(UroToday.com) The 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, TX was host to the Testis Cancer Session. Dr. Samuel Funt discussed How to Avoid Inappropriate Chemotherapy Administration for Testicular Cancer in case-based presentation.
Dr. Funt began his presentation by emphasizing the importance of administering appropriate chemotherapy to patients with testicular cancer who truly need it. He highlighted the potential risks associated with chemotherapy, such as the increased likelihood of developing other cancers and the heightened risk of cardiovascular disease, particularly in a young population that has a long-term survival outlook. His presentation was organized into seven clinical cases, each designed to illustrate how to identify metastatic masqueraders in these scenarios.
Case # 1- A 37-year-old man who was found to have seminoma of the right testis.
- Tumor markers were normal.
- Images from his initial staging scans revealed a 10 x 7mm retroperitoneal lymph node and multiple pulmonary nodules.
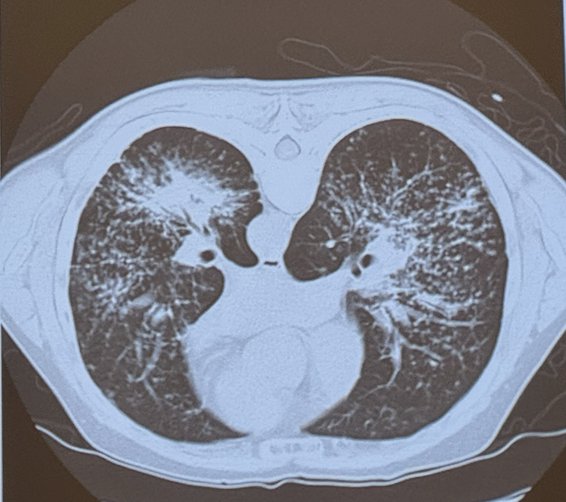
Masquerader #1: Sarcoidosis
There is approximately a 100-fold increase in sarcoidosis among patients with testicular cancer compared to the general population. Testicular carcinoma has the strongest association with sarcoidosis among solid tumors. Sarcoidosis may occur before or after the diagnosis of testicular cancer, necessitating a biopsy for accurate diagnosis. The differential diagnosis includes bleomycin toxicity, which can present similarly. Dr. Funt highlighted that solid lung relapses in seminoma are extremely rare.
Case # 2- 30-year-old man who was found to have seminoma of the left testis.
- Tumor markers were normal.
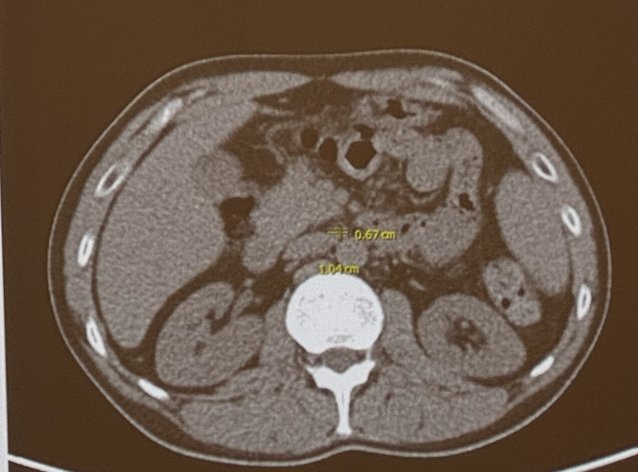
- Images from his initial staging scan showed a 1.2 cm left para-aortic lymph node just inferior to the left renal hilum.
Follow-up CT scan 2 months later showed markedly decrease in size of the questionable lymph node as shown below:
Masquerader #2: Benign Retroperitoneal Lymph Nodes
Dr. Funt emphasized that short-interval imaging is safe in certain cases of testicular cancer. He referenced the SWENOTECA study for non-seminomatous germ cell tumors (NSGCT), where approximately 25% of patients were downstaged during short-interval observation, with only 5% progressing during this period (only 2 cases outside the retroperitoneum), and a 26% pN0 rate observed. (1) He also highlighted that the pNo rate for all six published primary RPLND for seminoma studies is around 7%. This indicates that a significant number of patients can be managed conservatively with careful monitoring, reducing the need for immediate invasive procedures.
