(UroToday.com) At the WCET 2024 conference in Seoul, Dr. Thomas Ahlering from the University of California, Irvine, presented a groundbreaking study that challenges the conventional understanding of positive surgical margins (PSMs) following radical prostatectomy (RP).
Traditionally, PSMs have been regarded as a negative prognostic indicator, associated with worse long-term outcomes such as higher prostate cancer-specific mortality (PCSM) and overall mortality (OM). However, this study introduces a new dimension to the discussion by highlighting the role of pathological tumor volume (pTV) as a more significant predictor of these outcomes.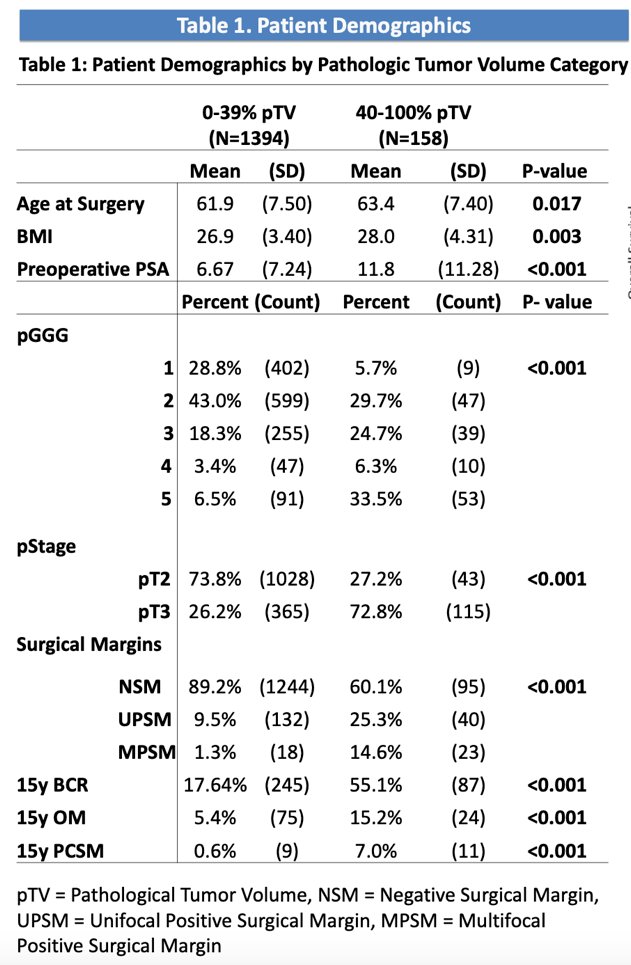
The study analyzed data from 1,322 patients who underwent RP by a single surgeon between 2002 and 2018. Utilizing Kaplan-Meier survival curves, the researchers stratified patients based on margin status and whether their pTV was greater or less than 40%. The aim was to assess how these factors influenced key outcomes, including biochemical recurrence, OM, and PCSM.
Results showed that patients with a pTV greater than 40% tended to have more aggressive cancer, as indicated by higher grades and stages at baseline. Over a 10-year follow-up, these patients exhibited significantly higher rates of biochemical recurrence, OM, and PCSM, with strong statistical significance (p < 0.001). Furthermore, the study found a significant association between high pTV and increased PSM rates, including multifocal margins. Notably, for patients with a pTV below 40%, the presence of PSMs did not significantly affect long-term mortality, suggesting that pTV might be a more critical factor in predicting patient outcomes than PSMs alone.
During the Q&A session, an audience member raised a question regarding whether the study’s results were controlled for any specific factors in the survival analysis. Dr. Ahlering clarified that the survival analysis was controlled for both stage and grade, ensuring that these important variables were accounted for in the study’s conclusions.
This study suggests that while minimizing PSMs remains important, pTV could be a more reliable predictor of adverse oncologic outcomes. The findings advocate for a more nuanced approach in surgical planning and patient management, where the focus shifts from merely minimizing PSMs to also considering the broader oncologic profile, particularly pTV. This could lead to more personalized treatment strategies that balance the need for oncologic control with preserving the quality of life, particularly in terms of urinary and sexual function.
Dr. Ahlering’s presentation adds valuable insights to the ongoing discussion about prostate cancer treatment, emphasizing the need for a more tailored approach based on individual patient characteristics. This study, conducted without external funding, offers important considerations for future clinical practices in managing prostate cancer.
Presented by: Thomas Ahlering, MD, Department of Urology, University of California, Irvine, Irvine, CA
Written by: Seyedamirvala Saadat, Research Specialist at Department of Urology, University of California Irvine, @Val_Saadat on X during the 2024 World Congress of Endourology and Uro-Technology: August 12 -16, 2024, Seoul, South Korea


