(UroToday.com) On the inaugural day of the WCET 2024 Annual Meeting in Seoul, South Korea, the first moderated poster session of the basic science abstracts was initiated with Dr. Aaron Miller, PhD of the Cleveland Clinic with an insightful study analyzing the prostate microbiome in benign prostatic hyperplasia (BPH) patients.
Benign prostatic hyperplasia is a condition causing lower urinary tract symptoms, affecting 80% to 90% of men who are 70 years of age or older1. Contemporary literature has demonstrated associations between the renal microbiome to prominent GU diseases and conditions including renal cancer, as well as nephrolithiasis. However, there exists a paucity with regard to the prostate microbiome. Accordingly, Dr. Miller and team sought to evaluate the microbiome of the prostate in patients with BPH using Next-Generation Sequencing, as well as assess further associations with patients’ characteristics.
For patient recruitment, males undergoing Holmium Laser Enucleation (HoLEP) for BPH, were included if they were ages 18 or older, had no previous history of prostate cancer or prostate surgery, and had never received pelvic radiation. Further exclusion requirements included: positive preoperative urine culture, bladder stones, or catheter-dependence. Patient metrics such as age, prostate-specific antigen (PSA) levels, American Urological Association Symptom Score (AUASS), and history of prostate biopsy were documented. In order to evaluate the respective microbiomes, intraoperative samples were obtained from prostate tissue, catheterized urine, urethral tissue, and swabs of the specimen container to serve as a negative control. These samples were further subjected to DNA extraction and high-throughput 16S sequencing. Data analysis was completed using R statistics, while Sparcc correlations quantified bacterial taxonomic diversity and patient metrics.
Overall, 50 patients were recruited to the study with a mean age of 67.8 years, PSA 4.00 ng/mL, prostate size of 108.6 g, and AUASS of 19.4. Following bioinformatic decontamination of prostate samples, alpha and beta diversity analyses showed that microbiomes from the prostate, urethra, and urine were all distinct (p = 0.001). In reviewing the number of unique phylogenetic groups analogous to bacterial species following decontamination, there are a unique number of species for each sample, wherein the prostate harbors the lowest diversity overall (Figure 1A). Subsequent beta diversity demonstrates the microbiome composition based on either the presence of absence of bacteria and the relative abundance, where each point is an individual sample and the distance between points is directly correlated to the dissimilarity in microbiome composition. This overall showed that each area depicted by letters (ie. Urethra, urine, and prostate) contained significantly different compositions (Figure 1B).
Following these findings, Dr. Miller and colleagues aimed to characterize the overlap among various species present in their respective samples. Overall, they identified a low overlap (<20%) between the prostate and either urine or urethra), and a high overlap between the urethra and urine; which further suggests that the microbiome of the prostate is vastly different from the aforementioned groups (Figure 1C). These findings encouraged further evaluation between each sampling, which was completed in a pairwise fashion. The two prostate comparisons demonstrated higher beta diversity values, where beta diversity is given in a range from 0-1 with 1 representing the least similarity, as compared to the urethra and urine group, further suggesting a difference in prostate microbiota (Figure 1D).
 Figure 1. The prostate microbiome is unique. A) Number of unique phylogenetic clades; B) Microbiome composition; C) Overlap in taxa between tissues; D) Between-group similarity in microbiome composition.
Figure 1. The prostate microbiome is unique. A) Number of unique phylogenetic clades; B) Microbiome composition; C) Overlap in taxa between tissues; D) Between-group similarity in microbiome composition.
