(UroToday.com) At the annual WCET 2024, a plenary session included a panel on the management of multiple small renal masses (SRMs). This included a presented argument by respective conservative, intermediate, and prompt approaches moderated by Dr. Woong Kyu Han, MD. Honored panelists included Dr. Jason Y. Lee, MD, MHPE, FRCSC, Dr. Orit Raz, MD, and Dr. Jaime Landman, MD.
Dr. Woong Kyu Han kicked off the session with two case presentations that require management: 1) A 45 yo healthy male with normal renal function, and a left 3.0 cm and right 1.5 cm, 0.8 cm mid portion masses, 2) 56 yo Von Hippel-Lindau (VHL) male with normal renal function and a 2.4 cm right tumor and two left tumors measuring 4.0 and 3.7 cm. Such SRMs that are especially challenging to surgeons may include those that are bilateral, synchronous, and metachronous. Notably, literature has shown benign rates for SRMs ranging from 15-30%, with average growth rates of 2-3 mm per year. Moreover, without any intervention, there is a low risk of metastasis within 5 years of diagnosis.
For this with SRMs, Dr. Lee considers the optimal choice for oncological outcomes, renal function preservation, treatment morbidity, and accessibility, wherein partial nephrectomy, “may not be the best option for all patients, it is for most patients.” In the case of the indicated patients, both are young and healthy, serving as good candidates for this approach. Given there is no major difference in oncologic outcomes of partial and radical nephrectomy, where partial confers a 95% 5-year disease free survival rate, there are excellent outcomes that permit partial nephrectomy as a beneficial option for these patients of Dr. Lee’s practice. Over the previous decade, partial nephrectomy techniques have been optimized to reduce parenchymal loss, as many surgeons no longer use a capsular layer renorrhaphy technique due to local ischemia; while many are also practicing enucleation techniques for safe margins.
Dr. Lee further remarked, “Even in cases where I have a focal positive margin, I have solace in the fact that data suggests in low grade, low risk SRMs, focal positive margin does not impact overall survival for cancer specific mortality,”. Indeed, he proceeded to share that radical and partial nephrectomy do not differ in renal function outcomes, similar to treatment morbidity. He further presented an argument against ablation, where adequate tumor cell depth for treatment requires an ablation zone 5 mm beyond the margin of tumor. When treating large or multiple tumors with ablative therapy like the aforementioned index patients, there may be a significant amount of parenchymal loss compared to partial nephrectomy (Figure 1). In comparison to ablation, in a sample of the largest case series published, the oncologic outcomes of ablation remain suboptimal to those of partial nephrectomy. Moreover, size is important for ablation, wherein tumors beyond a 3 cm threshold have decreased oncologic outcomes. There may also be an increased risk of complications as compared to partial nephrectomy, especially for cases with larger and multiple renal tumors. He concluded his review by reviewing AUA Guidelines, suggesting partial nephrectomy for all T1a renal masses.
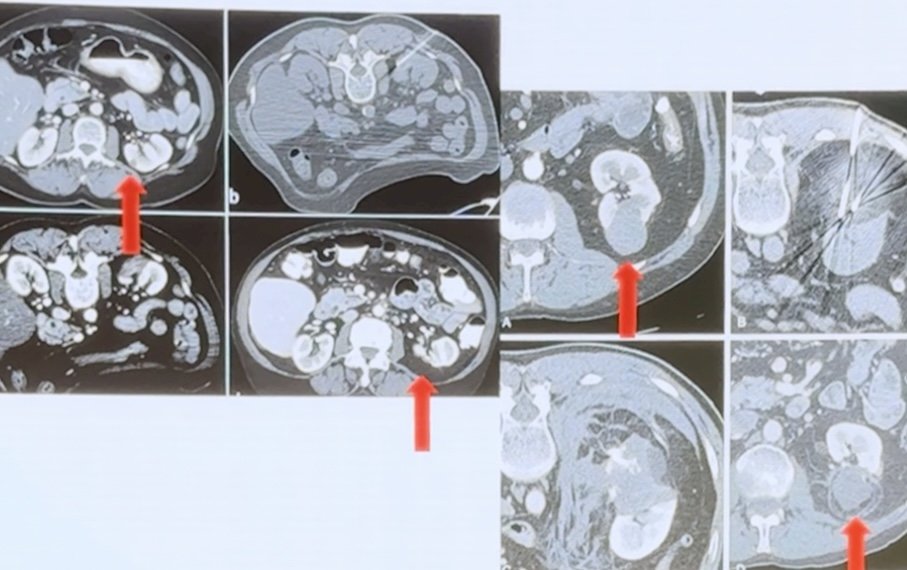
Figure 1. Comparison of pre and post operative parenchymal loss.
