(UroToday.com) The 2024 SUO annual meeting included a prostate cancer session, featuring a debate regarding the management of localized radiorecurrent prostate cancer, and a presentation by Dr. Behfar Ehdaie discussing the role of salvage radical prostatectomy.
A recurrence after primary radiation is defined by the ASTRO criteria as: (i) a PSA nadir + 2 ng/mL (Phoenix definition) or (ii) 3 consecutive rises in PSA measurement. However, there are limitations, including PSA bounce (occurs in 15% of cases), potentially early disease recurrence, and we should biopsy all patients to define local recurrence, but should wait at least 24 months after primary prostate radiotherapy.
Post radiotherapy recurrence, an MRI prostate should be performed with contrast, and the prostate biopsy should be systematic + targeted biopsies and include the seminal vesicles. Importantly, Dr. Ehdaie states that a focused effort should also be made to biopsy medial tissue adjacent to the urethra as this is a sanctuary site of recurrent disease. Of note, prostate adenocarcinoma with “treatment effect” is not disease recurrence: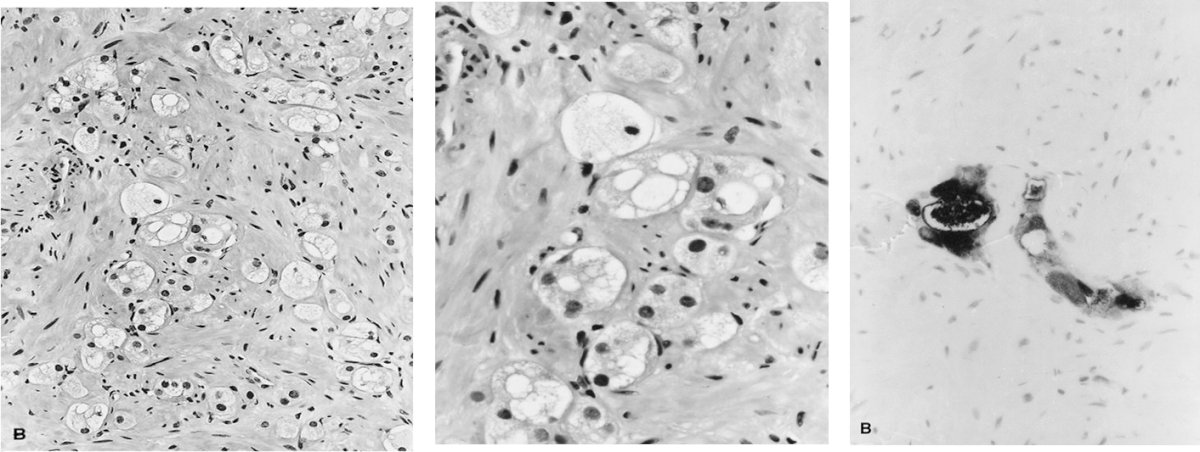
Despite advancements in MRI, defining a focal local recurrence is challenging. In 2021, Dr. Ehdaie and colleagues assessed 77 patients that underwent salvage radical prostatectomy with preoperative MRI, systematic/targeted biopsy, and post surgery tumor maps.1 The primary outcome was the ability of clinicopathologic and imaging criteria to identify patients who may be eligible for salvage partial gland ablation based on detailed tumor map from whole-mount salvage radical prostatectomy slides. Of these 77 patients, 15 patients (19%) were determined to be eligible for salvage partial gland ablation based on biopsy-proven unilateral disease in contiguous sextant segments, a dominant lesion on MRI concordant with biopsy location or no focal region of interest, and no imaging evidence of extraprostatic disease: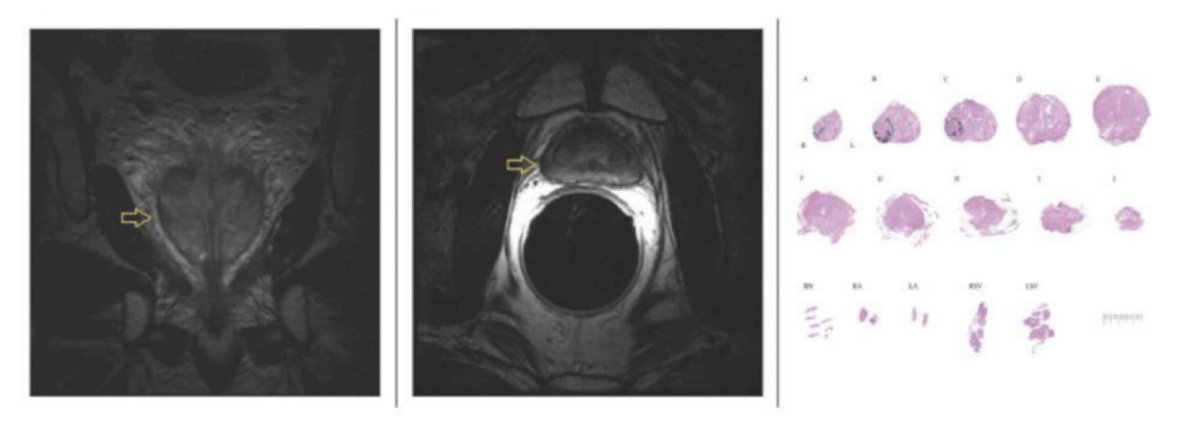
Undoubtedly, a salvage radical prostatectomy carries certain risks. Dr. Ehdaie notes that based on work from Fridriksson et al.2 the risk of procedures associated with the urinary tract or gastrointestinal complications is increased after radiotherapy up to 12 years after treatment: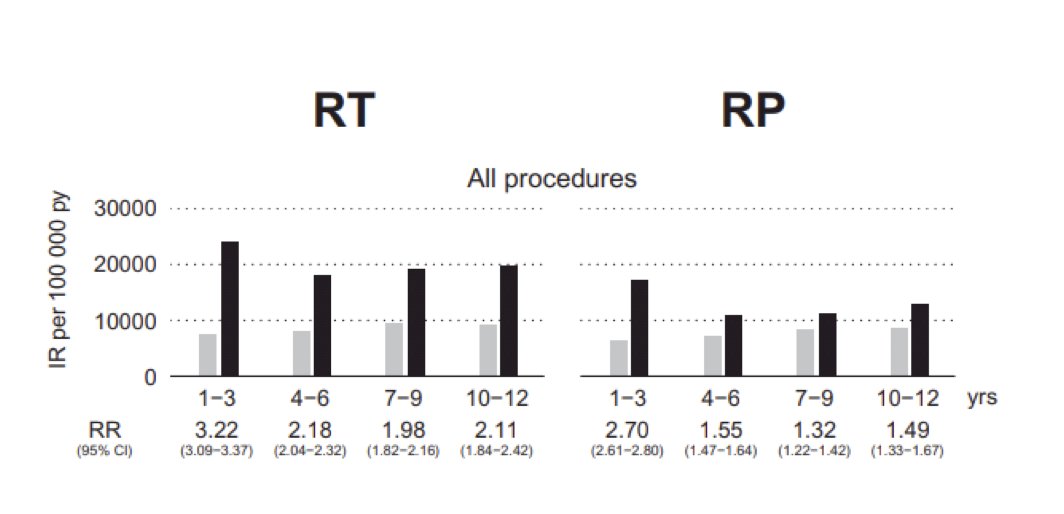