Case # 3- 28 year-old man with NSGCT of the left testis.
- Tumor markers are normal.
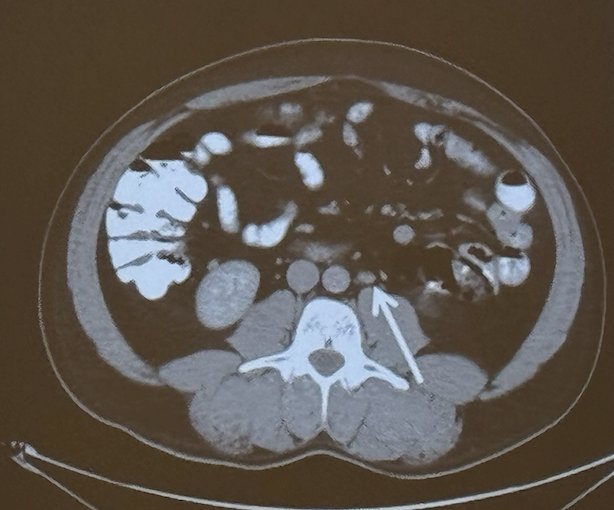
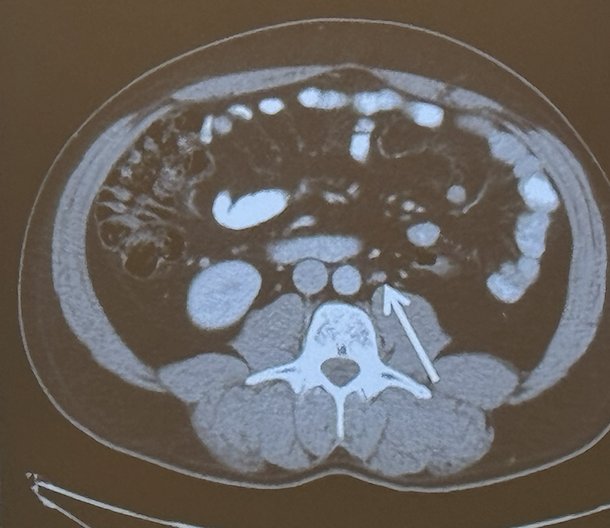
- His initial staging scan showed a left para-aortic lesion suspicious of an enlarged lymph node:
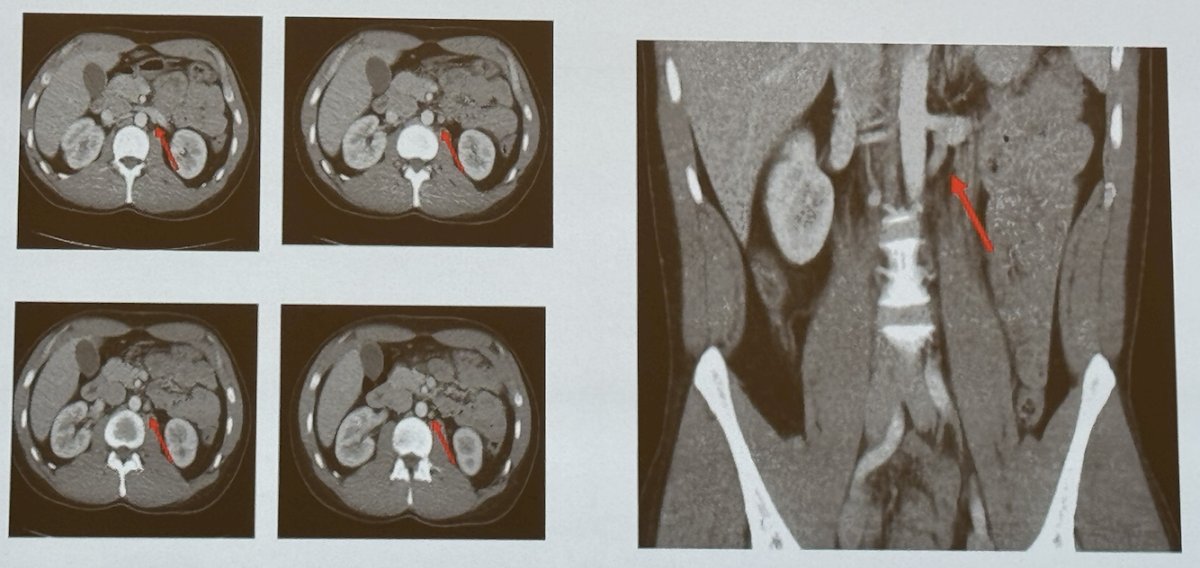
Masquerader #3: Descending lumbar vein
A descending lumbar vein can be easily mistaken for a retroperitoneal lymph node on imaging, which might lead to unnecessary radiotherapy or chemotherapy. To avoid this, it is crucial to review imaging in all planes of the CT scan to correctly identify anatomical structures and avoid misdiagnosis.