The talk then continued with Dr. Raz contributing to the argument for robust therapy, radical nephrectomy. Although surgeons aim to achieve superior outcomes with optimal approaches, she notes that there is no randomized controlled trial to date that includes and compares all three options discussed in today’s plenary. After reviewing treatment considerations including tumor characteristics and patient history, Dr. Raz reviewed studies of SRMs for radical nephrectomy which demonstrated 5% multifocality and 11% with bilateral disease. She then reviewed cases in which a patients who underwent partial nephrectomy for cystic appearing lesions were found to have ccRCC (Figure 2), and an additional patient who underwent both partial nephrectomy and ablation that caused chronic ureteral damage and urine leakage. As a lasting message, Dr. Raz emphasized the severity of RCC, wherein it is most safe for a radical approach.
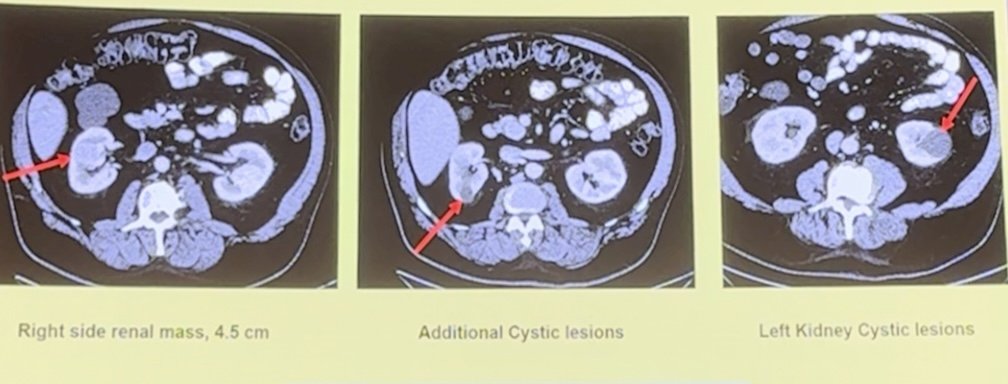
Figure 2. Bilateral SRMs with final diagnosis of ccRCC.
Lastly, Dr. Landman then presented his approach to SRMs, highlighting percutaneous cryoablation. (Unfortunately, there were technical issues and he presented without slides) Important factors for consideration of ablation include oncologic disease management, renal function, minimal invasiveness, and complications, as well as cost. Including 7% of patients who require additional cryoablative therapy, there will be equal oncologic control in comparison to partial nephrectomy. With regard to renal function, whether creatinine, GFR, parenchymal volume, or renal scan are used, ablation will result in superior outcomes. Though ablation may require a larger radius, “The data is crystal clear, oncologic control is perfect, and renal function is best with ablative therapy than compared to any other extirpative technology”. Without the need for anesthesia, patients can return home within a day, significantly reducing costs compared to other therapies
For the first patient case, he would opt for renal biopsy to confirm the absence of malignancy given the feasibility of other diseases. Additionally, this patient is anatomically not suitable for percutaneous ablation and would be deferred to the two previous mechanisms of action. For the second case, Dr. Landman states that the right sided 2.7 cm tumor associated with VHL would prove to be ccRCC. However, the left sided tumor is limited by the sagittal-only views of his CT imaging. Therefore, ablation is considered for possibility.
In conclusion, the panel on managing multiple SRMs discussed diverse approaches to treatment, each tailored to specific patient cases. Dr. Lee advocated for partial nephrectomy, emphasizing its balance of oncologic outcomes, renal function preservation, and reduced morbidity. Dr. Raz supported radical nephrectomy, underscoring its safety in the face of multifocal and bilateral disease. Meanwhile, Dr. Landman discussed percutaneous cryoablation, noting its superior renal function outcomes and minimal invasiveness, although he acknowledged limitations based on tumor size and location. The session underscored the importance of individualized treatment strategies for optimal patient outcome
Moderated by: Woong Kyu Han, MD, Yonsei University College of Medicine, South Korea
Panelists:
- Jason Y. Lee, MD, MHPE, FRCSC – University of Toronto, Canada
- Orit Raz, MD – Assuta Ashdod Public Hospital, Israel
- Jaime Landman, MD – University of California, Irvine, USA
Written by: Mariah Hernandez, Research Specialist, Department of Urology, University of California Irvine, @mariahch00 on Twitter during the 2024 World Congress of Endourology and Uro-Technology (WCET) Annual Meeting, August 12 -16, 2024, Seoul, South Korea


