(UroToday.com) The 2024 SUO annual meeting included a prostate cancer session, featuring a presentation by Dr. Daniela Wittmann discussing sexual satisfaction despite sexual dysfunction. Dr. Wittmann started her presentation by highlighting what we most associate with sex: experience of pleasure, feeling of intense satisfaction, intimate connection with a partner, and sharing pleasure. However, she notes that none of these absolutely require intact sexual function.
Undoubtedly, urologic cancer treatments save lives, but impair sexual function:
- Surgery: removing whole or parts of genitals (clitorectomy, penectomy, orchiectomy, pelvic exenteration), which interferes with nerve structures and vasculature
- Radiation: causes neuropathy, fibrosis, scarring, and atrophy of genital structures
- Hormonal therapy: causes loss of the biological substrate of sexual function
- Chemotherapy/immunotherapy: alters the quality of skin, particularly the mucosal surfaces
After cancer treatment, patients cope with losses in all domains of their sexual function, including desire, arousal, orgasm, pain with sexual activity, and sexual satisfaction. Moreover, a body altered by cancer and treatment leads to psychological, relationship, and social problems:
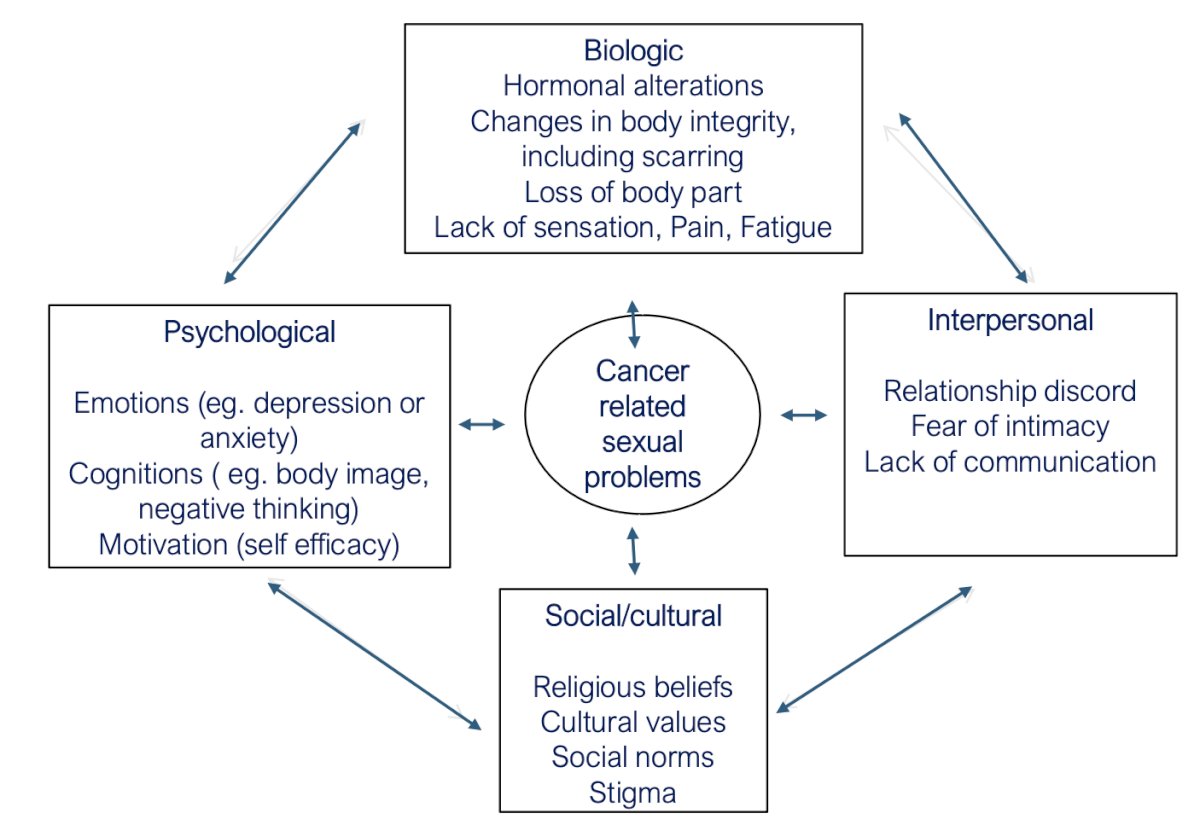
Dr. Wittmann notes that there are unique needs of diverse cultural, ethnic, and racial groups, as well as sexual and gender minorities. In some cultures, sexual dysfunction takes away from the man’s role as the head of the family and marginalizes the partner. There are also unique needs of gay and bisexual men in that they need firmer erections for anal penetration, and ejaculation is meaningful to gay and a bisexual man’s erotic experience.
