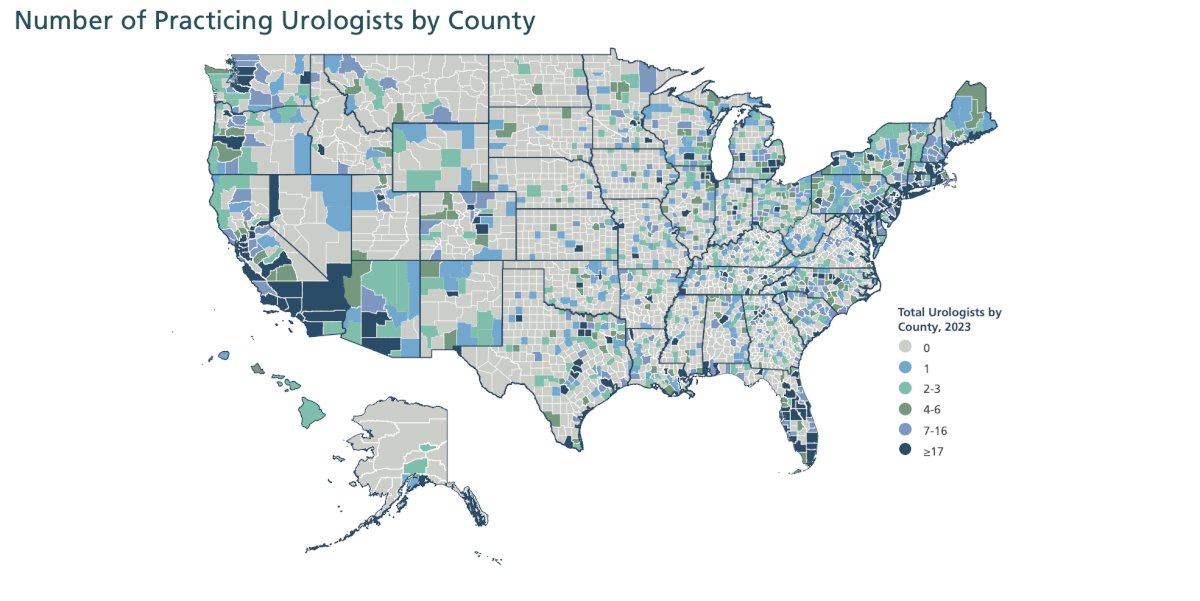
(UroToday.com) The 2024 SUO annual meeting included a health services session, featuring a presentation by Dr. Juan Andino discussing public policy and future directions of telehealth and cancer. The workforce challenges in urology today are highlighted by the AUA’s number of urologists practicing per county:
This leads to a barrier of care, in addition to several other barriers that include structural, physician/clinical factors, and patient factors;1 barriers that telehealth has the potential to mitigate: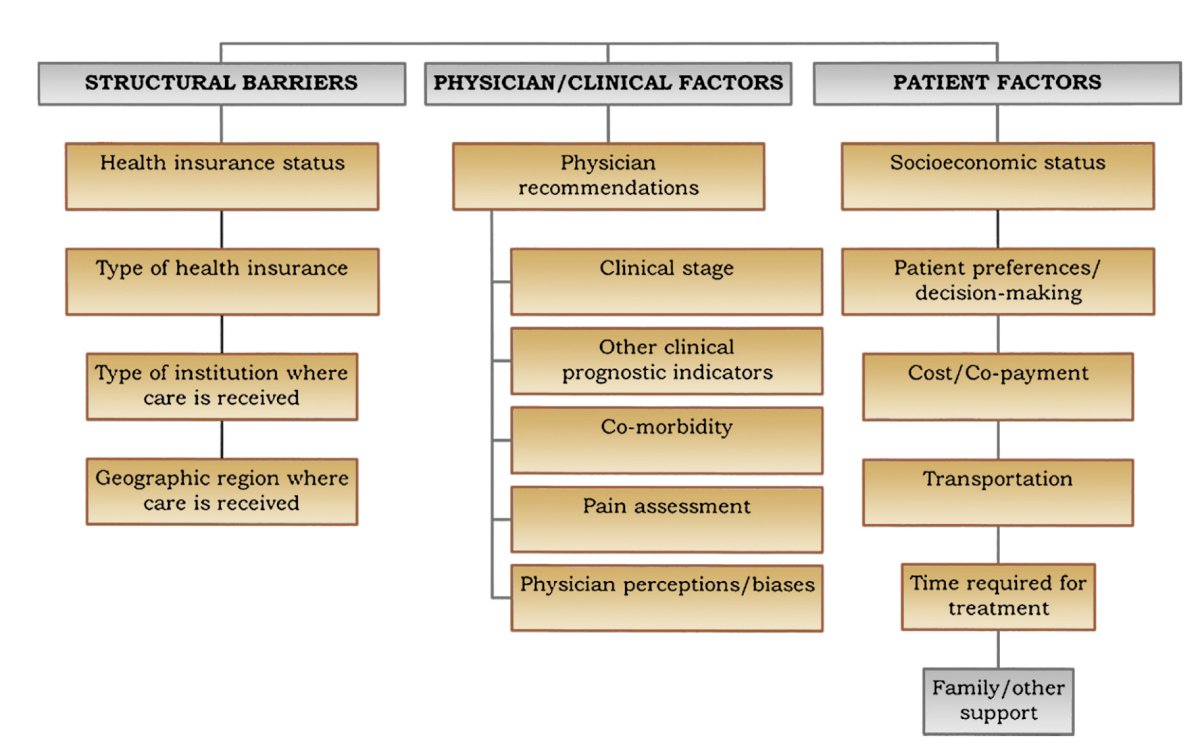
In 2017, Dr. Andino and colleagues examined the value of video visits to patients in an outpatient Urology clinic [2]. This study included an on-site survey of 108 patients at a tertiary medical center's outpatient urology clinic over a 3-month period. Of the patients, 94% owned a device that could be used for a video visit. The median level of patient interest in video visits was reported as 72 out of 100 (IQR 51.25) with a statistically significant difference in interest level across different age groups (p = 0.022). The median amount patients reported they were willing to pay out-of-pocket for video visits was $20 (IQR: $39.25, max: $174). Moreover, this decreased travel distance and time when an examination or procedure was not indicated.
Next, Dr. Andino’s group looked at the impact of a physical exam during a new patient telehealth visit and plans for office or operating procedures [3]. During the COVID-19 pandemic they retrospectively reviewed 590 consecutive urology patients who underwent new patient video visits from March through May 2020 at a single academic center. Overall, 195 (33%) were evaluated by new patient video visits and had a procedure scheduled, of which, 186 (95%) had concordant plans after in-person evaluation. Further, 99% of plans for in-office procedures and 91% for operating room procedures were unchanged.
