(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between December 3 and December 6, 2024, was host to the Testis Cancer Session. Dr. Katherine McGlynn discussed the Updates to Testicular Cancer Epidemiology.
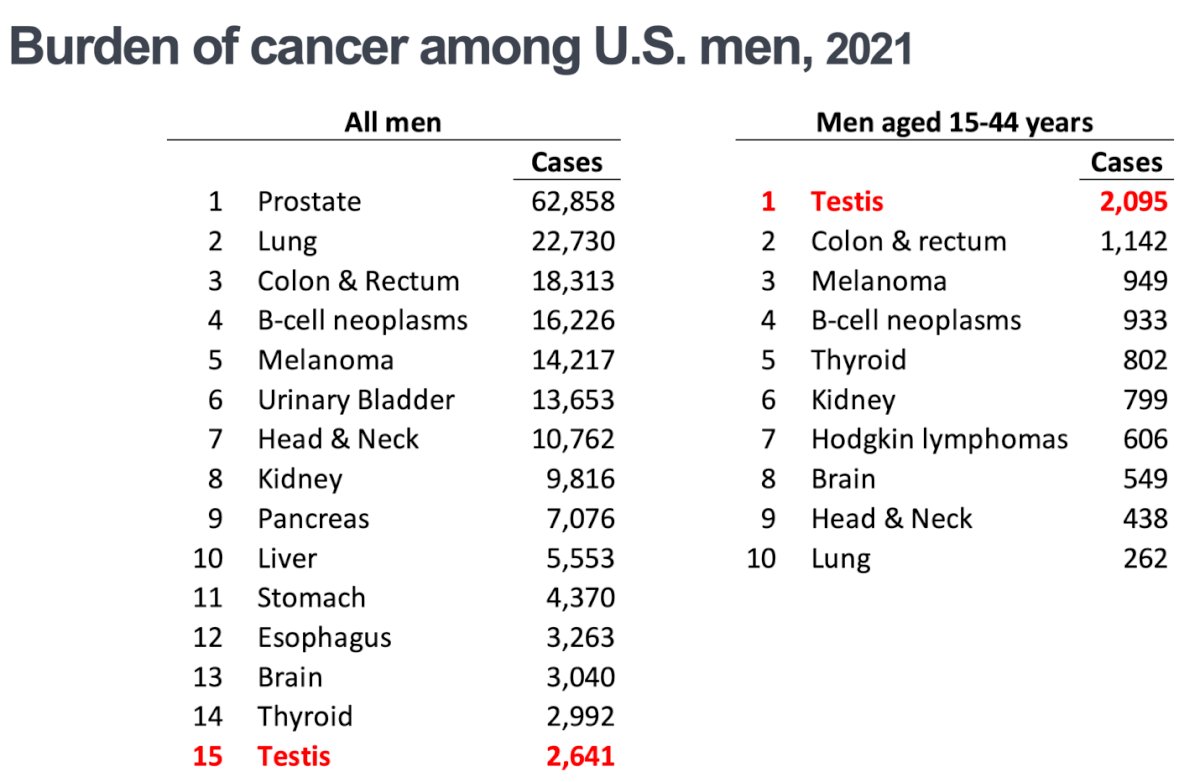
Dr. McGlynn began her presentation by highlighting the statistics of testicular cancer in the U.S. She noted that it was the 15th most diagnosed cancer among men, with 2,641 cases reported in 2021. However, when focusing specifically on men aged 15 to 44 years, testicular cancer was the most frequently diagnosed cancer, with approximately 2,095 cases in this age group according to data from the Surveillance, Epidemiology, and End Results (SEER) Program on Cancer Statistics.1