Both patients and their partners experience a loss of sexual function, familiar sexual interactions, body image, and even potentially status in a social environment that may lead to a mourning process. ‘Disenfranchised grief’ was identified as reluctance of patients and partners to ask for help with sexual problems from clinicians who saved their lives. There is no return to baseline sexual function for most patients, but rehabilitation and recovery of sexual intimacy is possible.
Dr. Wittmann was first author of for the Guidelines for Sexual Health Care for Prostate Cancer Patients.1 For the section on counseling patients and partners about the impact of prostate cancer on biopsychosocial aspects of sexuality, Statement 1 is: “A clinician-initiated discussion should be conducted with the patient and the partner (if partnered and culturally appropriate), about realistic expectations of the impact of prostate cancer treatment on the patient’s sexual function, the partner’s experience, and the couple’s sexual relationship. The clinician should promote openness and inclusivity, consider cultural context, and tailor counseling to the specific needs of patients who are heterosexual, gay, bisexual, identify as men who have sex with men, transgender women and gender non-conforming individuals. (Strong Recommendation; Evidence Strength Grade C).”
Key interventions that help couples recover sexual intimacy after cancer include pre-treatment education, normalization of the process, focusing attention on other areas of sexual pleasure (ears, nipples, stomach, anus, etc), individualization of treatment based on inclusivity, and timely referral to relevant subspecialties. Dr. Wittmann notes that one comment that resonates with her from a patient and partner post-prostatectomy is “I wish I could be back to being unselfconscious (not return of erectile function).”
In a study assessing factors contributing to a more or less successful couples’ sexual recovery from 20 couples with prostate cancer, Dr. Wittman and colleagues2 noted the following:
- Post-surgery positive coping: shared normal grief and mourning, ongoing sexual activity, acceptance of sexual losses, use of sexual aids, partner’s positive interest in sex regardless of menopause
- Post-surgery self-defeating coping: inability to share the grief of sexual losses, no or infrequent sexual activity, relationship problems, stressors, inflexible sexuality, partner’s low or no interest in sex regardless of menopause
The physical pleasure-relational intimacy model of sexual motivation is key to maintaining satisfying sex after prostate cancer treatment:3
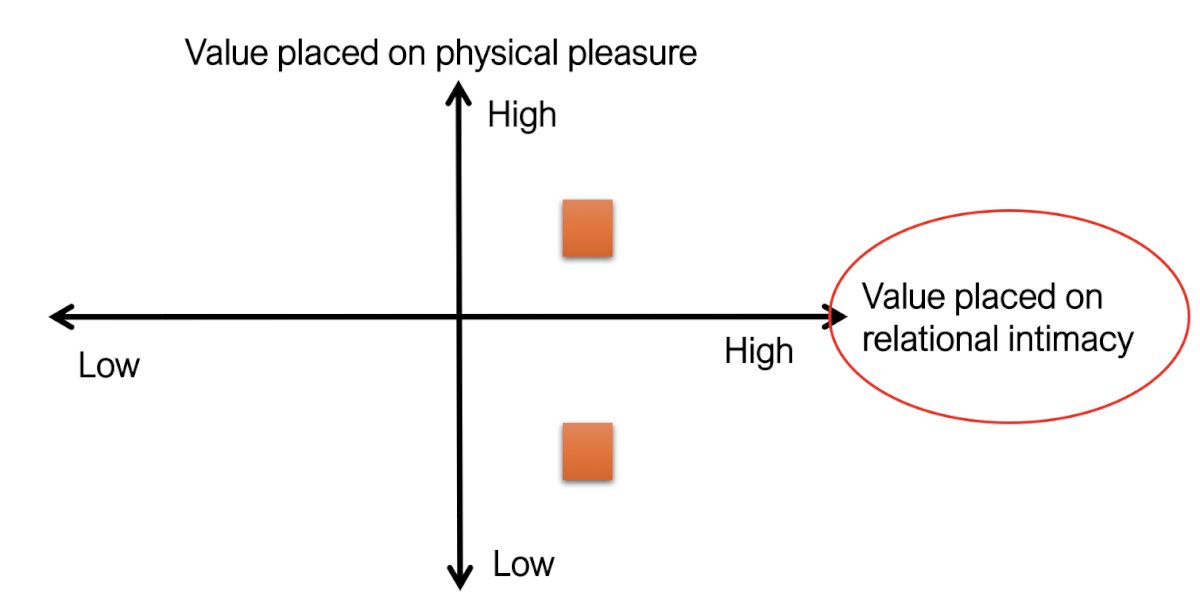
In this qualitative study of 17 men with prostate cancer, the reported factors that enabled couples to retain their sexual relationship were acceptance, flexibility, and persistence.
