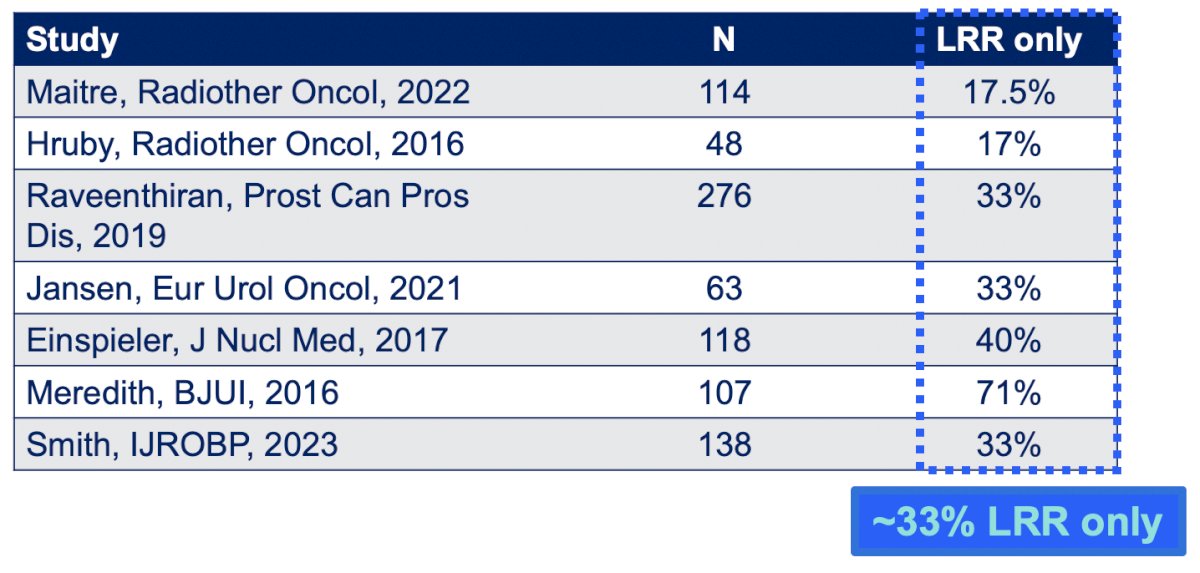
(UroToday.com) The 2024 SUO annual meeting included a prostate cancer session, featuring a debate regarding the management of localized radiorecurrent prostate cancer, and a presentation by Dr. Himanshu Nagar discussing the role of salvage radiotherapy. A solitary loco-regional recurrence on PSMA PET/CT for PSA recurrence is common, seen in 17%-71% of cases after primary radiotherapy:
Importantly, a local recurrence may lead to a “second wave” of metastasis. A systematic review from Kishnan et al.1 of 992 patients for patients undergoing primary radiotherapy for high grade prostate cancer (Gleason Grade 4-5) showed that over a median follow-up of 6.4 years, there was a 24% local failure rate, 37% distant metastasis rate, and 30% prostate cancer specific mortality rate. This study found that the development of local failure was significantly associated