Case # 4- 18-year-old man with NSGCT of the left testis + LVI.
- Tumor markers are normal.
- His CT scan pre-orchiectomy was normal. However, his scan post-irchiectomy showed enlarged hypodense masses in the pelvis.
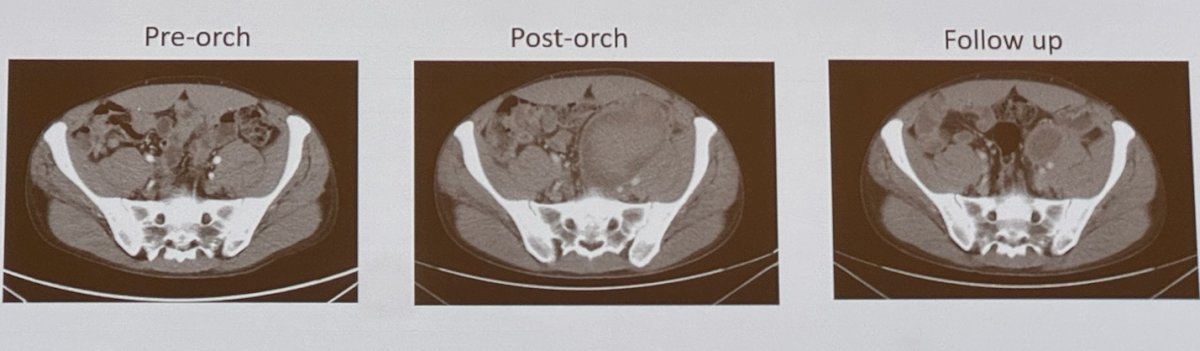
Masquerader #4: Post-orchiectomy Hematoma
This case underscores the critical need for a preoperative scan for comparison and a follow-up scan two months later. These scans are essential to accurately assess changes over time and avoid unnecessary treatments such as radiotherapy or chemotherapy.
Case # 5- A 27-year-old man with poor risk NSGCT of the left testis with HCG > 3.000.000 mIU/mL. The patient completed VIPx4.
- HCG was still elevated to 12.3mIU/mL five months after completing chemotherapy.
- His post-chemotherapy is shown below:

- His additional workup included:
- MR Brain: No evidence of new enhancing intracranial lesion to suggest recurrent or new brain metastasis.
- Repeat cross-sectional imaging: No growth
- Trending the markers every 1-3 weeks: 12.3→10.2 →9.1→8.8→7:5→6.2→ 53→1.4→ 0.6
- Went for RPLND: The pathology showed extensive necrosis with associated fibrosis and histiocytic reaction.
- Went for Lung Resections: pathology with extensive necrosis with associated fibrosis and histiocytic reaction.
- To date the patient remains with no evidence of disease
Masquerader #5: Slow Terminal Half-Life of HCG in Patients with Starting Values >50,000 mIU/mL
Less than 10% of patients with an initial hCG level higher than 50,000 mIU/mL will see their hCG levels normalize by the fourth cycle of chemotherapy. However, up to 50% of these patients can achieve no evidence of disease (NED) status without additional chemotherapy. Dr. Funt advises a cautious approach: take your time and follow closely before deciding on surgery. It's essential to trend the hCG levels and perform imaging evaluations, considering other potential causes for elevated hCG, such as marijuana use, low testosterone, or brain metastasis.
