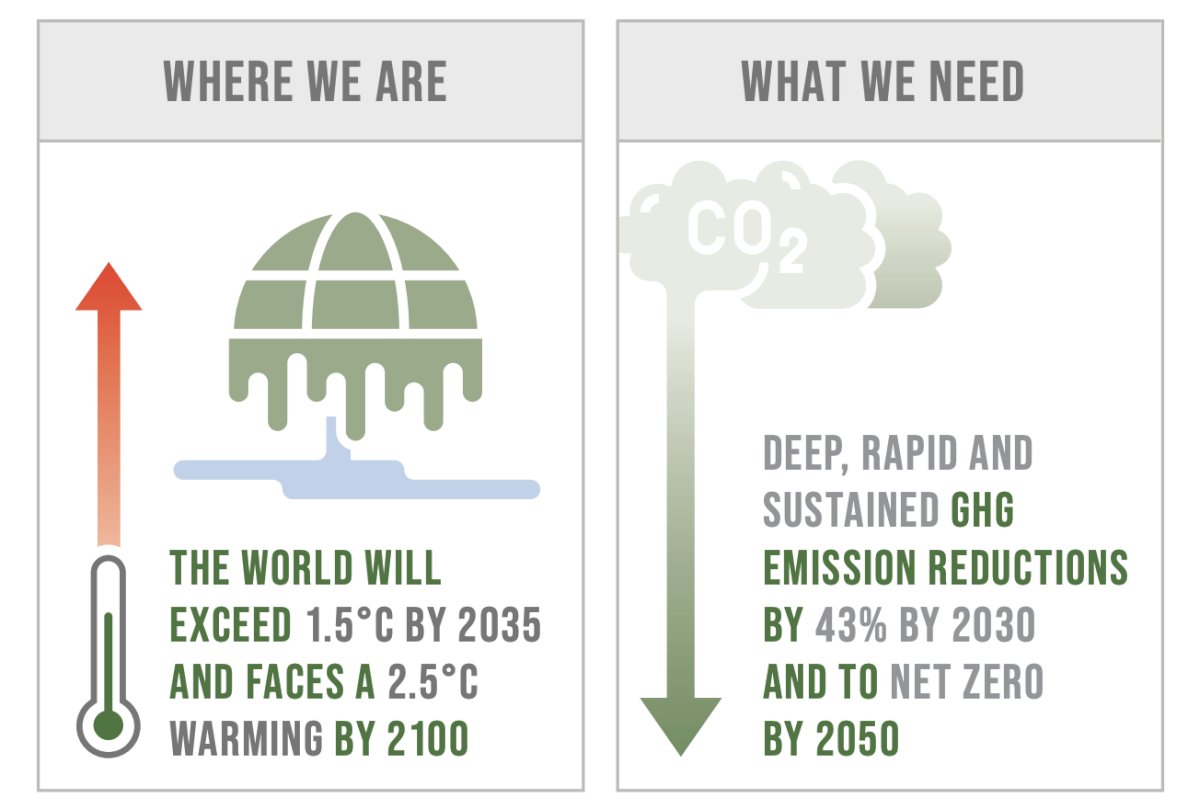
(UroToday.com) The 2024 SUO annual meeting included a prostate cancer session, featuring a presentation by Dr. Michael Leapman discussing sustainability in prostate cancer care. Despite increased pledges and targets to address climate change, current policies still leave the world on course for a ~2.7 °C end-of-century global warming above pre-industrial levels—far from the ambitious aim of the Paris Agreement to limit global warming to 1.5 °C:
Dr. Leapman notes that climate change presents a fundamental threat to human health. It affects the physical environment, as well as all aspects of both natural and human systems – including social and economic conditions and the functioning of health systems. It is therefore a threat multiplier, undermining and potentially reversing decades of health progress. As climate conditions change, more frequent and intensifying weather and climate events are observed, including storms, extreme heat, floods, droughts and wildfires. These weather and climate hazards affect health both directly and indirectly, increasing the risk of death, non-communicable diseases, the emergence and spread of infectious diseases, and health emergencies.