with overall survival (HR 1.70), prostate cancer specific survival (HR 3.10), and distant metastasis free survival (HR 1.92):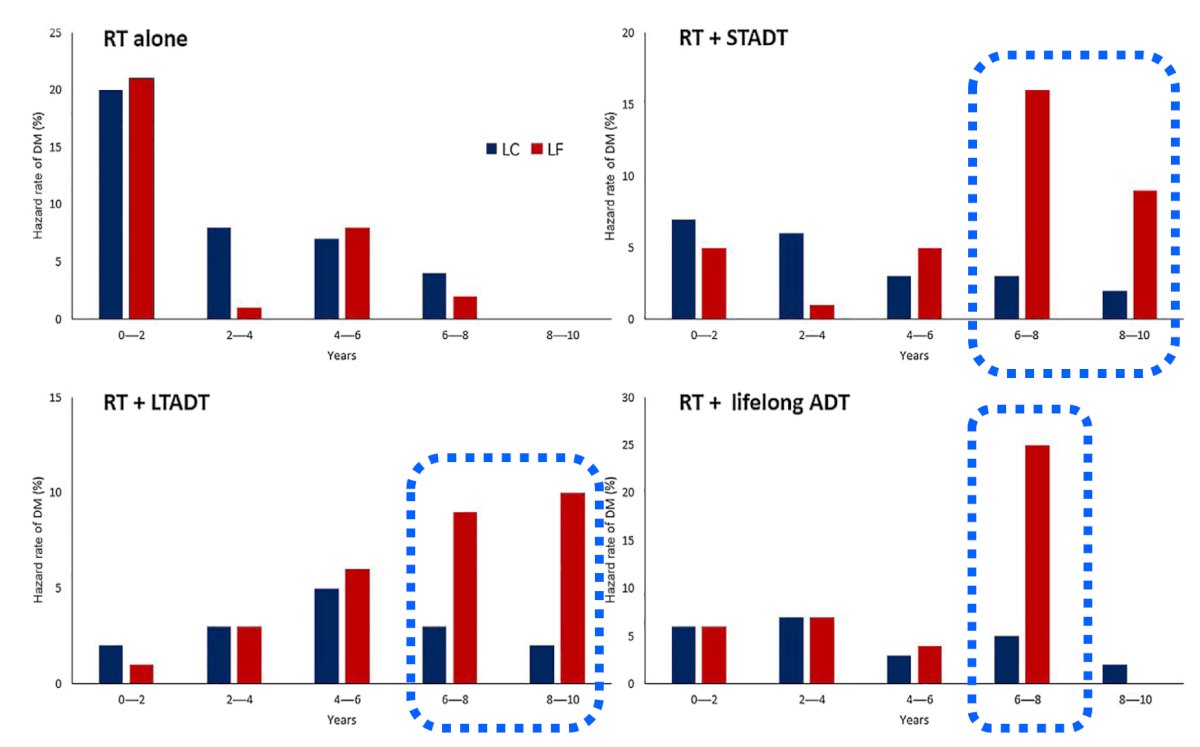
Dr. Nagar emphasized that the integration of PSMA PET/CT and mpMRI in the workup for local recurrence are critical. Additionally, a prostate biopsy is required, since the most common sites of false positive on 68Ga-PSMA-11 PET/CT is the irradiated prostate. Imaging alone does not reveal the true extent of pathologic involvement: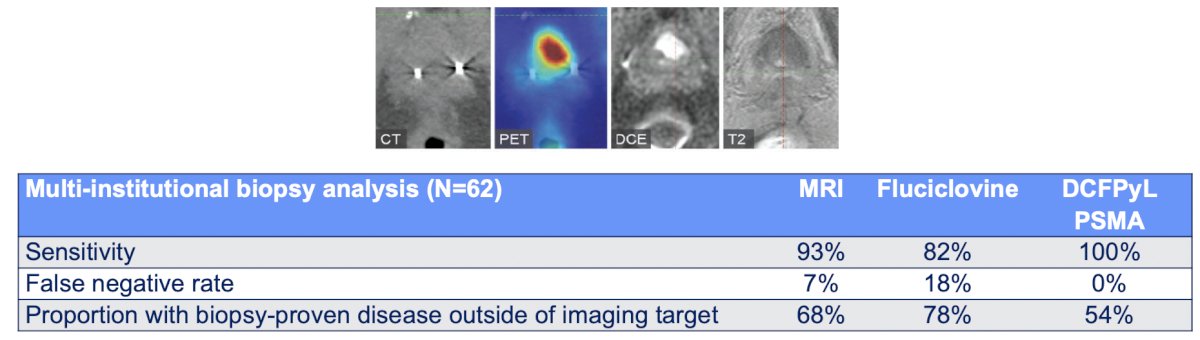
At the 2022 APCCC meeting, when the international panel of experts were queried regarding treatment of EAU low risk failure (interval to biochemical failure > 18 months and Gleason Group 4), the most common salvage therapy selected was salvage radical prostatectomy (38%). For EAU high risk failure (interval to biochemical failure <= 18 months and Gleason 