One of the main goals of telehealth is improving access to care and saving cost. Patel et al.4 recently published a study estimating patient travel, time, and cost savings associated with telehealth for cancer care delivery. The main outcome was estimated patient cost savings from telehealth, which included 2 components: (i) costs of travel and (ii) potential loss of productivity due to the medical visit. Among 25,496 telehealth visits with 11,688 patients there were 4,525 new or established visits and 20,971 follow-up visits. According to cost models, the estimated mean total cost savings ranged from $147.4 (SD $120.1) at $0.56/mile to $186.1 (SD $156.9) at $0.82/mile. For new or established visits, the mean total cost savings per visit ranged from $176.6 (SD $136.3) at $0.56/mile to $222.8 (SD $177.4) at $0.82/mile, and for follow-up visits, the mean total cost savings per visit was $141.1 (SD $115.3) at $0.56/mile to $178.1 (SD $150.9) at $0.82/mile. As such, this model may reduce the financial toxicity of cancer care. Dr. Andino emphasized that telehealth is still patient centric care: 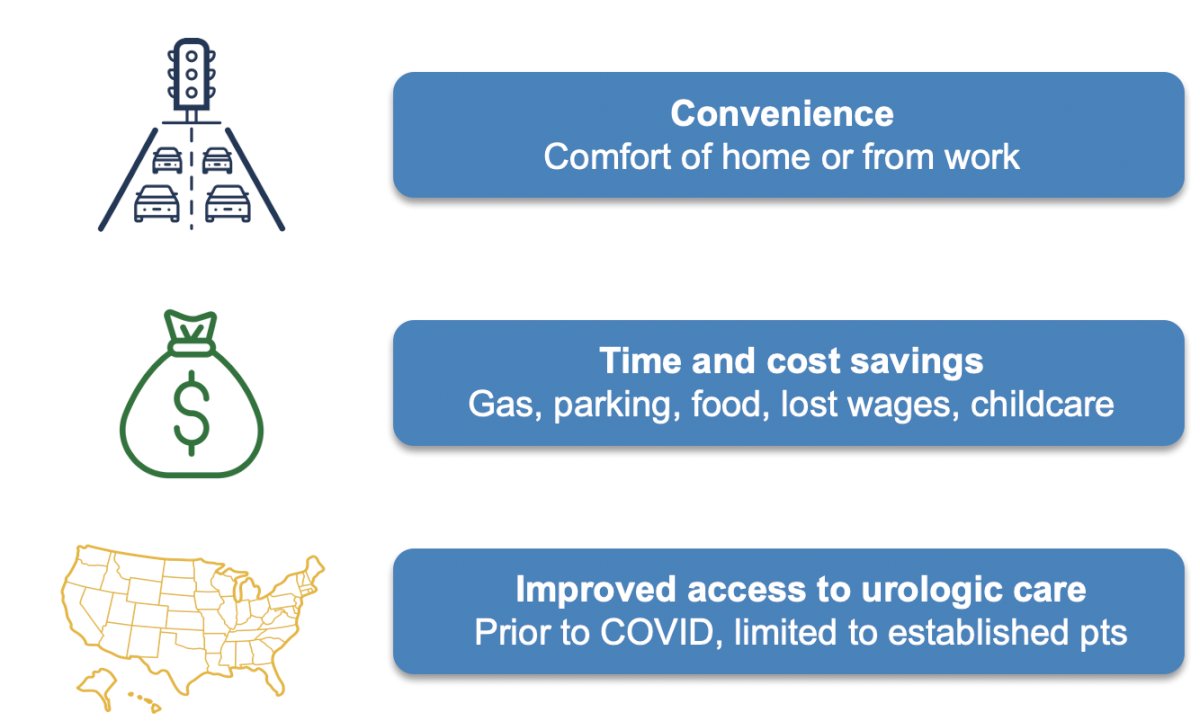
Dr. Andino discussed that based on the Consolidated Appropriations Act, extension of flexibilities pertaining to telehealth are until December 31, 2024. With regards to Medicare, there is a waiver of originating site requirement (ie. the patient can use from home), there is payment parity for telehealth versus in-person visits, and direct supervision includes virtual supervision (which originally ended in 2023, but was extended secondary to provider feedback). Indeed, incentives drive behavior: in Dr. Andino’s 2017 paper2 they not that video visits “could reduce average billing rates.” However, he notes that this