He also emphasized that climate change is also having an impact on our health workforce and infrastructure, reducing capacity to provide universal health coverage. More fundamentally, climate shocks and growing stresses such as changing temperature and precipitation patterns, drought, floods and rising sea levels degrade the environmental and social determinants of physical and mental health. All aspects of health are affected by climate change, from clean air, water and soil to food systems and livelihoods. Further delay in tackling climate change will increase health risks, undermine decades of improvements in global health, and contravene our collective commitments to ensure the human right to health for all: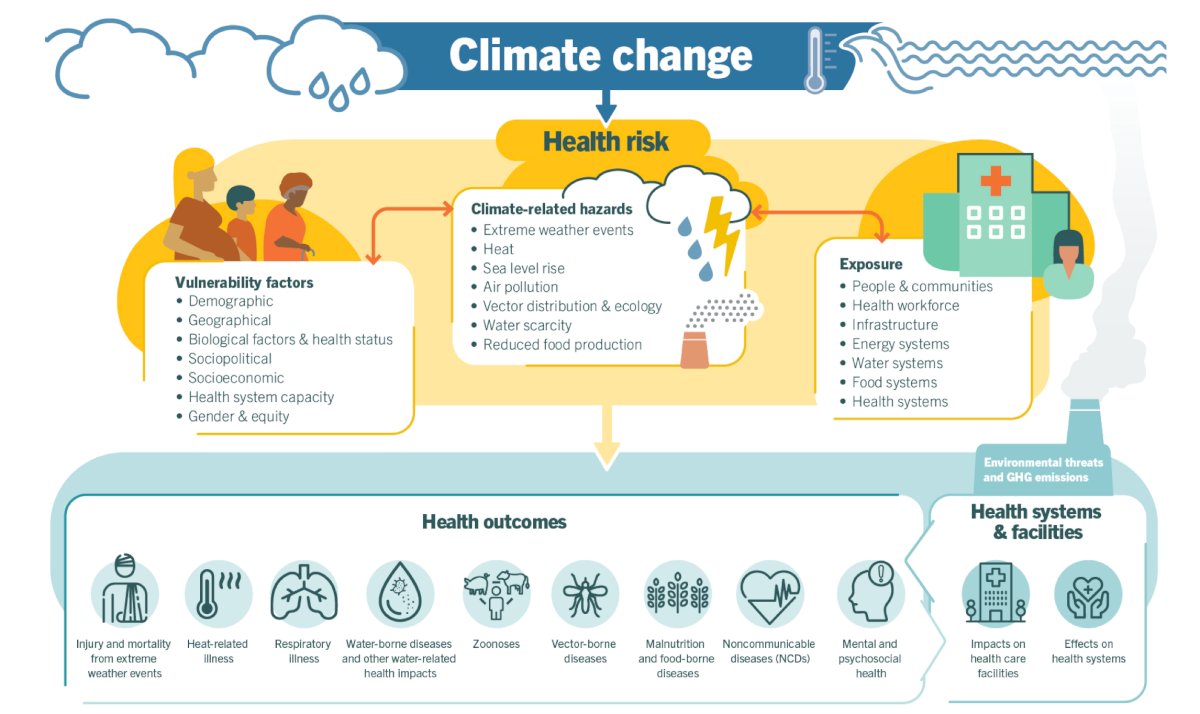
Dr. Leapman notes that nearly 10% of US greenhouse gas emissions are from the healthcare sector, and 1,692 kg/capita of greenhouse emissions for healthcare in the US is the highest in industrialized nations. As follows shows that certain cancers, specifically lung, skin, and gastrointestinal cancer, may be specifically related to greenhouse gas emissions: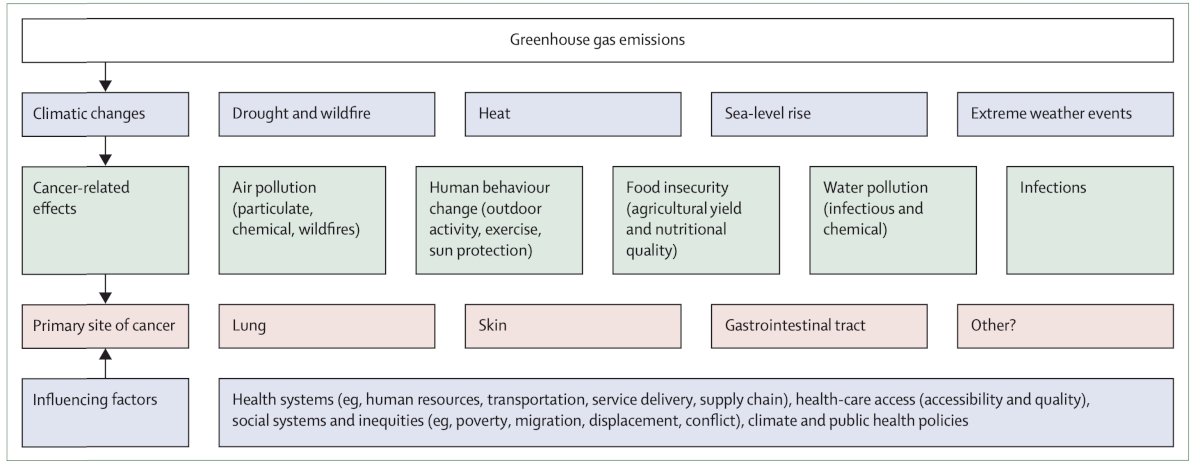