In terms of histology, seminoma was the most commonly diagnosed histology, comprising 54% of the cases. This was followed by nonseminomatous germ cell tumors (NSGCT) in 42% of cases, and non-germ cell tumors in 3% of cases, as shown in the data below.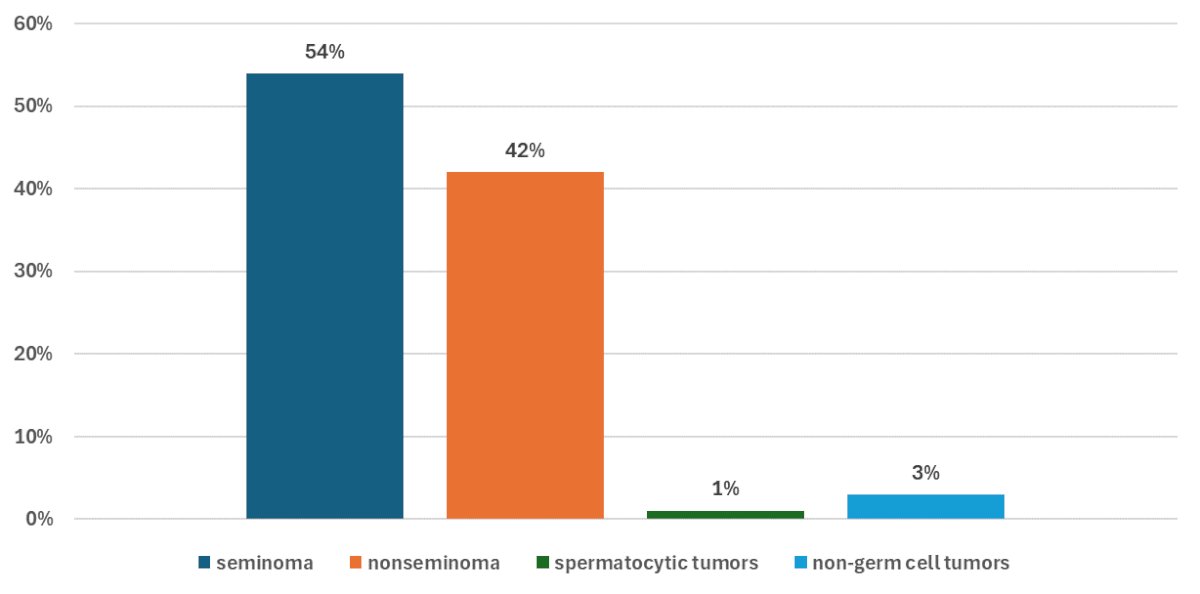
Regarding the age at diagnosis for testicular germ cell tumors among U.S. men, Dr. McGlynn noted the following: seminoma peak incidence occurred in the 35–39-year-old group, with over 8 cases per 100,000 person-years. On the other hand, NSGCTs were more commonly diagnosed in the 25-29 age group, with over 7 cases per 100,000 person-years.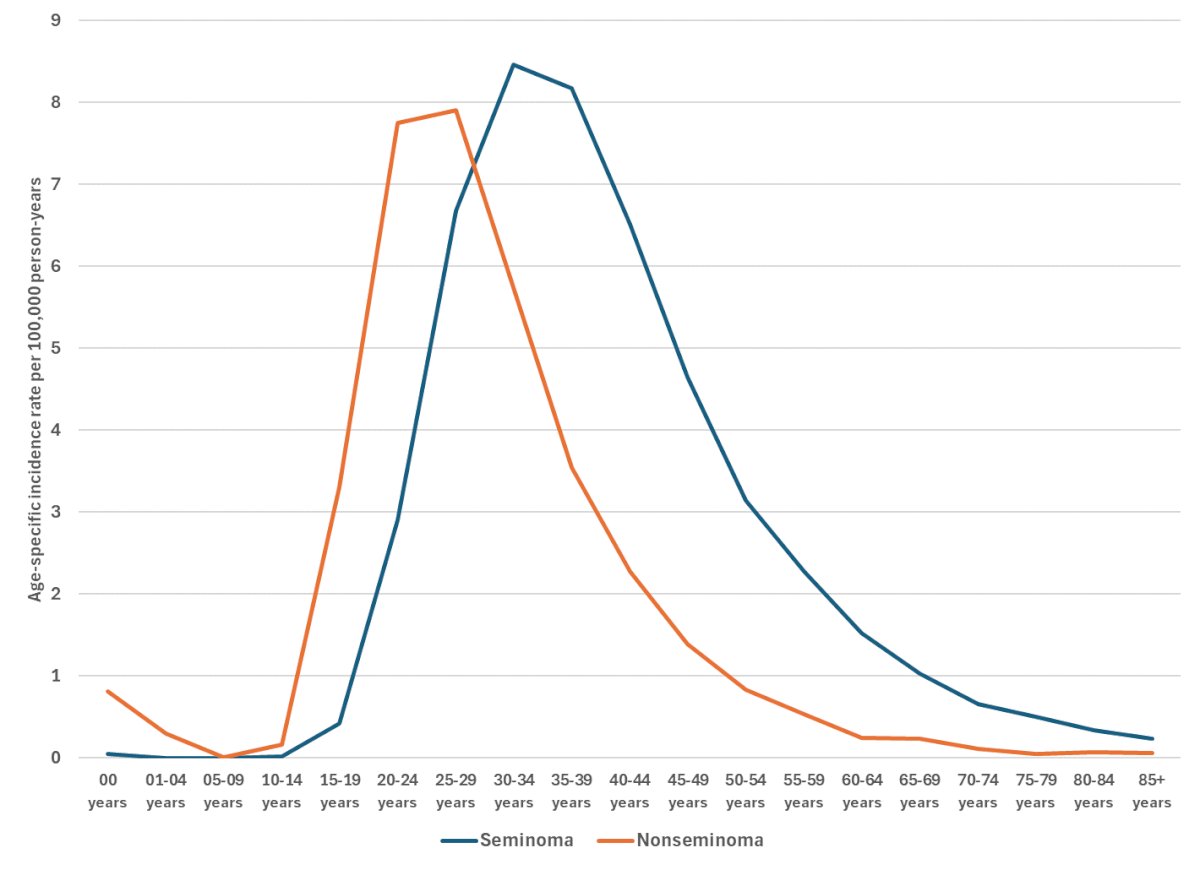
