups. ADT was utilized after radiation in 51.7% of patients above the threshold and 62.5% below. Median PSA nadir was 0.31 above and 0.1, while PSA at PSMA-PET was 4ng/ml above and 1.2 below the Phoenix threshold groups, other clinical and demographic characteristics are shown below:
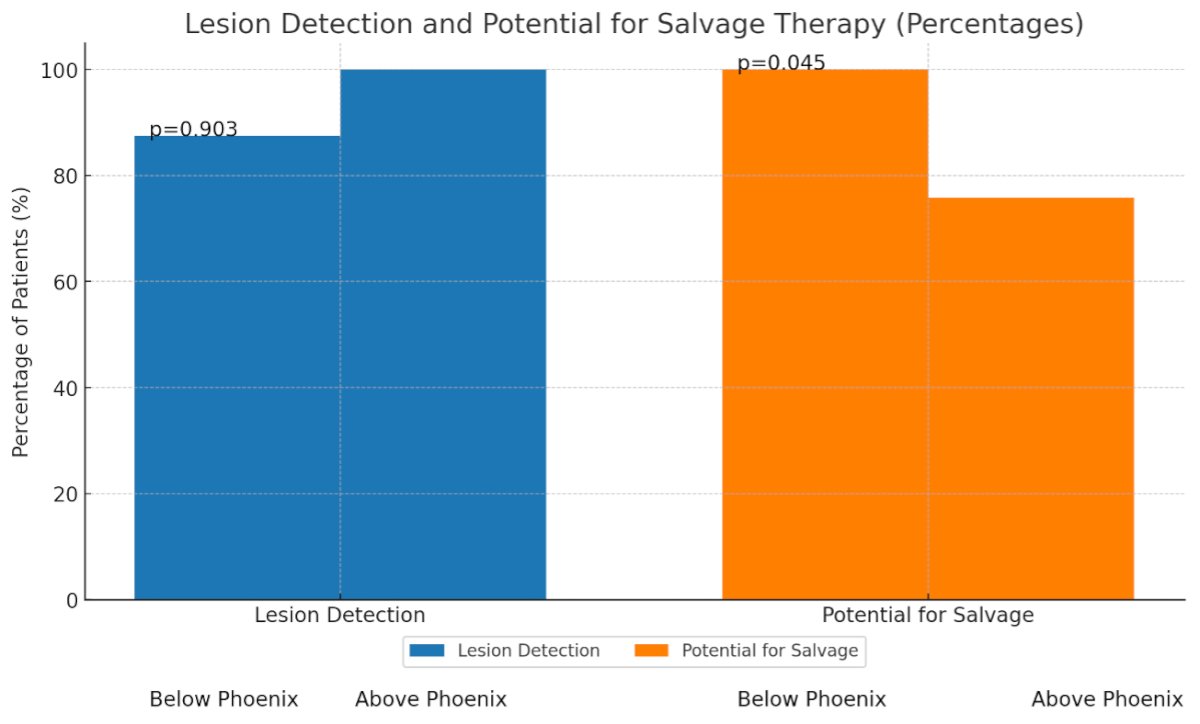
The lesion detection was comparable below and above Phoenix threshold (14/16 (87.5%) vs 29/29 (100%), respectively (p=0.903).
Furthermore, there was a significantly higher proportion of patients with disease potentially amenable to salvage therapy when the PSA was below the Phoenix threshold vs above 100% vs. 76.8% (p=0.045), as shown in the graphic below:
Post-PSMA treatments included:
- ADT (34.5% ≥2 and 31.3% <2)
- ARPI (10.3% ≥2 and 12.5% <2)
- Chemotherapy (3.4% ≥2 and 6.3% <2)
- Cryoablation/image-guided ablation (17.2% ≥2 and 18.8% <2)
- Metastasis-directed therapy (27.6% ≥2 and 25% <2).
Dr. Ghaffar concluded his presentation with the following remarks:
- PSMA-PET shows significant efficacy in detecting lesions even in patients with PSA levels below the Phoenix criteria for biochemical recurrence (BCR).
- Lesions detected below the Phoenix threshold by PSMA-PET can potentially be identified early.
- Early lesion detection with PSMA-PET may allow for PSMA-guided salvage therapy.
- This underscores the utility of PSMA-PET in the early detection and management of recurrent prostate cancer.
- The ability of PSMA-PET to detect lesions early provides opportunities for timely and targeted treatment interventions.
Presented by: Umar Ghaffar, MD, Research Fellow in Urology at Cedars-Sinai Health Sciences University - Los Angeles, CA.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.