4-5), the most common salvage therapy selected was external beam radiotherapy or brachytherapy: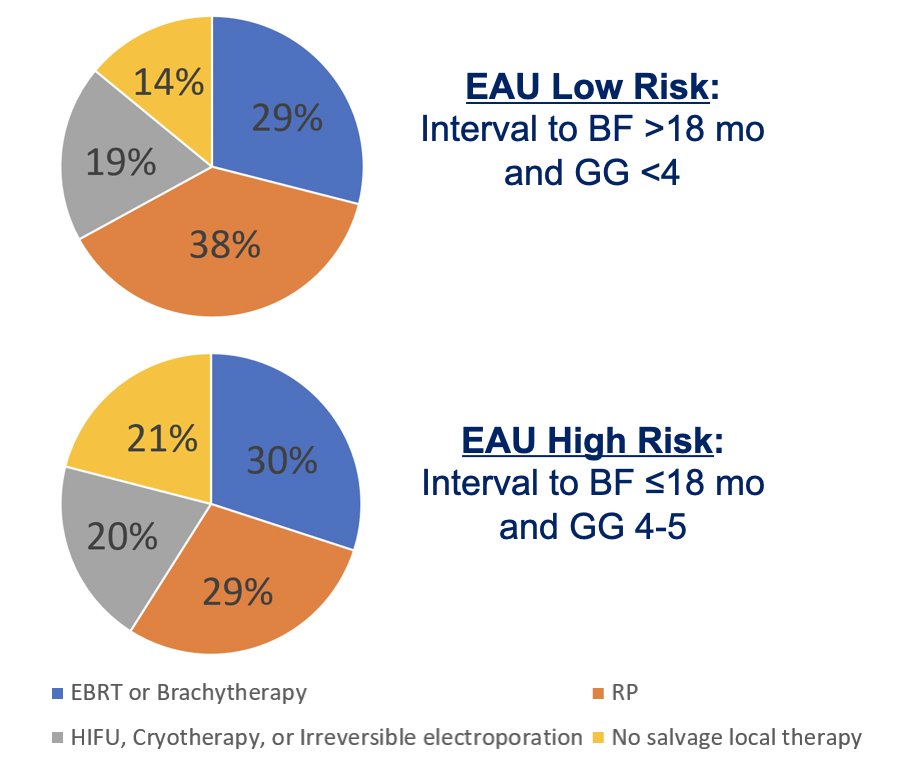
Salvage local therapy has two major attractions for patients:
- Offers an opportunity for a cure
- Alternative to long term palliative systemic therapy
Dr. Nagar then discussed radiation treatment options. Salvage brachytherapy series suggest a 5 year PSA recurrence free survival rate of ~50% and a 5 year metastasis free survival rate of ~75%-90%: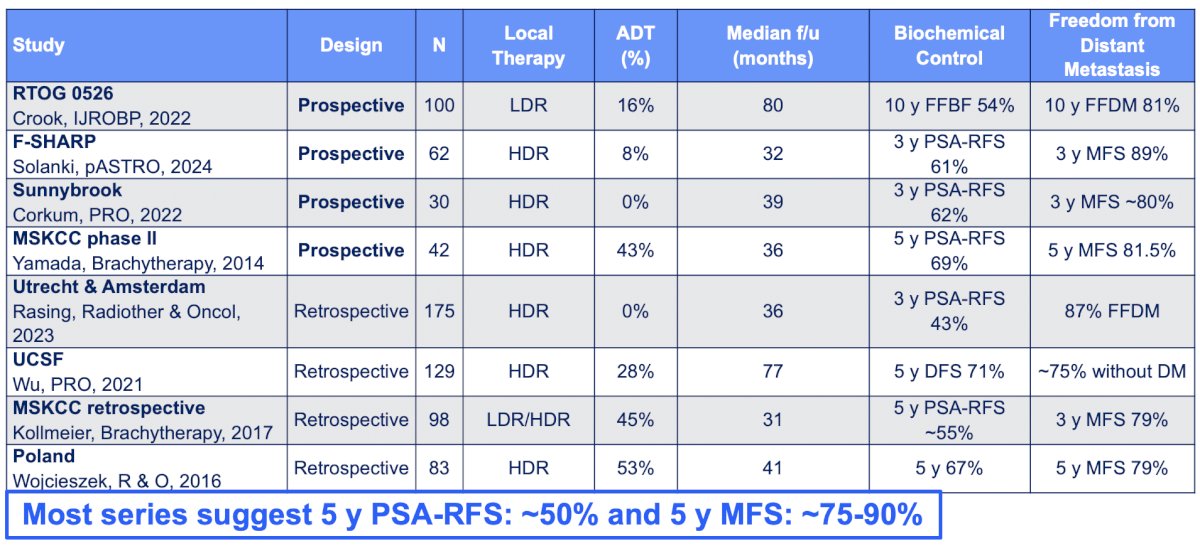
For salvage SBRT, series suggest a 5 year PSA recurrence free survival rate of ~50-80% and a 5 year metastasis free survival rate of ~65%-90%: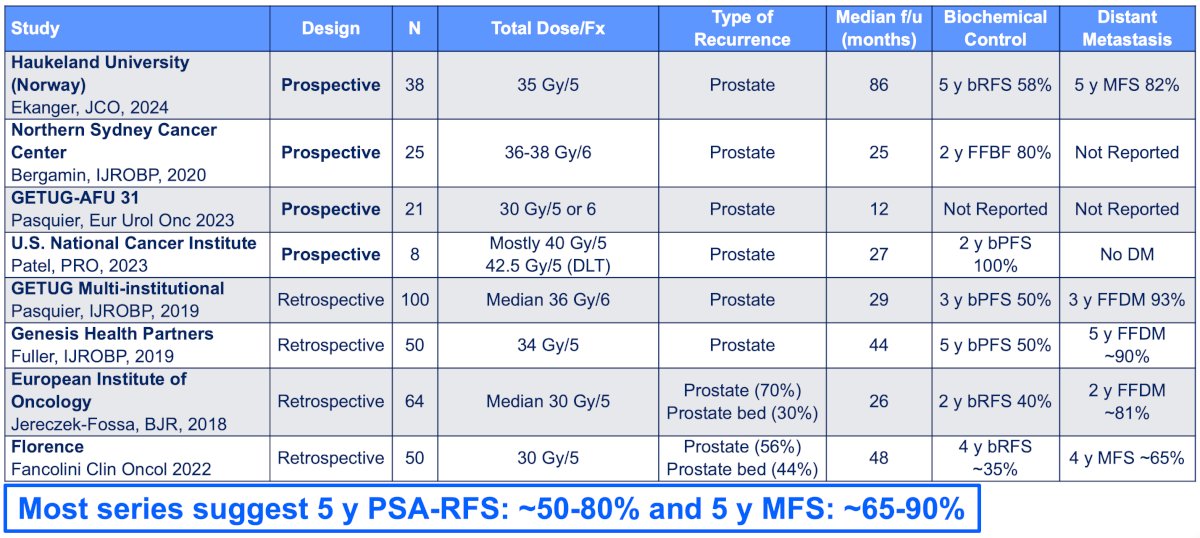
Toxicities for salvage brachytherapy and SBRT include grade 3+ genitourinary toxicity rates of ~5-15% and grade 3+ gastrointestinal toxicity rates of <5%: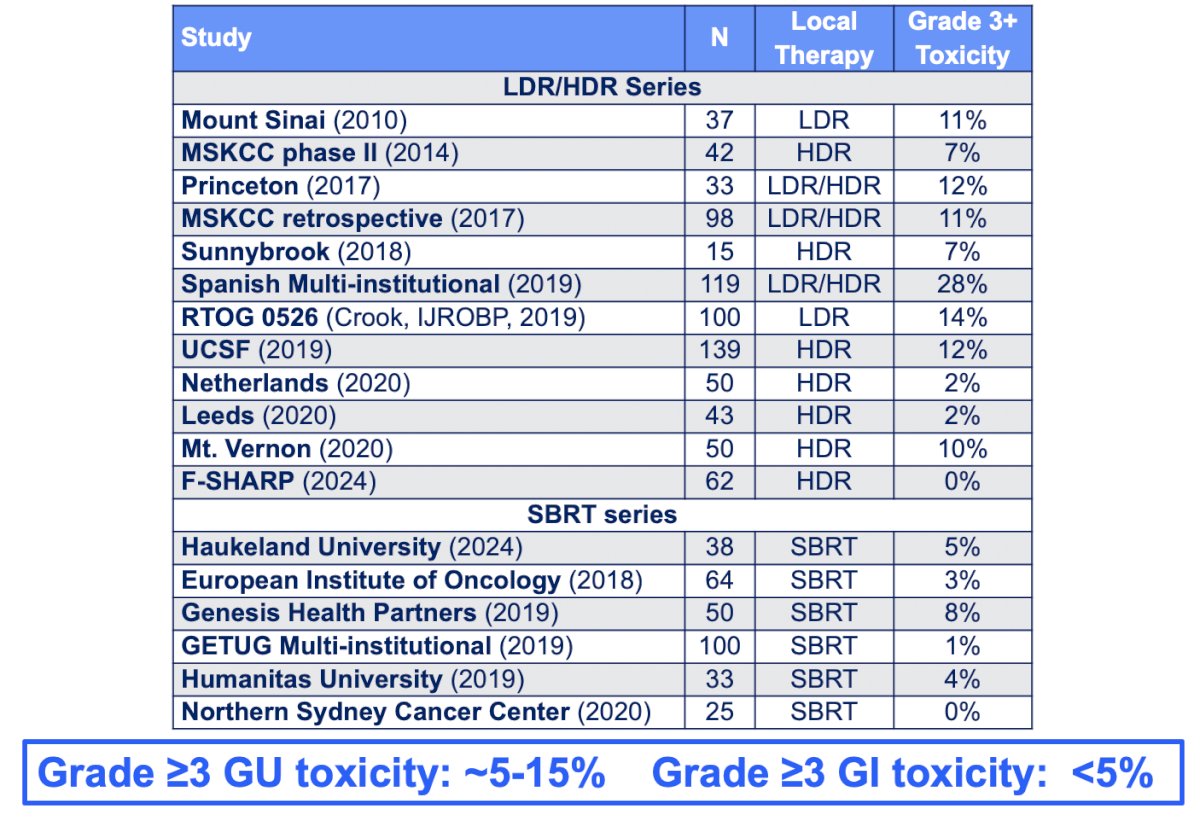