Specific to the healthcare sector, hospitals, profession services, product/supplies, etc are all contributing the environment and health impacts: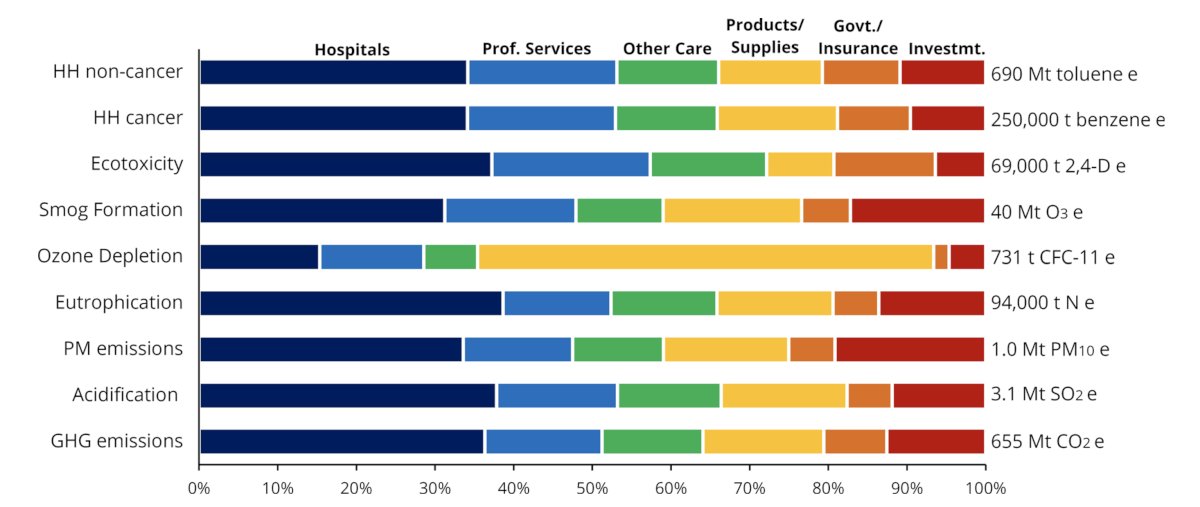
Dr. Leapman emphasized that there are cascading effects of prostate cancer services leading to a carbon footprint, including PSA testing, mpMRIs, prostate biopsy, pathology reporting and subsequent treatment:
Thinking about the total costs of prostate cancer delivery, Dr. Leapman highlighted a 2019 study by Trogdon et al. [1] that estimated a $1.2 billion 3-year Medicare cost for detection of prostate cancer in men older than 70 years of age. Not only is this a significant health care financial cost, but there is also a carbon footprint cost![Thinking about the total costs of prostate cancer delivery, Dr. Leapman highlighted a 2019 study by Trogdon et al. [1] that estimated a $1.2 billion 3-year Medicare cost for detection of prostate cancer in men older than 70 years of age. Not only is this a significant health care financial cost, but there is also a carbon footprint cost](/images/com-doc-importer/184-suo-2024/suo-2024-sustainability-in-prostate-cancer-care/image-5.jpg)