Notably, the incidence of both seminoma and NSGCT decreased significantly with age. Interestingly, for patients diagnosed with spermatocytic tumors, the incidence slightly increased in those over 50 years old.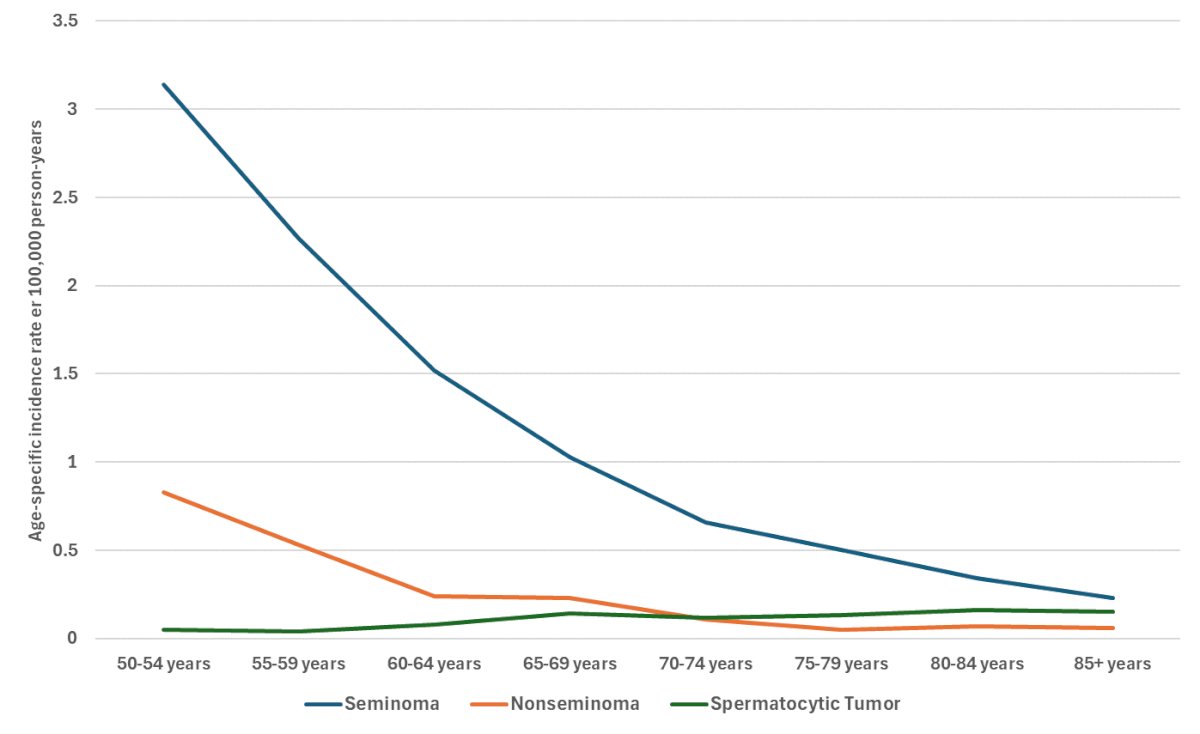
Dr. McGlynn provided a summary of where the data reporting the trends of testicular germ cell tumors (TGCT) in the U.S. is coming from which is of great interest to epidemiologists, noting that the primary source of this data is the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. SEER-12 collects data from 12 cancer registries, with incidence data spanning nearly 30 years from 1992 to 2021, and survival data covering 26 years from 1992 to 2017.