The MASTER study was a 2021 systematic review and meta-analysis of outcomes for local salvage therapy after primary radiotherapy.2 There were 150 studies (28 prospective studies) assessing 11,322 patients. Adjusted 5 year recurrence free survival ranged from ~50% - 60%, reirradiation had lower risk of severe genitourinary toxicity versus radical prostatectomy, and HDR had reduced risk of severe toxicity versus radical prostatectomy:![The MASTER study was a 2021 systematic review and meta-analysis of outcomes for local salvage therapy after primary radiotherapy [2]. There were 150 studies (28 prospective studies) assessing 11,322 patients. Adjusted 5 year recurrence free survival ranged from ~50% - 60%, reirradiation had lower risk of severe genitourinary toxicity versus radical prostatectomy, and HDR had reduced risk of severe toxicity versus radical prostatectomy:](/images/com-doc-importer/184-suo-2024/suo-2024-debate-management-of-localized-radiorecurrent-prostate-cancer-salvage-radiotherapy/image-7.jpg)
One emerging treatment is focal dose-escalated salvage HDR brachytherapy. The F-SHARP trial presented initial result at ASTRO 2024 – this is a multi-institutional phase I/II trial of focal dose-escalated salvage HDR for intraprostatic radio recurrence. Eligibility criteria included a history of localized prostate cancer treated with any form of definitive radiation therapy, and biopsy-proven intraprostatic radio recurrence with no regional or distant metastasis. All patients had a PET/CT. The primary objective was to determine the acute radiation therapy-related grade 3+ CTCAE v4.03 genitourinary and gastrointestinal toxicity rates. Secondary endpoints included all-grade acute and late toxicity, quality of life (IPSS and EPIC-26), and biochemical/radiographic disease