(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, TX between December 3rd – 6th, 2024 was host to a prostate cancer session. Dr. Soroush Rais-Bahrami discussed the use of biparametric or non-contrasted prostate MRIs, as well as the incorporation of biomarkers in this setting.
Where have we been with prostate MRIs? This imaging tool has shifted the prostate cancer detection paradigm, forging a new frontier for biopsying at-risk patients. It is a non-invasive imaging tool for tissue characterization, helping define the underlying risk of prostate cancer. It has led to enriched, targeted biopsy sampling with an improved yield for the detection of clinically significant prostate cancer.
Currently, multi-parametric MRIs are performed using multiple sequences in a 45-to-60-minute time frames, using the following phases:
- T2-weighted (T2W)
- Diffusion-weighted imaging (DWI)
- Dynamic contrast-enhanced (DCE)
There has been a broad adoption and integration of prostate MRIs in multiple settings:
- Patients with prior negative biopsies
- Patients on active surveillance
- Biopsy-naïve men with screening PSA or DRE concerns
- Patients with disease recurrence following radiotherapy or ablations
Where should we be going with prostate MRIs? For pre-biopsy imaging, Dr. Rais-Bahrami argued that there are benefits to eliminating contrast administration during prostate MRIs for the following reasons:
- Eliminating the risk of gadolinium deposits and buildup in the central nervous system
- Decreased MR gantry time per study allowing for better use of shared resources
- Added opportunity and realized cost with IV access, contrast material, and increased complexity of interpretation