Low volume prostate cancer care has little to no benefit, has potential harm, and incurs costs and resources. Over-screening is in the form of 38% of Medicare Advantage patients receiving low-value PSA screening, and for every $1 spent on low value PSA cancer screening, an additional $6 is spent on follow-up care. Assessing the prostate biopsy life cycle, there is an environmental impact over the course of the entire life cycle of a product, material, process or other measurable activity:2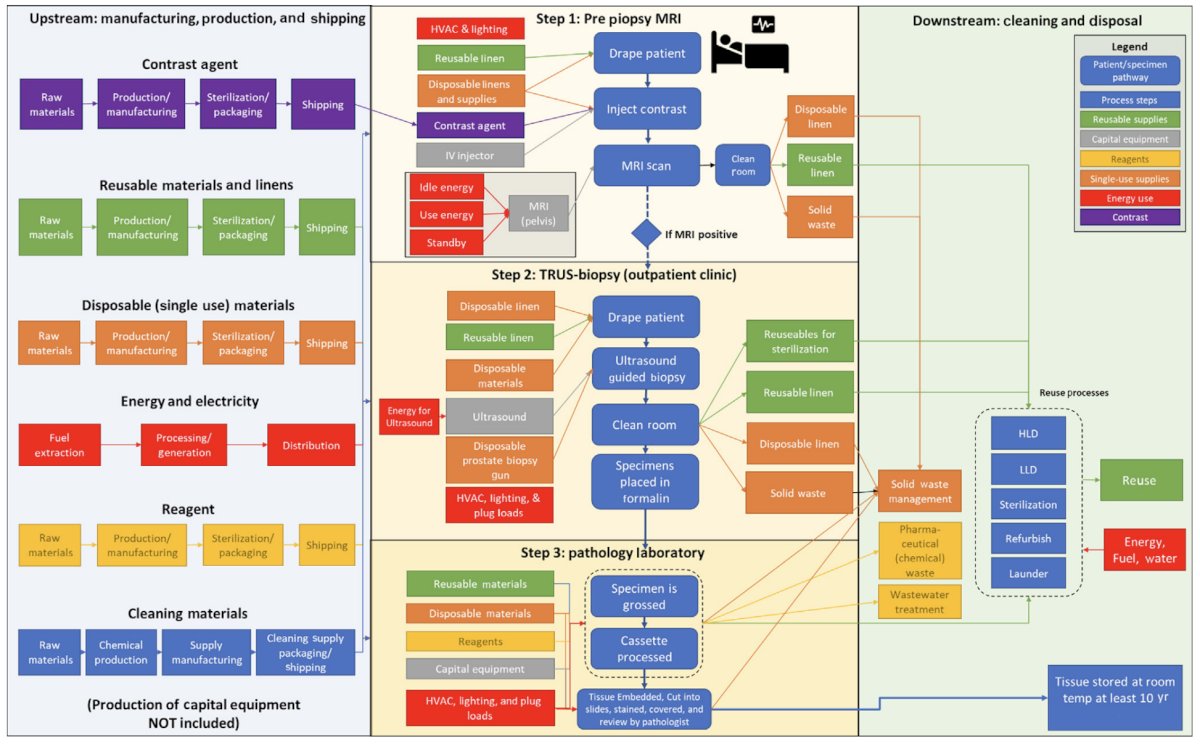
In 2023, Dr. Leapman and colleagues assessed the environmental impact of prostate MRI and transrectal ultrasound prostate biopsy.2 The methodology included a cradle-to-grave life cycle assessment of prostate biopsy, including data from materials and energy inventory, patients and staff travel contributing to prostate MRI, transrectal ultrasound guided prostate biopsy, and pathology analysis. They found that a single transrectal prostate