control and survival measures. From 2017-2023, there were 62 patients enrolled at three sites (Loyola University, University of Virginia, and UT Southwestern). The 2-stage phase I/II study schema is as follows: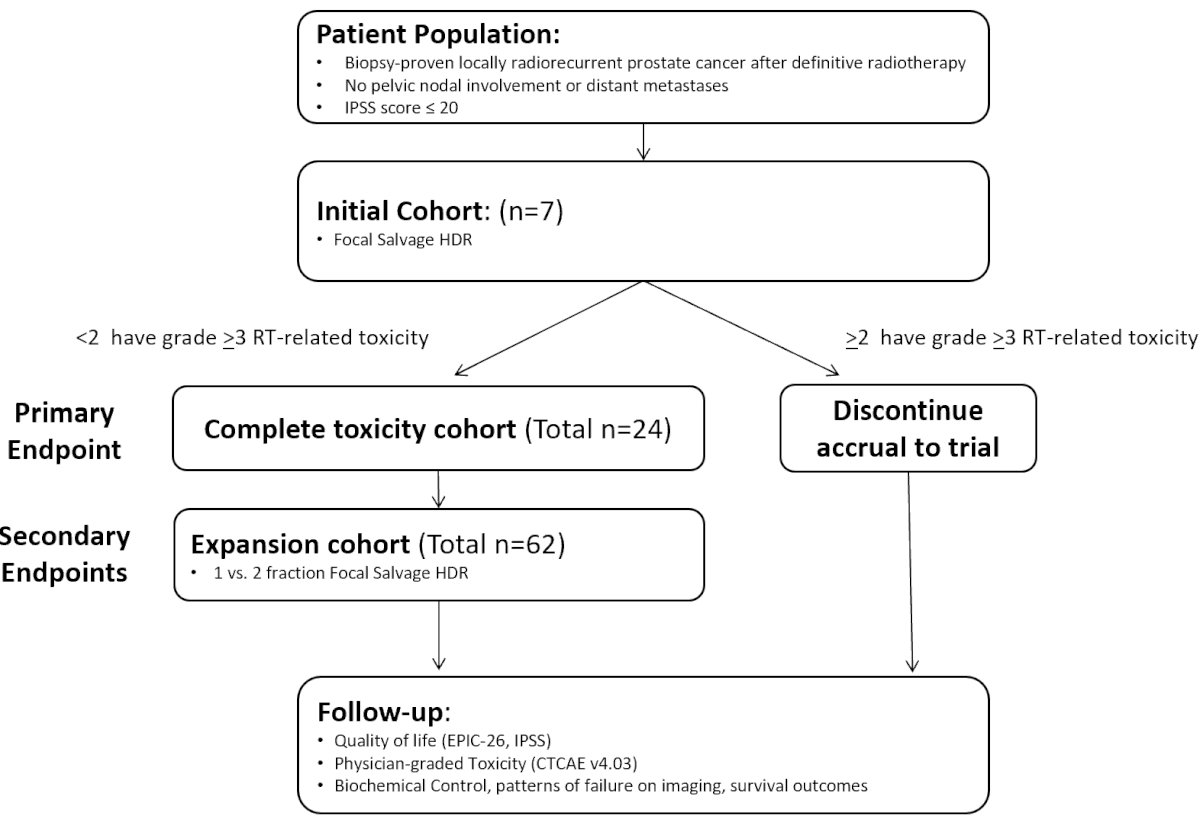
Over a median follow-up of 32.3 months, there were no grade >=3 acute or late toxicities. Acute/late grade 2 genitourinary toxicity occurred in 52%/33%, acute/late grade 2 gastrointestinal toxicity occurred in 1.4%/0.3%, and acute/late grade 2 sexual toxicity occurred in 22%/24%. The 3-year biochemical progression-free survival was 61%, radiographic progression-free survival was 67%, locoregional recurrence-free survival was 73%, metastasis-free survival was 89%, and freedom from ADT was 93%
The RO-PIP trial is randomizing men with radiorecurrent prostate cancer to SBRT versus HDR brachytherapy, with a primary outcome of feasibility of recruitment: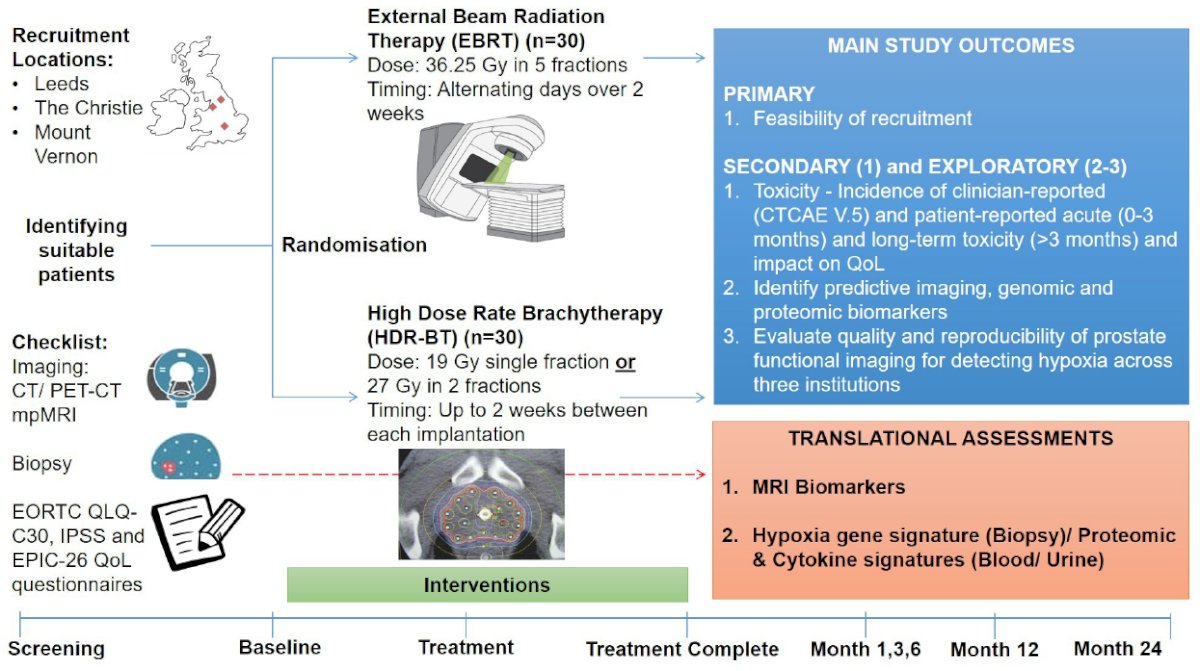
Dr. Nagar concluded his presentation discussing the role of salvage radiotherapy with the following take home messages:
- Local radio-recurrence is an increasingly identified disease state
- PSMA PET, MRI, and biopsy are critical
- There is no standard of care management approach
- Salvage brachytherapy and SBRT are effective and safe
Presented by: Himanshu Nagar, MD, MS, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:
- Kishan AU, Chu FI, King CR, et al Local failure and survival after definitive radiotherapy for aggressive prostate cancer: An individual patient-level meta-analysis of six randomized trials. Eur Urol. 2020 Feb;77(2):201-208.
- Valle LF, Lehrer EJ, Markovic D, et al. A systematic review and meta-analysis of local salvage therapies after radiotherapy for prostate cancer (MASTER). Eur Urol. 2021 Sep;80(3):280-292.


