(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, TX between December 3rd – 6th, 2024 was host to a prostate cancer session. Dr. John Davis discussed the incorporation of artificial intelligence into the surgical care paradigm of prostate cancer patients to facilitate live remote surgery.
What was the state of telesurgery 20 years ago? At that time, the remote surgeon could only telestrate and move the camera. The pros of such an approach were the opportunities to teach/proctor surgeons remotely, and this was seen as an impressive demonstration and an academic niche. There were numerous issues, however, including license barriers, high costs, reimbursement difficulties, patient acceptance issues, and the absence of sustainable interest.
Fast-forward to today, there have been significant updates in transmission speed, latency, and connection stability. Remote surgeons now can have full control, as opposed to just controlling the camera. As such, there has been renewed interest in telesurgery worldwide. However, barriers remain – namely, licensing, ethics, reimbursement, and sustained interest beyond demonstrations and feasibility.1
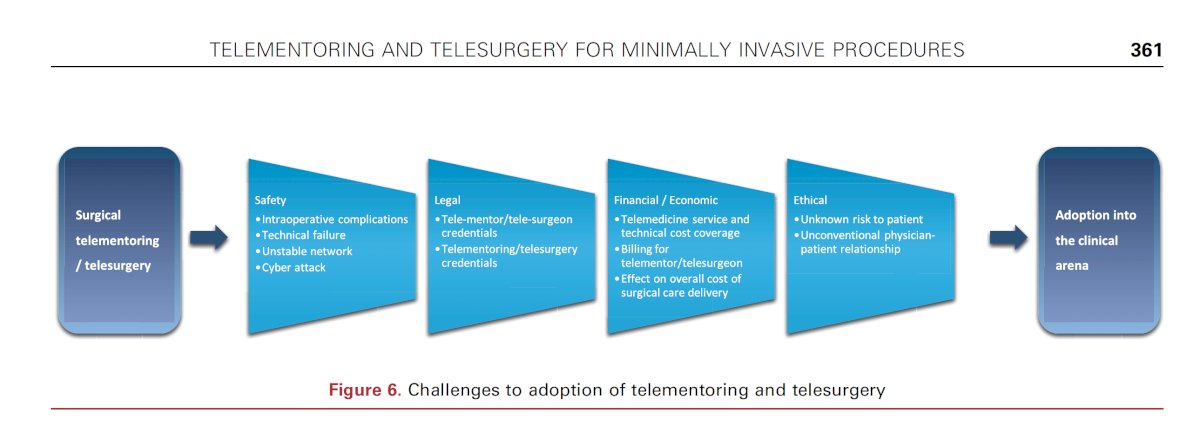
The contemporary challenges to telementoring and telesurgery for minimally invasive procedures were comprehensively reviewed by Hung et al. in 2018.2 These can be summarized under the following headings:
- Safety
- Intra-operative complications
- Technical failure
- Unstable network
- Cyberattacks
- Legal:
- Telementor/telesurgeon credentialing
- Telementoring//telesurgery credentials
- Financial/economic
- Telemedicine service and technical cost coverage
- Billing for telementor/telesurgeon
- Effect on overall cost of surgical care delivery
- Ethical
- Unknown risk to patient
- Unconventional physician-patient relationship
Despite these challenges, there are obvious upsides to the use of telesurgery, including:
- Demonstration of novel technology
- Mentoring
- New procedures/platforms
- Recent trainees or surgeons inexperienced with minimally invasive techniques
- Billing motivations
- Networked health care system
- Patient access to care, both domestically and internationally
- Overcoming surgeon shortages
- Improving the efficiency of a surgeon’s workflow
- Can remote cases be performed while turnover is happening between cases at the surgeon’s hospital where he/she is physically located?

Who will lead the change? Dr. Davis argued that it will require both senior surgeons, who can offer elite leadership and resources in this setting, as well as younger, junior surgeons who have the advantages of time, bandwidth, and tend to be more career-focused at this stage of their careers.