Furthermore, Dr. Miller and team sought to identify the specific taxonomic signature of BPH symptoms, as related to age (passive accumulation of bacteria), AUASS, prostate size, and PSA level. While only one strain was correlated with age, uropathogens including Campylobacter, Caryophanaceae, Enterobacter, and Senegalimassilia were positively correlated with prostate size or PSA (Figure 2). Additionally, there was no significant association between AUASS and history of prostate biopsy for specific bacteria.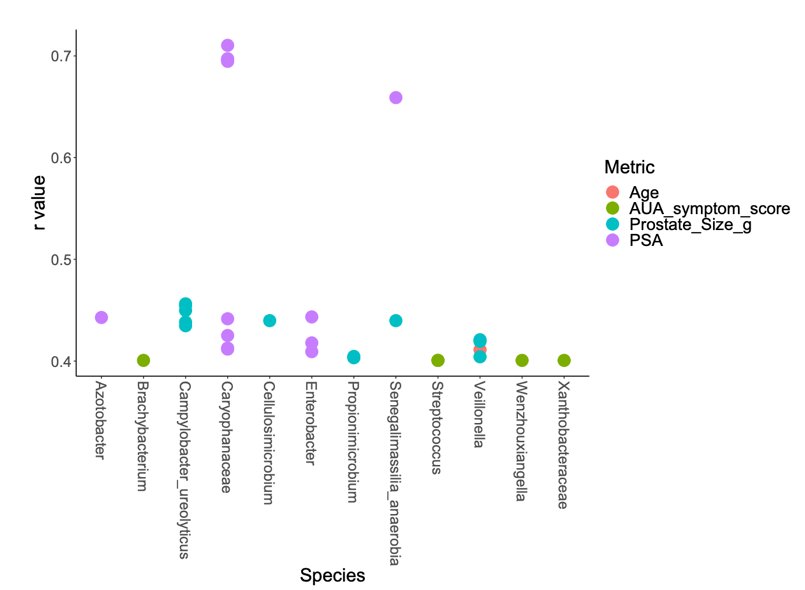
Figure 2. Correlations between age, PSA, prostate size, and AUASS reveal unique associations with known uropathogens.
Upon concluding his presentation, Dr. Miller’s talk sparked a lively discussion. Moderator Dr. Jeffrey Gahan, MD of UT Southwestern Urology shared, “This is a very specific set of patients. It is difficult to study patients who have not undergone HoLEP (ie only maintained on alpha-blockers), however, it would be interesting to evaluate whether this is correlated with patients with BPH or only those who are chronically obstructed that require surgical intervention”.
In response, Dr. Miller stated, “Indeed, it is a very specific subset, and we did not have healthy controls, which we may certainly do [in future studies]. Our data gives specific targets with specific bacteria which we plan to bring this into a mouse model, to elucidate bacterial mechanisms…which may include bacterial attachment to cells, biofilm formation, and production of toxic metabolites.”
Dr. Gahan had an additional question regarding clinical implications, primarily involving negative urine cultures which may not detect such species, further questioning the utility of antibiotics vs other anti-bacterial agents for targets. Dr. Miller then reported, “We have completed a surmountable volume of studies reviewing the impact of antibiotics on urinary tract bacteria, which have demonstrated these may promote the growth of uropathogens compared to true elimination. Therefore, we are aiming to target specific pathologic features such as inhibiting bacterial attachment to cells and biofilm formation in general. Ultimately, this may offer a more effective and long-term solution compared to antibiotics…healthy bacteria may also be beneficial in the inhibition of BPH symptoms.”
In summary, Dr. Miller et al. concluded with these lasting thoughts from his presentation:
- These findings are the first to correct for possible contaminants while using prostate tissue
- The prostate contains a unique microbiome
- Taxa such as Campylobacter or Caryophanaceae are associated with prostate size or PSA levels independent of age
- These results warrant the requirement of further mechanistic studies
Presented by: Aaron Miller, PhD, Cleveland Clinic, Cleveland, OH
Written by: Mariah Hernandez, Research Specialist, Department of Urology, University of California Irvine, @mariahch00 on Twitter during the 2024 World Congress of Endourology and Uro-Technology: August 12 -16, 2024, Seoul, South Korea
References:
- Ng M, Leslie SW, Baradhi KM. Benign Prostatic Hyperplasia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.