Case # 6- A 35-year-old man with pure embryonal carcinoma of the left testis.
- His pre-chemotherapy scan showed a ~2.5cm Para-aortic lymph node. (Below)
- Tumor markers were elevated.
- He received BEPx3 under the care of an oncologist.
- The post-chemotherapy scan revealed complete resolution of the para-aortic lymph node.

The patient comes four months later with a scan showing a growing cystic mass in para-aortic region with normal serum tumor markers.

Bilatreral nerve-sparing post-chemoterapy retroperitoneal lymph node dissection identifies a larger than 3 cm retroperitoneal mas and the pathology reveals teratoma.
Masquerader # 6: Growing Teratoma
Dr. Funt emphasized that in patients with a growing mass and normal tumor markers after first-line chemotherapy, second-line chemotherapy should not be initiated without pathological confirmation of a viable, non-teratomatous germ cell tumor. He briefly discussed the TIGER Trial (TIP vs. TI-CE in second-line chemotherapy), noting that the inclusion criteria required a tumor biopsy of new, growing, or unresectable lesions to demonstrate the presence of viable non-teratomatous germ cell tumor. This highlights the importance of histological confirmation to guide further treatment decisions and avoid unnecessary chemotherapy.(2)
Case # 7- A 39-year-old man with a mixed NSGCT of the right testis, a 1.5 cm aortocaval lymph node and a rising HCG (11 → 25→113→238)
- The patients starts EPx4 for IGCCCG good risk disease when HCG is 238.
- When he comes in for his Cycle 1,week 2 toxicity check, his HCG has continued to rise to 328.
Masquerader # 7: Tumor marker lysis
Tumor marker lysis, which refers to the transitory elevation in tumor markers, typically occurs during the first to second week of the first cycle of chemotherapy. This phenomenon is a result of the effective destruction of cancer cells by the chemotherapy, leading to the release and subsequent clearance of tumor markers from the bloodstream. It's important to understand that this rapid decrease in tumor markers is a sign of the treatment's efficacy and not indicative of true tumor progression
- The same patient comes during cycle 3, week 2, his AFP went from 2.1 to 10.
Masquerader # 8: Benign fluctuations in AFP
Elevated alpha-fetoprotein levels can occur due to transient liver inflammation, which may be caused by chemotherapy or other medications. This elevation should not be interpreted as true tumor progression. Instead, it is often a side effect of the treatment process itself
Presented by: Samuel A. Funt, MD, Genitourinary Medical Oncologist at Memorial Sloan Kettering Cancer Centre, New York, United States.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 Society of Urologic Oncology (SUO) annual meeting held in Dallas, between the 3rd and 6th of December, 2024.
References:- Gerdtsson A, Negaard HFS, Almås B, Bergdahl AG, Cohn-Cedermark G, Glimelius I, Halvorsen D, Haugnes HS, Hedlund A, Hellström M, Holmberg G, Karlsdóttir Á, Kjellman A, Larsen SM, Thor A, Wahlqvist R, Ståhl O, Tandstad T. Initial surveillance in men with marker negative clinical stage IIA non-seminomatous germ cell tumours. BJU Int. 2024 Jun;133(6):717-724. doi: 10.1111/bju.16289. Epub 2024 Jan 31. PMID: 38293778.
- Gleeson JP, Knezevic A, Bromberg M, Patil S, Sheinfeld J, Carver BS, Bains M, Jones DR, Bajorin DF, Bosl GJ, McHugh DJ, Funt SA, Motzer RJ, Feldman DR. Paclitaxel, Ifosfamide, and Cisplatin as Initial Salvage Chemotherapy for Germ Cell Tumors: Long-Term Follow-Up and Outcomes for Favorable- and Unfavorable-Risk Disease. J Clin Oncol. 2024 Sep 10;42(26):3130-3139. doi: 10.1200/JCO.23.02542. Epub 2024 Jul 19. PMID: 39028926.