How will this change be implemented? Help from other sources, including policy, technology, and patients themselves, will be crucial. Additionally, change enablement training will be crucial to help facilitate adoption, and this framework relies on the pillars of:
- Alignment
- Building
- Lead
- Embracing

At the current time, telesurgery is mostly limited to experts who have demonstrated its feasibility. However, which model will eventually ‘lead’? Will it remain in its current status of mostly experts sporadically performing this or will it evolve to:
- Expert surgeons doing remote surgery continuously?
- Expert surgeons occasionally proctoring a former trainee or an experienced surgeon learning a new procedure?
- A health system setting this up for surgeons to use occasionally?
Additionally, who will solve international issues with liability, credentialing, and reimbursement?
Dr. Davis argued that we need to remove geographic barriers to surgery. By removing barriers to surgery, remote surgery enables us to extend our reach – ensuring patients have access to the right care and the right surgeon. He remarked: “Imagine you are no longer with your patients and your surgical team during a surgery… it changes how you approach your surgery, interact with your care team, prepare, and the entire post-operative experience.” This is what Maxcess Health is designing––a new system of care and the tools and workflows to perform surgery from miles away.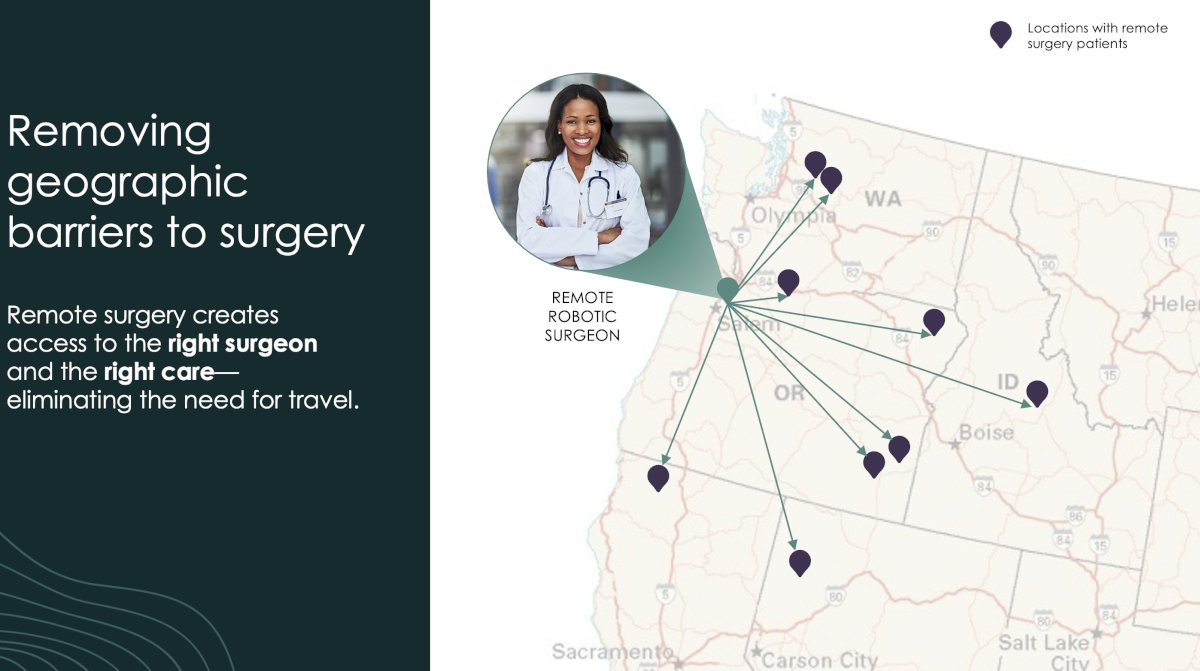
What will it take to enable remote surgery at scale? Following conversations with the robotics companies, many health system leaders, surgeons, and surgical teams, it has been determined that three things need to happen:
- We need to decouple or cut the cord between the surgical controls and the patient side 'arms'. This includes the technology that enables the robots to communicate control signals at a distance and the telecom service level agreements that provide access to the internet with the required reliability and latency.