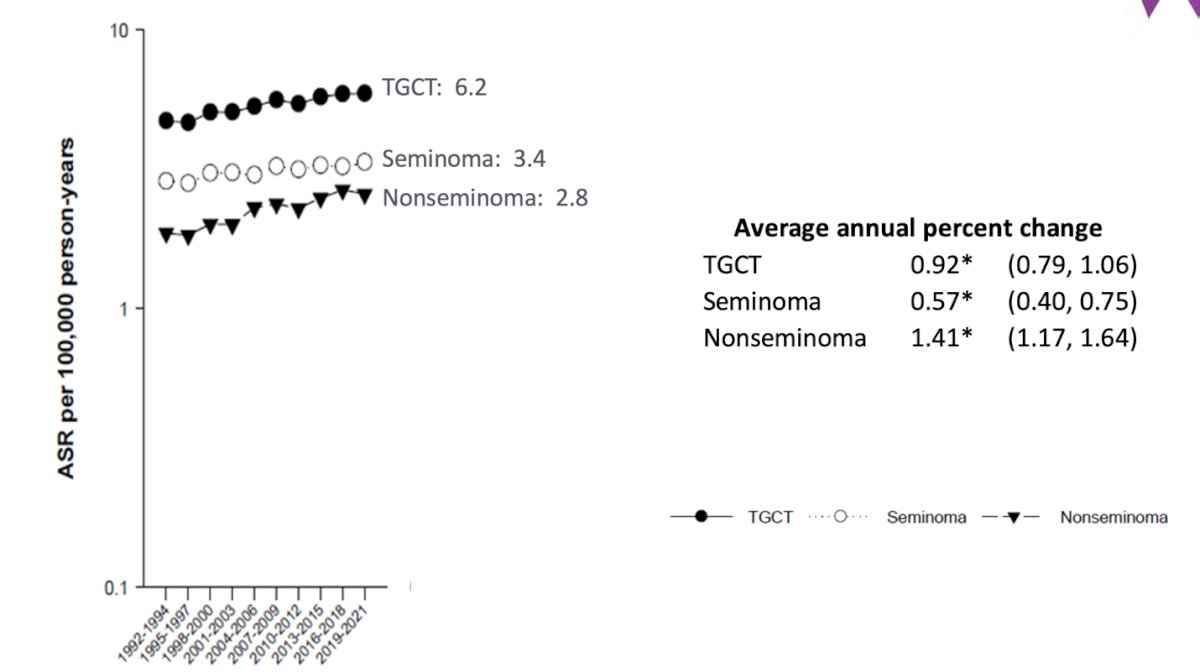
The adjusted standardized ratio (ASR) for TGCTs has been steadily increasing over the past century. The current ASR stands at 6.2 per 100,000 person-years for TGCTs, with 3.4 for seminoma and 2.8 for NSGCTs. Interestingly, the data shows an average annual percent change of 0.92 (95%CI 0.79-1.06) for TGCTs.