To assess cancer control and functional outcomes of salvage radical prostatectomy, in 2012 Chade and colleagues3 performed a systematic review of the literature, identifying 40 studies and 404 patients. Biochemical recurrence-free probability after salvage radical prostatectomy ranged from 47% to 82% at 5 years and from 28% to 53% at 10 years. Complications for salvage radical prostatectomy are generally as follows:
- Rectal injury: 2%
- Anastomotic leak: 20%
- Bladder neck contracture: 10%
- Severe urinary incontinence: 25%
Dr. Ehdaie concluded his presentation discussing the role of salvage RALP with the following surgical technique pearls:
- Sharp dissection is important
- Use a posterior approach to the seminal vesicles
- Beware of the apical dissection
- Preserve the endopelvic fascia
- Use monocryl, interrupted sutures on the vesicourethral anastomosis to decrease the risk of vascular compromise
Post-operatively, Dr. Ehdaie mentioned that he leaves a Foley catheter for 2 weeks and performs a cystogram on all patients prior to Foley catheter removal to ensure the anastomosis is adequately healed.
Presented by: Behfar Ehdaie, MD, MPH, Memorial Sloan Kettering Cancer Center, New York, NY
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Society of Urologic Oncology (SUO) Annual Meeting, Dallas, TX, Tues, Dec 3 – Fri, Dec 6, 2024.
References:
- Chesnut GT, Tin AL, Sivaraman A, et al. Defining the index lesion for potential salvage partial or hemi-gland ablation after radiation therapy for localized prostate cancer. Urol Oncol. 2021 Aug;39(8):495.e17-495.e24.
- Fridriksson JO, Folkvaljon Y, Nilsson P, et al. Long-term adverse effects after curative radiotherapy and radical prostatectomy: Population-based nationwide register study. Scand J Urol. 2016 Oct;50(5):338-345.
- Chade DC, Eastham J, Graefen M, et al. Cancer control and functional outcomes of salvage radical prostatectomy for radiation-recurrent prostate cancer: A systematic review of the literature. Eur Urol. 2012 May;61(5):961-971.