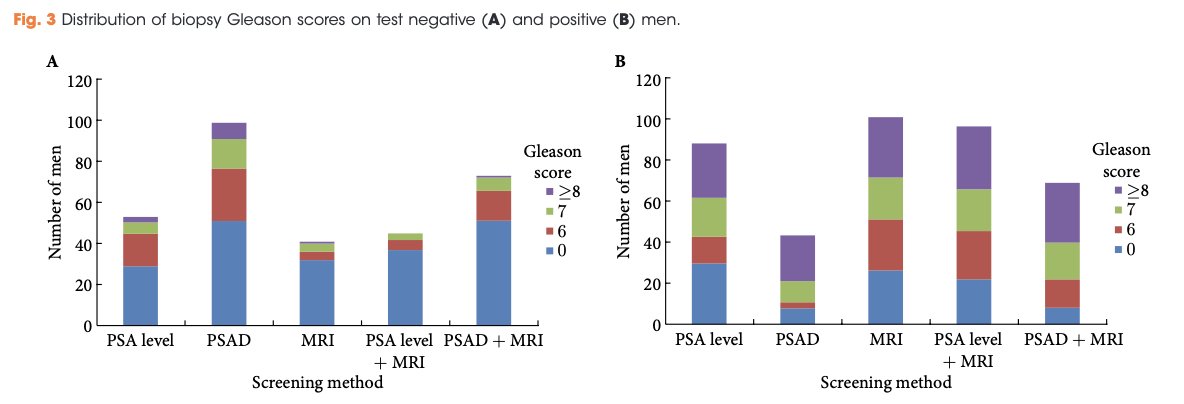
What is the diagnostic yield of biparametric (T2- and diffusion-weighted) prostate MRIs for cancer detection in biopsy-naïve men? In 2015, Dr. Rais-Bahrami and colleagues demonstrated that biparametric MRI performs well for prostate cancer detection with an area under the curve (AUC) of 0.80. This AUC can be further improved to up to 0.87 when combining these imaging results with the PSA and PSA density parameters.1
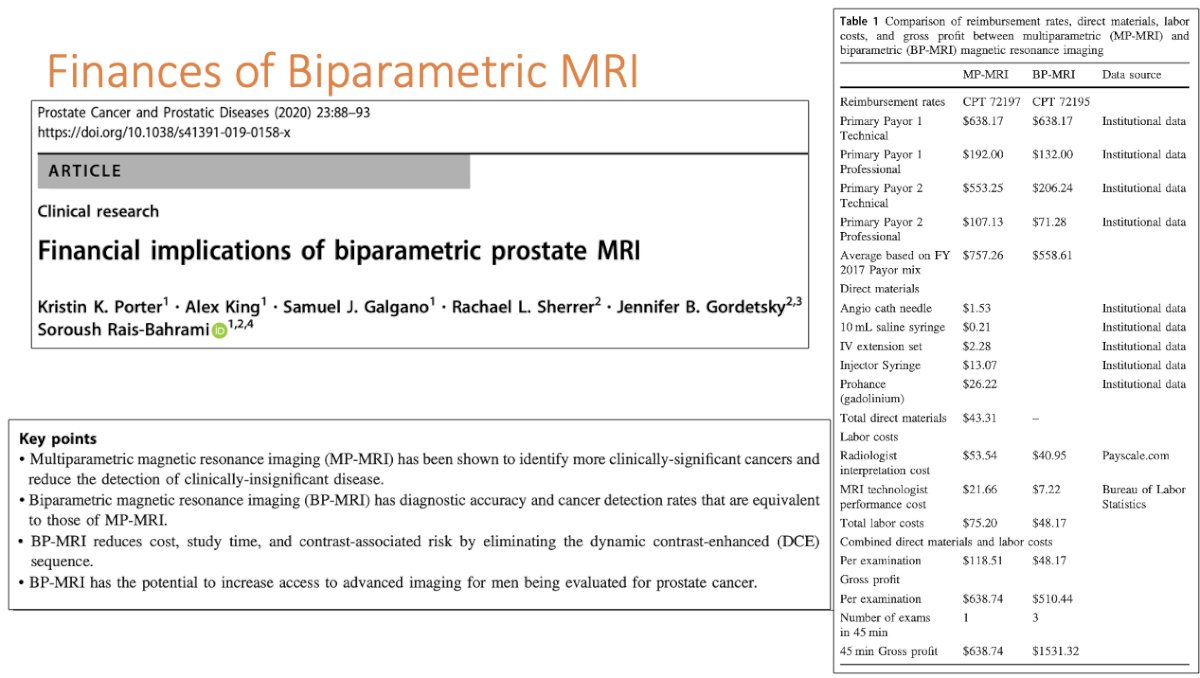
In addition to the potential health benefits with the avoidance of contrast administration, the use of biparametric MRIs has been shown to be associated with lower costs. When controlled for a 45-minute time window that allows for one full mpMRI or three full biparametric MRI studies, the biparametric MRI 45-minute gross profit was shown to be $1,531.32. This represents an increase in gross profit of $892.58 for the 45-minute time window or $10,710.98 in a 9 hour business day when performing biparametric MRI compared to multiparametric MRI for prostate cancer detection.2
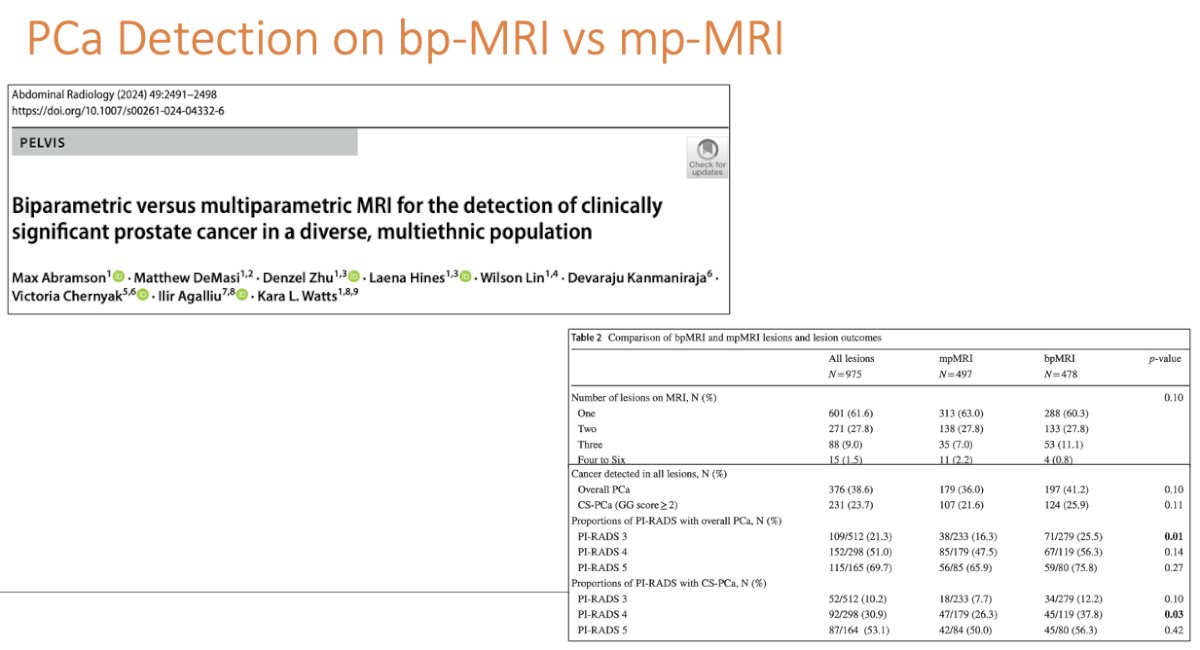
At this point, biparametric MRI has been shown to be cost-effective, compared to multiparametric MRI. But, what about its diagnostic performance for prostate cancer detection, compared to multiparametric MRI? In a retrospective analysis of 556 men with 975 PI-RADS 3-5 lesions on MRI who underwent an image-guided fusion prostate biopsy at a single institution between 2016 and 2021, the odds of detecting overall (OR: 1.19, p=0.031) and clinically significant prostate cancer (OR: 2.15, p=0.014) on fusion biopsy were higher for lesions identified on biparametric MRI, compared to multiparametric MRIs.3