biopsy procedure including prostate MRI, and targeted and systematic biopsies emits an estimated 80.7 kg CO2e. An approach of MRI targeted cores alone without a systematic biopsy generated 76.2 kg CO2e, a systematic 12-core biopsy without mpMRI generated 36.2 kg CO2e, and bpMRI with targeted and systematic biopsies generated 70.5 kg CO2e. mpMRI alone contributed 42.7 kg CO2e (54.3% of baseline scenario). Energy was the largest contributor, with an estimated 38.1 kg CO2e, followed by staff travel (20.7 kg CO2e) and supply production (11.4 kg CO2e):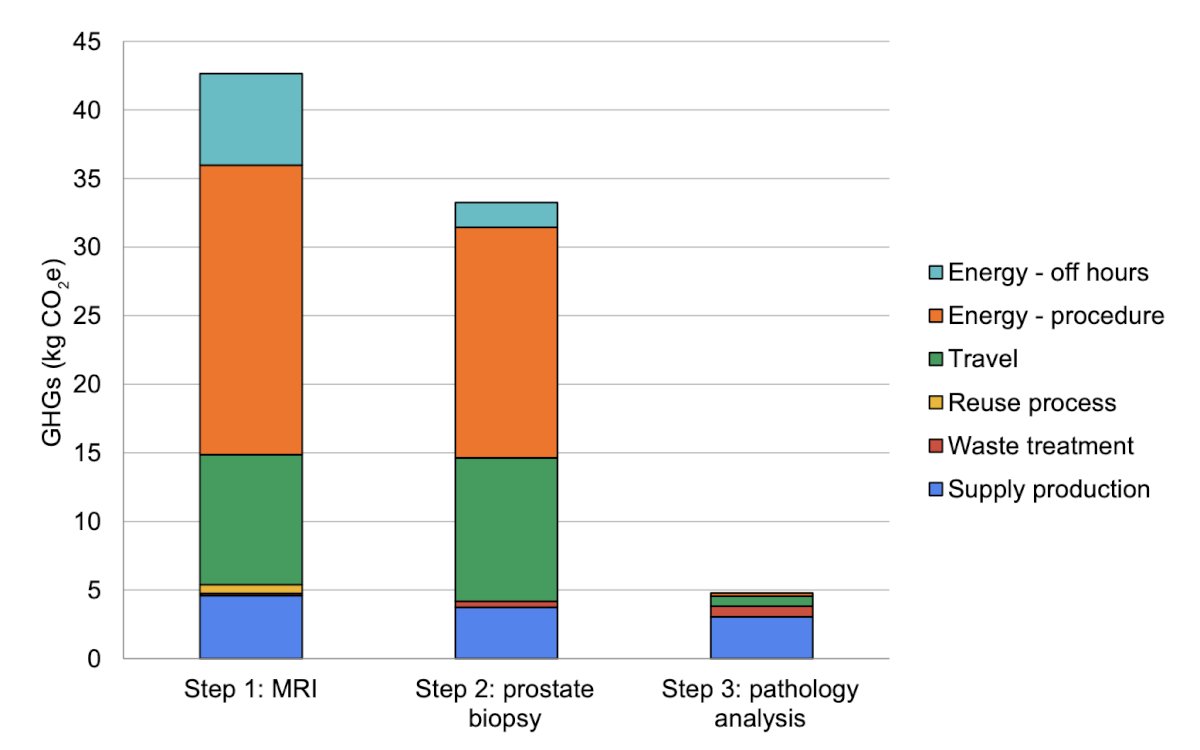
A strategy of a 12-core systematic biopsy without prostate MRI generated the fewest emissions (36.2 kg CO2e), the majority of which (33.0 kg CO2e, 91.3%) were contributed by the biopsy procedure itself and 3.2 kg CO2e (8.7%) from pathology analysis: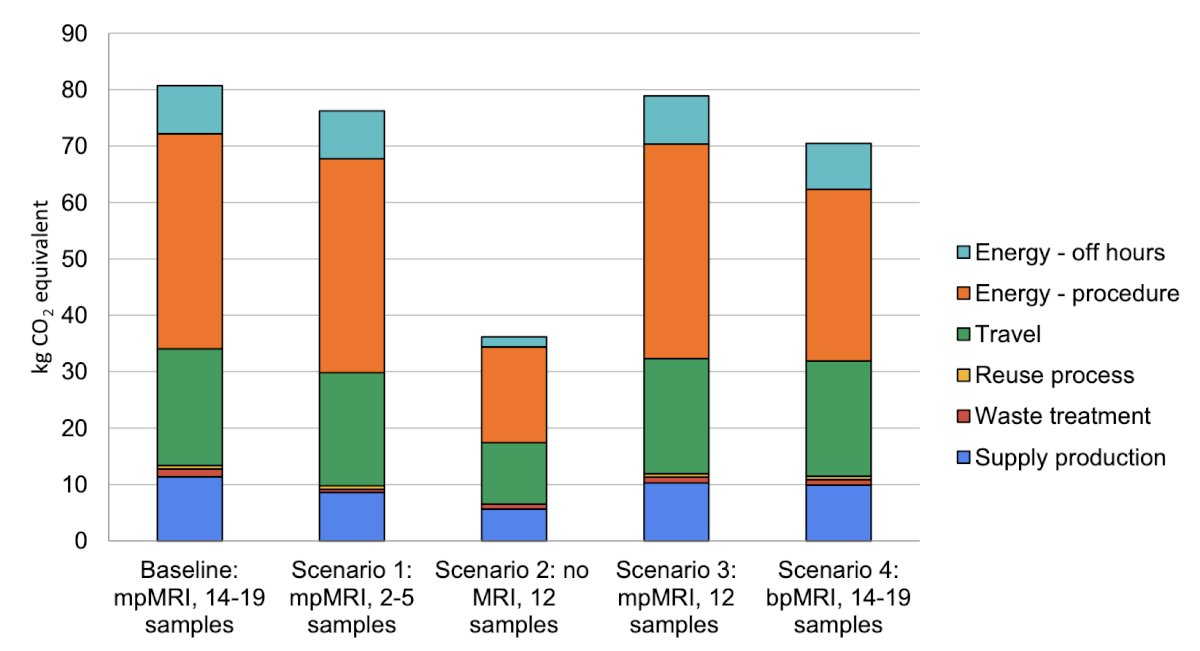
Performing 100,000 fewer unnecessary biopsies would avoid 8.1 million kg CO2e, the equivalent of 4.1 million liters of gasoline consumed. Per 100,000 patients, the use of prostate MRI to triage prostate biopsy and guide