- When we separate the surgeon from the patient, we are meaningfully disrupting the system of care – or care processes – as we know it. We are also introducing unfamiliarity for each of the players. Across disparate locations, each person in the care process –patient, surgeon, nurses, surgical techs, etc – needs to know their role and be able to execute that role with accuracy. Thus, we need to redesign the system of care and provide a platform to orchestrate the entire journey. This includes hardwiring the care process, automating what we can, enabling operational needs like provider licensing and credentialing, and allowing collaboration among the care team in their various locations.
- As we change the system of care and the role the different players have in the care process and introduce new technologies, we will create appropriate contracting strategies and financial incentives.
Sovato is purpose built to do all of these things in partnership with providers and surgical and interventional robotics manufacturers.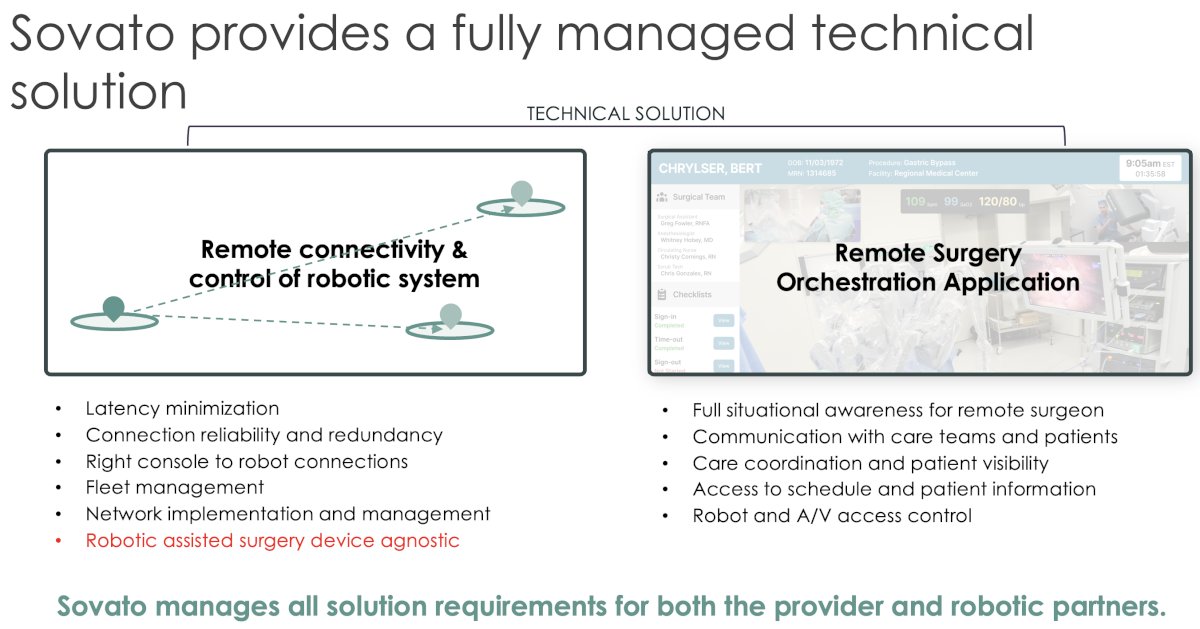
Dr. Davis concluded his presentation with the following quote:
Presented by: John Davis, MD, Professor, Department of Urology, MD Anderson Cancer Center, Houston, TX
Written by: Rashid K. Sayyid, MD, MSc – Robotic Urologic Oncology Fellow at The University of Southern California, @rksayyid on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, TX between December 3rd and 6th, 2024
References:
- Patel V, Saikali S, Moschovas MC, et al. Technical and ethical considerations in telesurgery. J Robot Surg. 2024; 18(1):40.
- Hung AJ, Chen J, Shah A, Gill IS. Telementoring and Telesurgery for Minimally Invasive Procedures. J Urol. 2018; 199(2):355-69.