However, the real interest of this analysis was to look incidence rates of testicular germ cell tumors (TGCTs) by race and ethnicity. The incidence of TGCT among non-Hispanic White men seem to be plateauing, with an adjusted standardized ratio (ASR) of 7.2 per 100,000 person-years in 2021. Interestingly, the incidence rates among Hispanic men have increased to levels comparable to those of non-Hispanic White men, reaching an ASR of 7.6 per 100,000 person-years. Incidence rates among non-Hispanic Black men have remained low (ASR 1.0).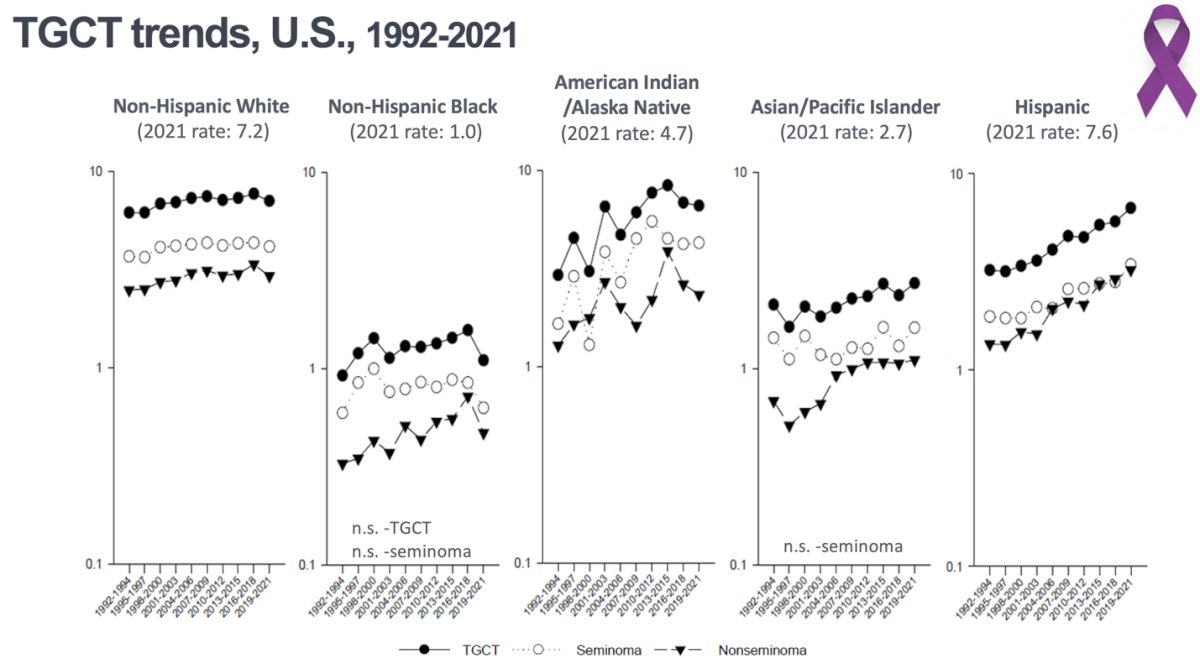
Dr. McGlynn discussed another analysis was to evaluate risk at birth cohort and age at diagnosis. The average age of diagnosis is 33 years in the overall population. Among Hispanic men, who are diagnosed the youngest, the average age is 29 years, while non-Hispanic Black men are diagnosed at an average age of 37 years. Furthermore, patients diagnosed with seminoma tend to be older, with an average age of 36 years, compared to 29 years for those diagnosed with NSGCTs. Dr. McGlynn