targeted biopsy cores would save the equivalent of 1.4 million kg of CO2 emissions, the equivalent of 700,000 liters of gasoline consumed: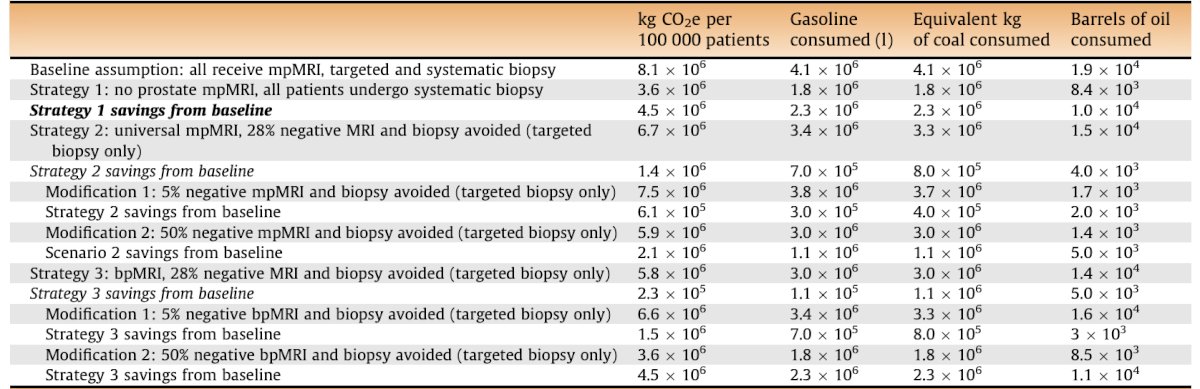
In a recently published article, Ramacciotti et al.3 aimed to assess the carbon footprint, accessibility, and diagnostic performance of an expedited ‘One-Stop’ prostate cancer diagnostic pathway. Among 1,083 consecutive patients undergoing MRI followed by transrectal ultrasound fusion-guided prostate biopsy, patients were divided according to the diagnostic pathway: (i) One-Stop, with MRI and same-day prostate biopsy (3 hours apart), or (ii) Standard, with MRI followed by a second visit for prostate biopsy: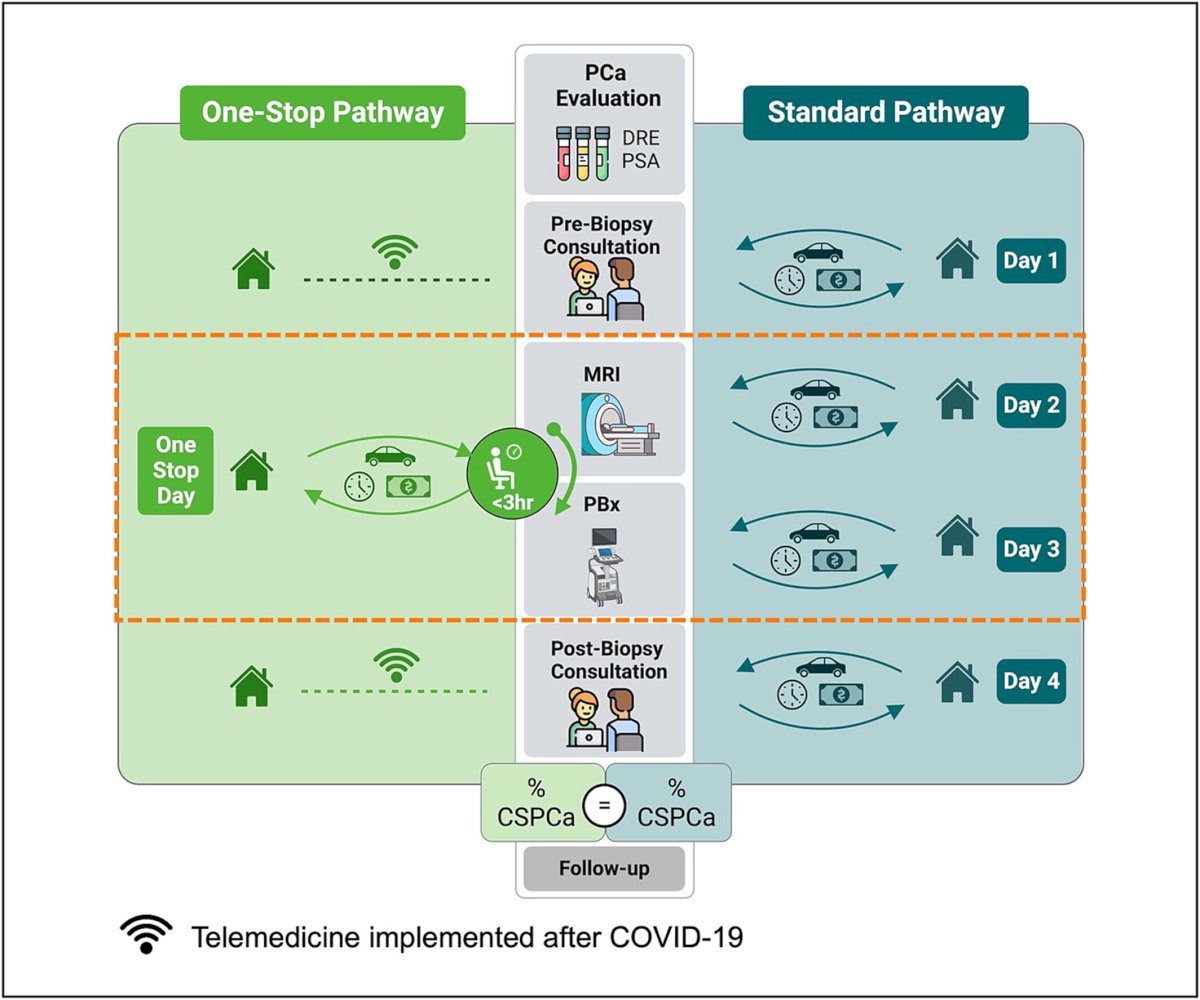
Overall, 260 patients underwent the One-Stop and 823 the Standard pathway. The One-Stop saved 69,575 km in round trips, over 16 tons of travel-related CO2 emissions, and $8,214 U.S. dollars: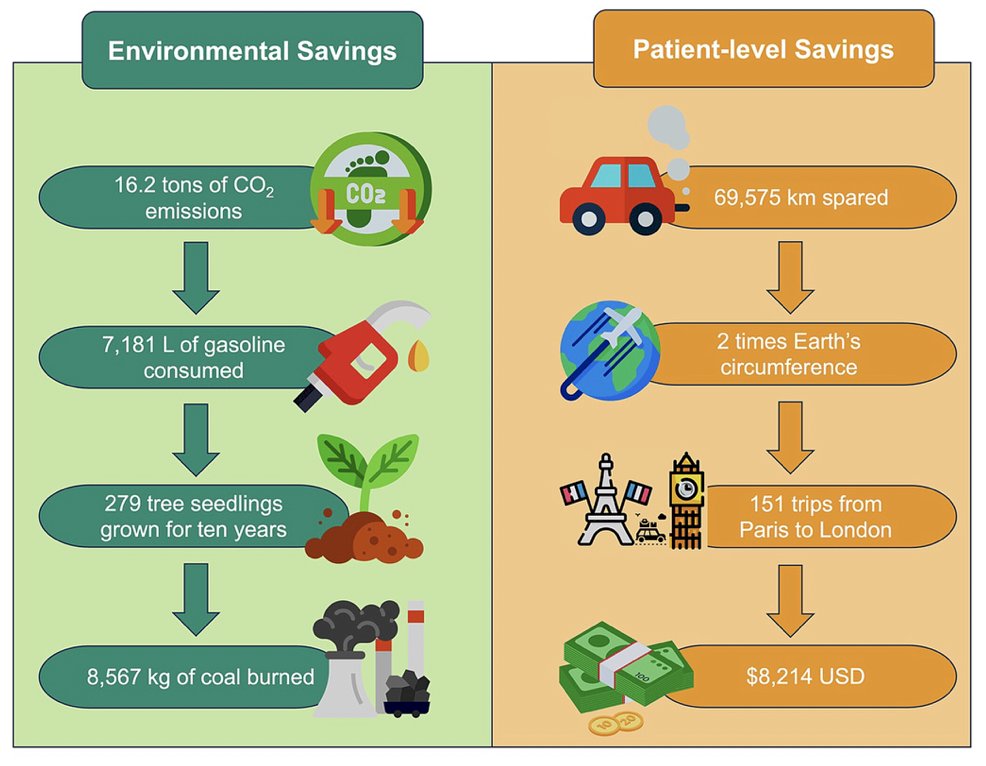