McInnis et al.4 sought to investigate the relationship among sexual functioning, sexual script flexibility, and sexual satisfaction in 61 individuals diagnosed with prostate cancer via a cross sectional survey. Overall, they found that greater sexual script flexibility was associated with a greater likelihood of being sexually satisfied: 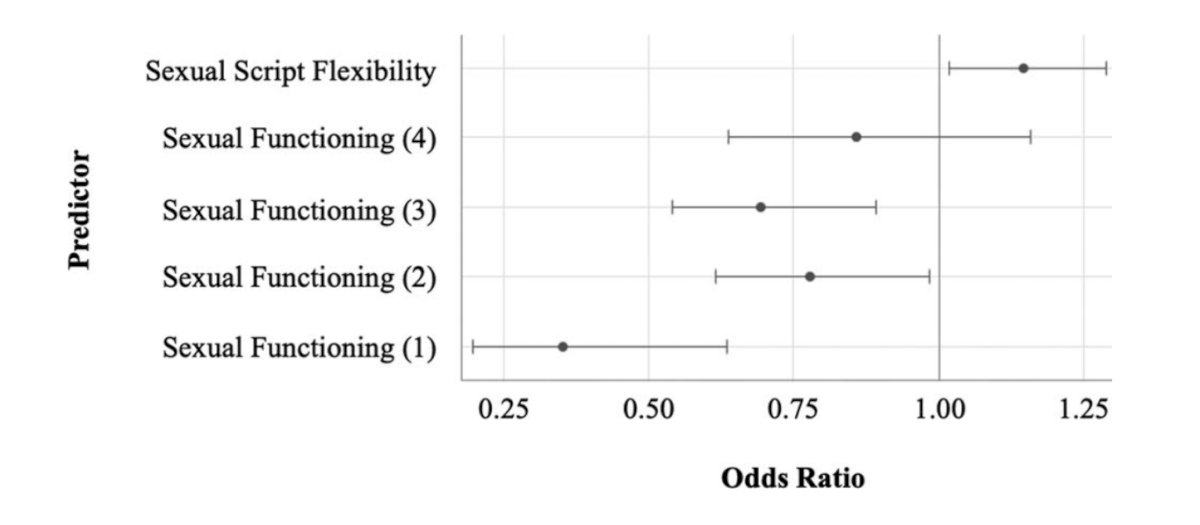
Dr. Wittmann concluded her presentation discussing sexual satisfaction despite sexual dysfunction with the following take home messages:
- Cancer has a significant impact on patients’ sexual function. Both patients and partners are affected
- Most patients do not return to baseline sexual function, but rehabilitation in all the biopsychosocial domains of sexuality can lead to recovery of sexual intimacy
- Clinicians must be the ones to ask about sexual concerns in a manner that recognizes individual differences with respect to culture/religion, sexual orientation, and gender identity
- A willingness to deal with sexual loss, couple communication, use of sexual aids, re-eroticization, flexibility, and early engagement in sexual activity are factors associated with more successful recovery of sexual intimacy after cancer despite sexual dysfunction
Presented by: Daniela Wittmann, PhD, University of Michigan, Ann Arbor, MI
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:
- Wittmann D, Mehta A, McCaughan E, et al. Guidelines for Sexual Health Care for Prostate Cancer Patients: Recommendations for an International Panel. J Sex Med. 2022 Nov;19(11):1655-1669.
- Wittmann D, Carolan M, Given B, et al. What couples say about their recovery of sexual intimacy after prostatectomy: toward the development of a conceptual model of couples’ sexual recovery after surgery for prostate cancer. J Sex Med. 2015 Feb;12(2):494-504.
- Beck AM, Robinsono JW, Carlson LE. Sexual values as the key to maintaining satisfying sex after prostate cancer treatment: the physical pleasure-relational intimacy model of sexual motivation. Arch Sex Behav. 2013 Nov;42(8):1637-1647.
- McInnis MK, Pukall CF. Sexual script flexibility after prostate cancer diagnosis: Implications for sexual satisfaction. J Psychosoc Oncol. 2023;41(3):267-276.