mentioned that this probably doesn’t mean a lot biologically but is important to know that these patients all have a very different ages of diagnosis depending on the ethnicity/race.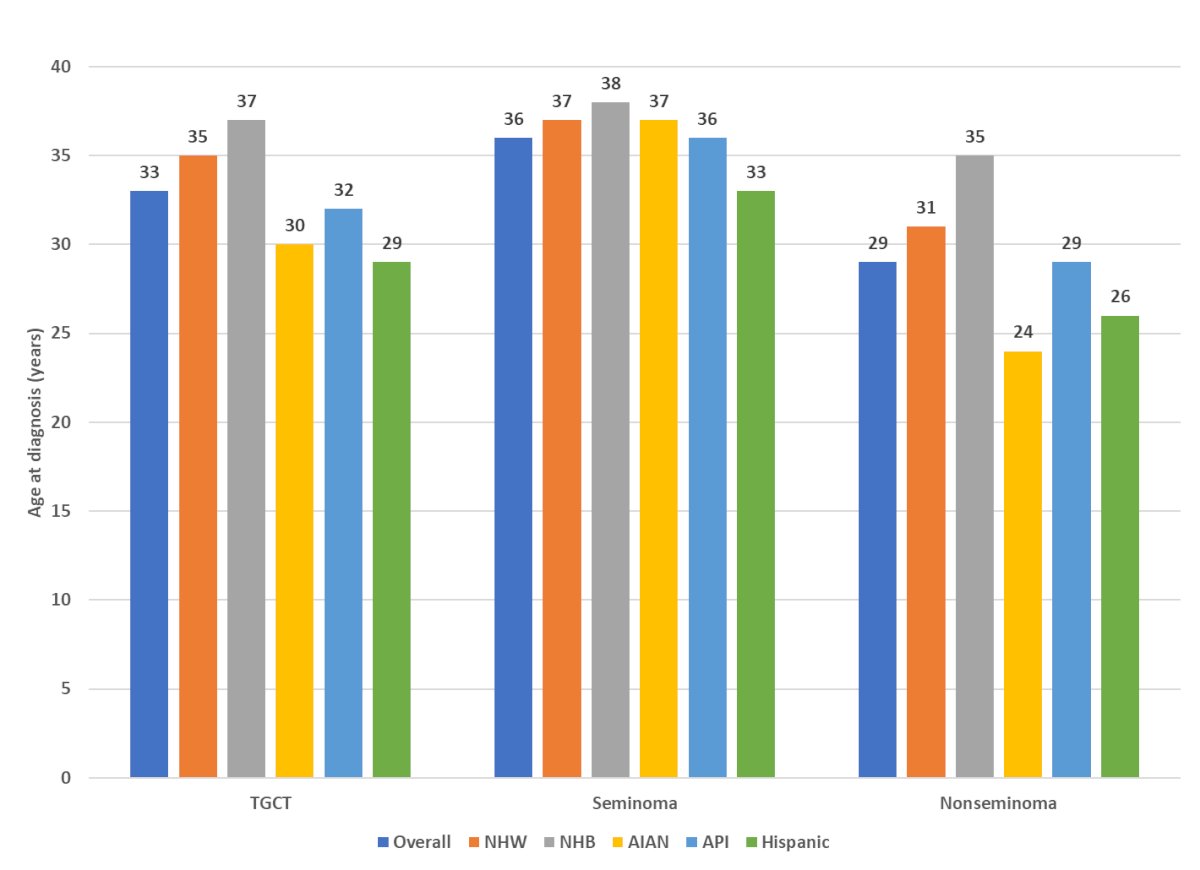
They looked at stage at diagnosis and reported that in all racial and ethnic groups, patients are more commonly diagnosed with localized TGCTs. However, there are notable disparities in the diagnosis of distant metastatic disease. Non-Hispanic Whites are diagnosed with distant metastatic disease in about 9% of cases. In contrast, other racial and ethnic groups, including Hispanics, non-Hispanic Blacks, and others, are diagnosed with distant metastatic disease in 12-18% of cases. This rate almost doubles that of the non-Hispanic White population, indicating significant disparities in the stage at diagnosis among different racial and ethnic groups.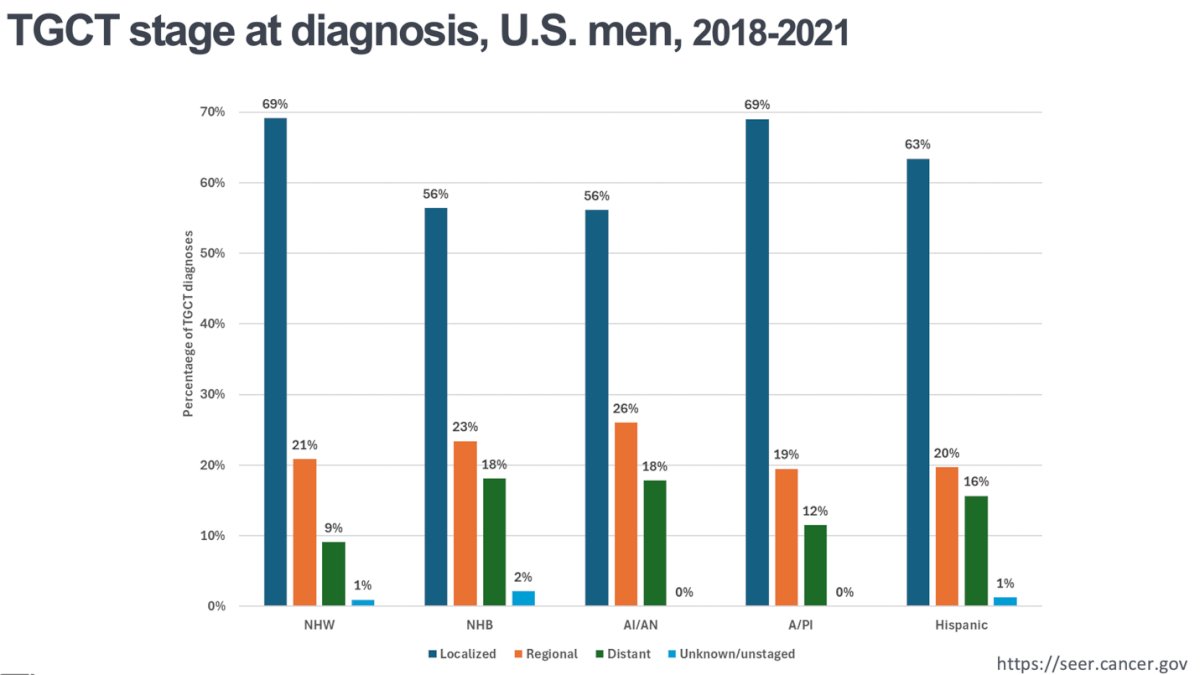