For patients with PIRADS 3–5, the clinically significant prostate cancer detection (53% vs. 50%, p = 0.55) was similar for the One-Stop and Standard pathways, respectively. Dr. Leapman notes that integrating climate-smart actions includes segregation, reducing waste, recycling, reusing, and reducing energy consumption: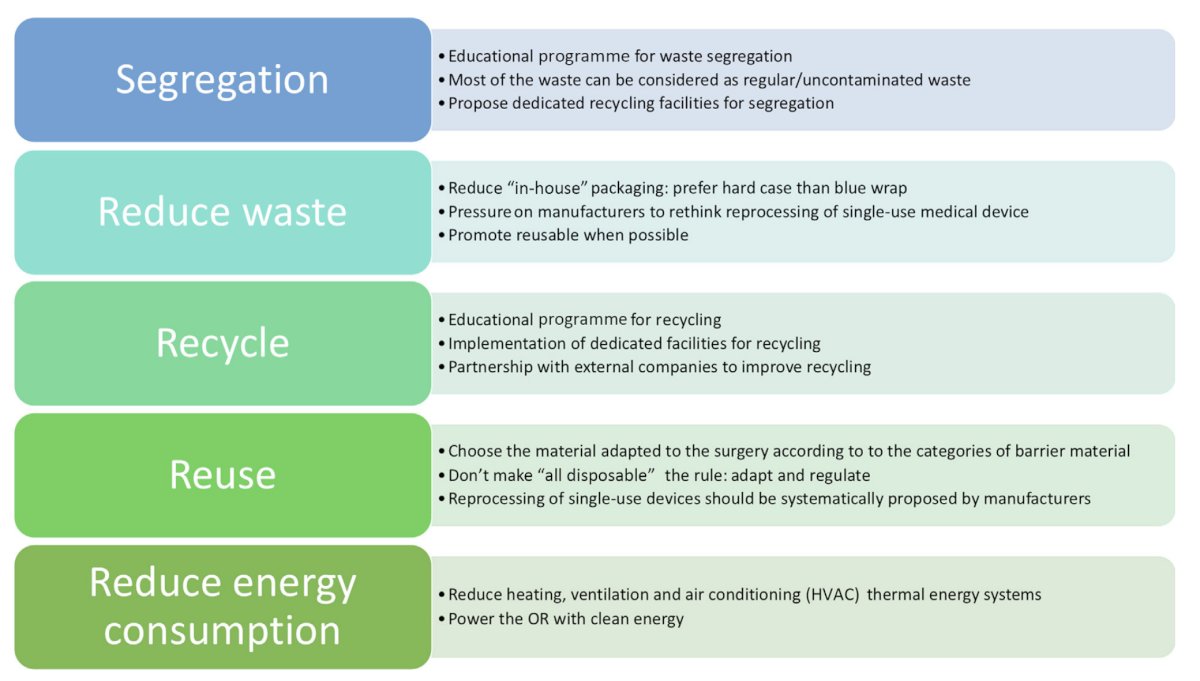
Dietary choices also affect urologic and environmental health. Work from Cole and colleagues4 suggests that we need to recognize the role of diet in disease etiology (prostate, bladder, kidney) and that animal agriculture has a detrimental impact on ecosystems, habitat, fresh water, pollution and global warming. In fact, livestock account for 14.5% of CO2 emissions, including 50% of methane and 60% of NO: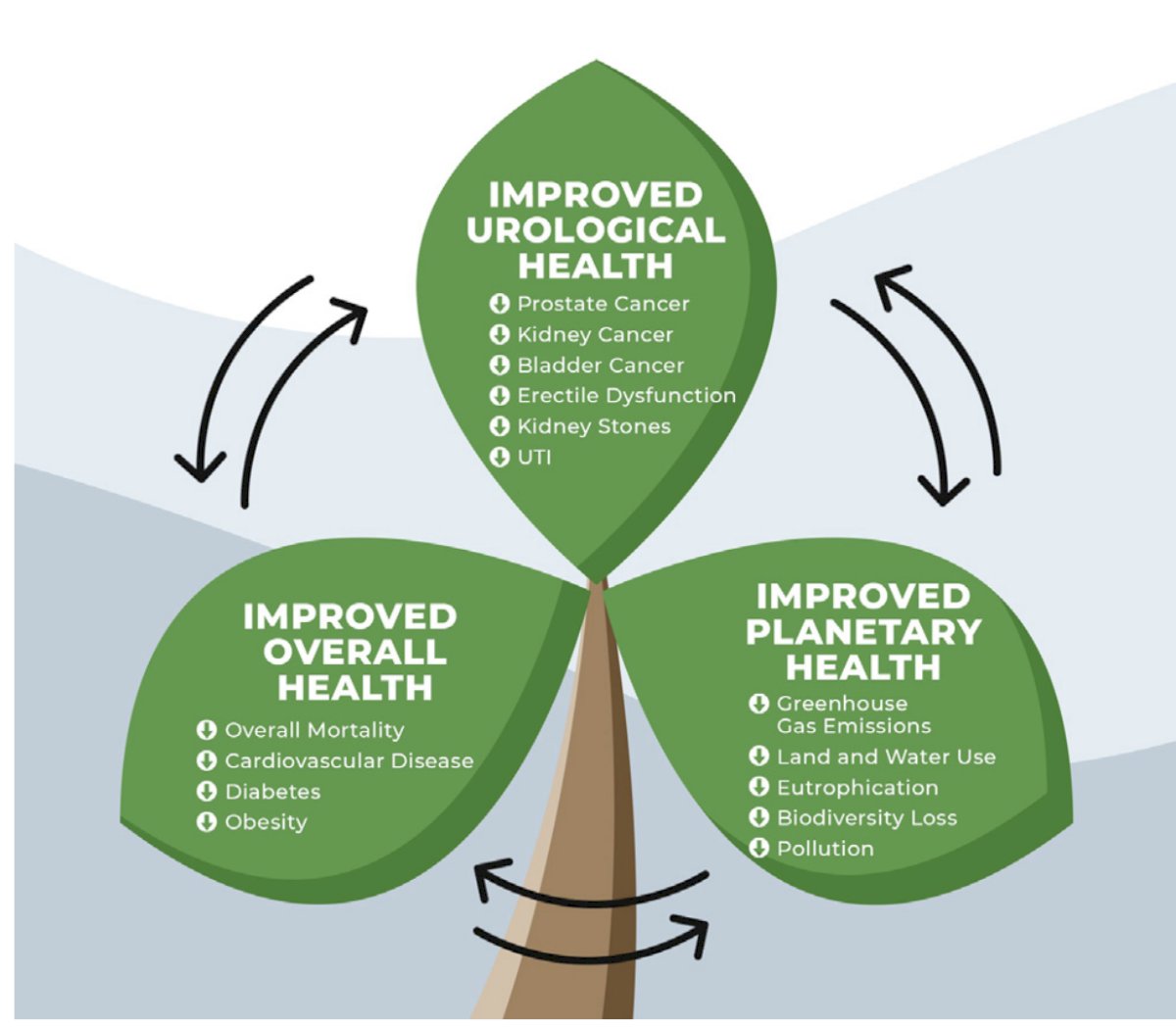
Finally, sustainability does not mean limiting necessary care for our patients. Moreover, the business case for sustainable healthcare is that energy use reduction, waste reduction, efficient OR purchases, and green activities could save $15 billion over 10 years.
Dr. Leapman concluded his presentation discussing sustainability in prostate cancer care with the following take home messages:
- We must recognize health impacts (including urologic cancer) associated with climate change
- We must prioritize high value prostate cancer care
- We must also prioritize sustainability practice, resource conservation, waste reduction, energy efficiency, and de-carbonization
Presented by: Michael Leapman, MD, MHS, Yale University, New Haven, CT
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:
- Trogdon JG, Falchook AD, Basak R, et al. Total Medicare Costs Associated with Diagnosis and Treatment of Prostate Cancer in Elderly Men. JAMA Oncol. 2019 Jan 1;5(1):60-66.
- Leapman MS, Thiel CL, Gordon IO, et al. Environmental impact of prostate magnetic resonance imaging and transrectal ultrasound guided prostate biopsy. Eur Urol. 2023 May;83(5):463-471.
- Ramacciotti LS, Kaneko M, Rodler S, et al. A sustainable and expedited ‘One-Stop’ prostate cancer diagnostic pathway to reduce environmental impact and enhance accessibility. BJU Int. 2024 [Epub ahead of press].
- Cole AP, Gupta N, Loeb S. The Plant-based Prescription: How Dietary Change Can Improve Both Urological and Planetary Health. Eur Urol. 2023 Oct;84(4):357-358.