is an outdated analysis since it was performed prior to the 2021 billing changes. Billing level for an in-person versus telehealth visit should be the same. Prior to changes in 2021, many practices used time-based billing secondary to a limited exam, but the 2021 changes allow documentation of number and complexity of problems, complexity of data/reviewed, and risks of complications/morbidity or mortality of patient management. However, Dr. Andino notes that future remains unclear and there are many mitigating factors:
- Temporary extension versus permanent solution to health care challenges
- Video versus audio-only (telephone) visits
- Reimbursement parity
- The need for interstate licensure
- Remote monitoring/hospital at home
- The role of artificial intelligence
Dr. Andino concluded his presentation discussing public policy and future directions of telehealth and cancer by encouraging people to register for the AUA 8th annual urology advocacy summit March 3-5, 2025 in Washington, D.C.
Presented by: Juan Andino, MD, MBA, University of California – Los Angeles, Los Angeles, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:
- Ufuah S, Tallman JE, Moses KA. The pursuit of health equity and equality in urologic oncology: Where we have been and where we are going. Eur Urol Focus. 2021 Sep;7(5):929-936.
- Andino JJ, Guduguntla V, Weizer A, et al. Examining the value of video visits to patients in an outpatient Urology clinic. Urology. 2017 Dec:110:31-35.
- Eyrich NW, Andino JJ, Ukavwe RE, et al. The lack of a physician exam during a new patient telehealth visit does not impact plans for office and operating room procedures. Urology. 2022 Sep;167:109-114.
- Patel KB, Turner K, Tabriz AA, et al. Estimated indirect cost saving of using telehealth among nonelderly patients with cancer. JAMA Netw Open. 2023 Jan 3;6(1):e2250211.