The 5-year survival rate for TGCTs is very favorable for the overall population and similar across different racial and ethnic groups, with 95.8% of patients alive in the overall population. However, disparities exist, as non-Hispanic Black patients have the worst survival rates both overall and for specific types of TGCTs: 92.7% for seminoma and 80.1% NSGCTs.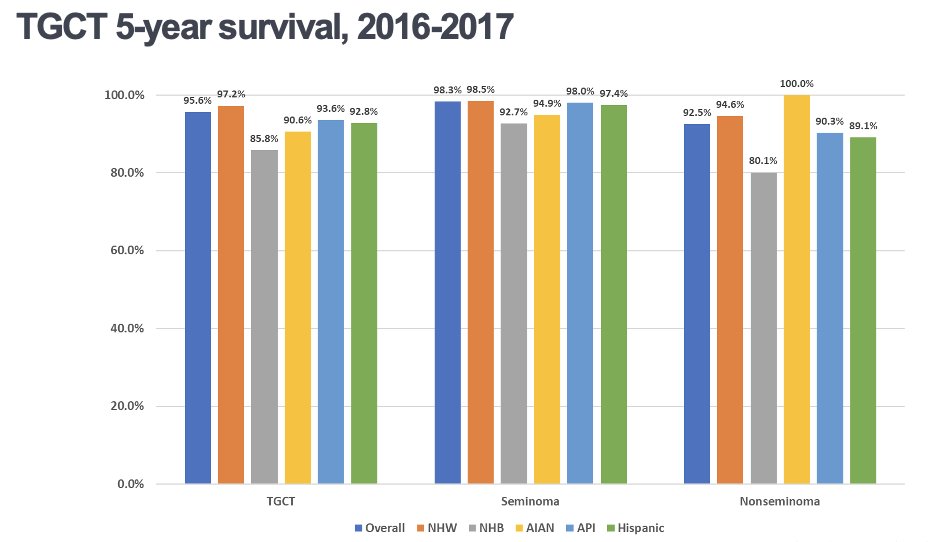
Dr. McGlynn highlighted that they looked at rates of testicular cancer incidence in Central America and Mexico, considering this are the highest number of immigrants into the US. They found their incidence of testicular cancer is much lower compared to data from the SEER program in the U.S. However, she noted that this discrepancy could be due to under registration of testicular cancer cases in these regions which could end up skewing the apparent incidence rates.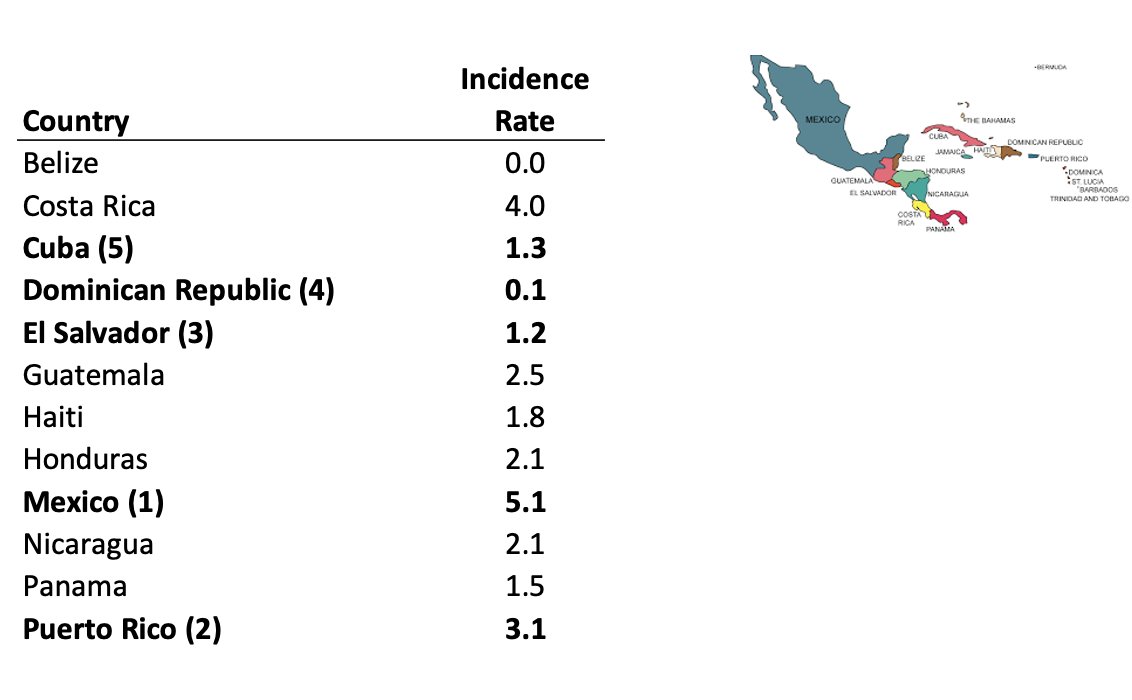
Risk factors for TGCT remain poorly understood. However, certain factors are likely to be associated with an increased risk of TGCT, including firefighting, aircraft maintenance, marijuana use, and exposure to some organochlorine compounds. Nonetheless, further research is needed to confirm these associations. Factors that are unlikely to be associated with TGCT, and which require additional study, are indicated in the following section. One of the factors that needs additional study and further research is the Per-and polyfluoroalkyl substances (PFAS) which are components of firefighting foams used at military installations.

Dr. McGlynn concluded her presentation with the following take home messages:
- TGCT rates among non-Hispanic White men appear to be plateauing.
- TGCT rates among Hispanic men have increased to level of rates among non-Hispanic White men.
- Rates among non-Hispanic Black men have remained low, but they are diagnosed at later stages and have lower survival rates.
- Risk factors for TGCT remain poorly understood.
Presented by: Katherine McGlynn, PhD, MPH, Senior Investigator, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NCI, United States.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:- Surveillance, epidemiology, and end results program. SEER. (n.d.). https://seer.cancer.gov/