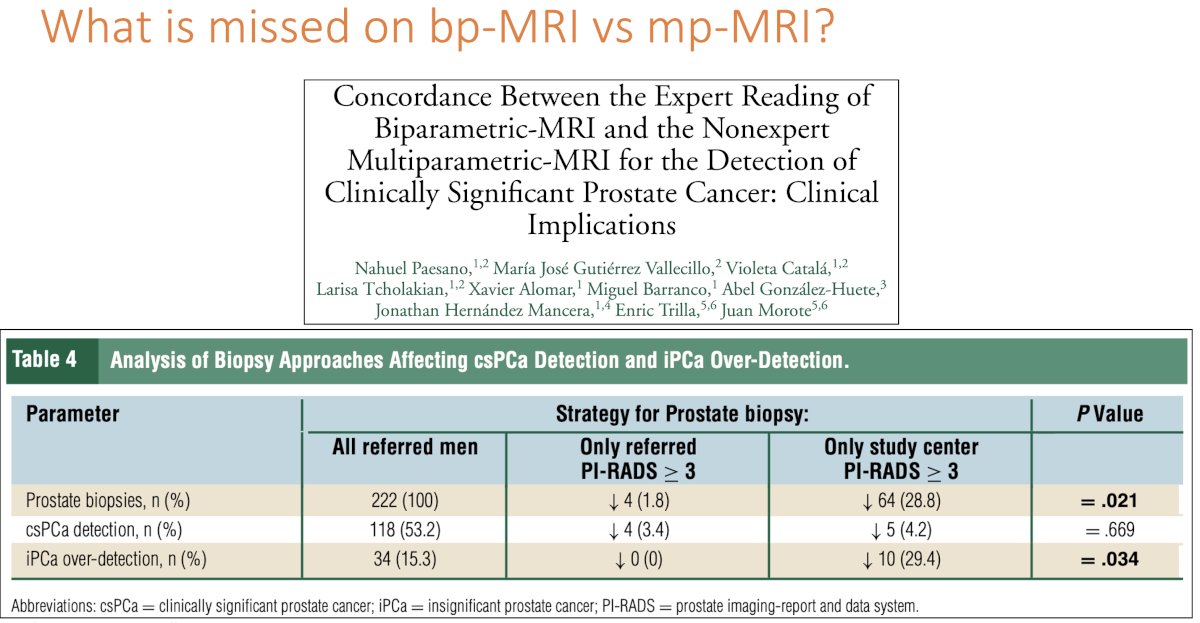
What is the value of the DCE phase? In other words, what is missed on biparametric MRIs, compared to multiparametric MRIs? Two hundred twenty-two men suspected of having prostate cancer and who had an mpMRI reported by nonexpert radiologists were referred to a reference center for transperineal MRI-TRUS fusion biopsy where an expert radiologist reported the biparametric MRI PI-RADS 2.1 and segmentation, blinded to external mpMRI. Mapping targeted suspected lesions and 12-core systematic biopsies were subsequently performed. Concordance between both PI-RADS was observed in 49% of cases (Kapp index=0.29). Expert reclassification to lower PI-RADS occurred in 46% of cases, while an increase was observed in 5% only. Agreement existed in 31% of nonexpert PI-RADS 3, 44% of PI-RADS 4, and 84% of PI-RADS 5 lesions. Potential clinical implications included a 27% reduction in prostate biopsies when using expert biparametric MRI readings, compared to nonexpert mpMRI readings. Reliance on the expert biparametric reading would lead to missing 4.2% of clinically significant prostate cancer lesions, compared to 3.4% with non-expert mpMRI. Over-detection reduction of insignificant PCa was 29.4% and 0%, respectively.4
Dr. Rais-Bahrami argued that the time is now to incorporate biparametric MRI along with secondary screening filters, such as Prostate Health Index, 4Kscore®, PCA3, SelectMDx, ExoDx, and use expanding imaging study options, including:
- PSMA PET
- Tissue elastography
- Microultrasound
