Patients were selected for this study if they had a preoperative sagittal CT tract length of < 10 cm via an upper pole, subcostal approach. Patients were given a preoperative regimen of tamsulosin 0.4 mg one week prior to surgery. A 16F sheath was used to protect the ureter prior to ureteroscope insertion, then the ureteroscope was inserted into the renal pelvis. Two cc of air was injected into the ureteroscope to form an air bubble, thus facilitating the identification of the upper pole calyx. Once the tip of the ureteroscope was confirmed to be aimed at the flank in the correct position, the laser fiber was fired at 1 J and 10 Hz and advanced directly through the posterior upper calyceal fornix and advanced towards the skin. The tip of the laser fiber then broke through the skin and was subsequently grasped in order to pass a needle over the laser fiber to properly dilate the nephrostomy tract (Figure 1). Perioperative data was recorded throughout each procedure.
Nine patients underwent this clever novel procedure. The mean operative time was 202 minutes and mean fluoroscopy time of 32 seconds. Of note, six patients were tested for residual stones using a CT scan on postoperative day 1 which revealed that 0% of these patients were stone free (fragments ≤ 4 mm). These fragment sizes ranged from 2.1 to 8.8 mm, but there was a mean 96% stone volume reduction reported from these patients. There was no significant ureteral injury following the insertion of the ureteral access sheath, but a Clavien IIIa complication was noted due to a subcapsular hematoma and subsequent drop in hemoglobin. This complication was properly treated via embolization and was transfused with two units of red blood cells which led to a full recovery.
By the end of Dr. Kaler’s presentation, several members in the audience were concerned about the viability of this method of tract access. The presenter responded in kind by informing the audience that he does not endorse this procedure to a surgeon that is untrained in retrograde nephrostomy access, as it is a particularly difficult procedure to master. However, Dr. Kaler explained that once a surgeon is proficient at the technique, access times and fluoroscopy times are greatly reduced, thus validating the procedure. In closing, Dr. Kaler reminded the audience that in a highly selective population where a subcostal approach in patients with a skin-to-stone distance < 10 cm, the LEXIT technique was efficacious in establishing a percutaneous nephrostomy tract.
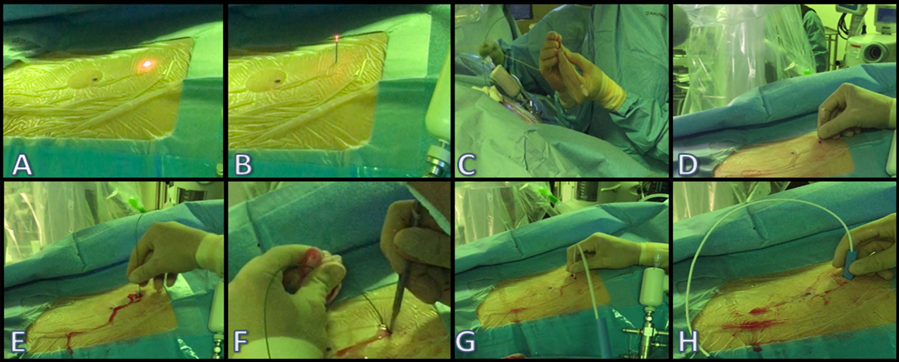
Figure 1: Laser Endoscopic X-ray-guided Intrarenal Tract (LEXIT) technique from the flank view. The glow of the laser beneath the skin is visible (A), followed by the exit of the laser fiber from the skin (B). The subsequent needle insertion and balloon tract dilation can be seen (C-H).
Presented by: Kamaljot S. Kaler, MD, Clinical Assistant Professor, Department of Urology, University of California, Irvine, USA; Department of Surgery, Section of Urology, University of Calgary, Canada
Co-Authors: Egor Parkhomenko, MD, Resident 1, Zhamshid Okhunov 2, Roshan Patel, MD, Assistant Clinical Professor2, Jaime Landman, MD, Professor and Chair2, Ralph Clayman, Professor2, Carlos A. Uribe 3
Author Affiliation:
1. Boston Medical Center
2. The University of California, Irvine, Department of Urology
3. Department of Urology, Hospital Pablo Tobon Uribe, (HPTU), Medellin, Columbia
Written by: Zachary Valley, Twitter: @ZacharyAValley, Department of Urology, University of California-Irvine, medical writer for UroToday.com at the 36th World Congress of Endourology (WCE) and SWL - September 20-23, 2018 Paris, France