- Microbubble contrast enhanced ultrasound
- Histoscanning
Dr. Rais-Bahrami concluded his presentation advocating for the use of the best tools available for the:
- Effective detection of clinically significant prostate cancer
- Efficient utilization of available resources to optimize the time available, patient access, and safety
- Minimization of overdetection of low-risk disease
Presented by: Soroush Rais-Bahrami, MD, Professor of Urology and Radiology, Department of Urology, University of Alabama, Birmingham, AL
Written by: Rashid K. Sayyid, MD, MSc – Robotic Urologic Oncology Fellow at The University of Southern California, @rksayyid on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, TX between December 3rd and 6th, 2024
References:- Rais-Bahrami S, Siddiqui MM, Vourganti S, et al. Diagnostic value of biparametric magnetic resonance imaging (MRI) as an adjunct to prostate-specific antigen (PSA)-based detection of prostate cancer in men without prior biopsies. BJU Int. 2015; 115(3):381-8.
- Porter KK, King A, Galgano SJ, et al. Financial implications of biparametric prostate MRI. Prostate Cancer Prostatic Dis. 2020; 23(1):88-93.
- Abramson M, DeMasi M, Zhu D, et al. Biparametric versus multiparametric MRI for the detection of clinically significant prostate cancer in a diverse, multiethnic population. Abdom Radiol (NY). 2024; 49(7):2491-8.
- Paesano N, Vallecillo MJG, Catala V, et al. Concordance Between the Expert Reading of Biparametric-MRI and the Nonexpert Multiparametric-MRI for the Detection of Clinically Significant Prostate Cancer: Clinical Implications. Clin Genitourin Cancer. 2024; 22(6):!02233.


