Dr. Penniston opened the plenary on "Myths and Misconceptions of Diet and Stone Prevention" with an engaging discussion. She deconstructed the turbulence regarding dietary advice for stone prevention, which in part arises from the complexity of the condition, with various stone types posing unique etiologies and risk factors. She proceeded to refute the traditional “one-size-fits-all” approach to dietary advice, as it is dually illogical and culturally insensitive.
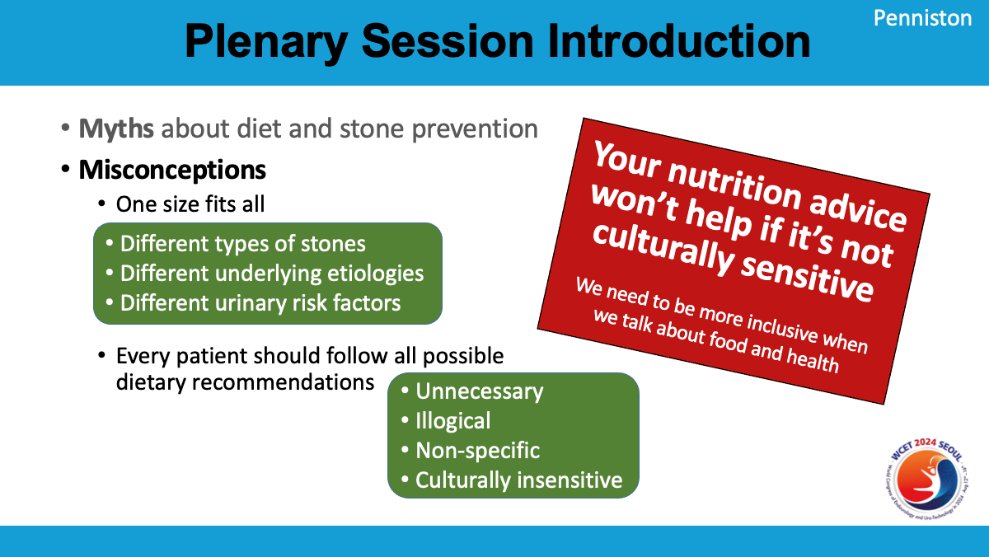
Instead, Dr. Penniston urged the audience to adopt personalized regimens for patients, stressing the importance of cultural sensitivity in dietary recommendations. With this foundation, Dr. Penniston introduced the four experts who would address the truths behind four key dietary topics: calcium, coffee and tea, oxalate, and soda.
Dr. Sri Sivalingam kicked off his talk by emphasizing the significant role that both genetic and environmental factors—particularly diet—play in kidney stone disease. He highlighted that calcium intake is essential for maintaining body homeostasis, particularly for bone health, muscle function, and renal function. However, calcium has often come under scrutiny, especially regarding its supplementation and the perceived link to stone formation.
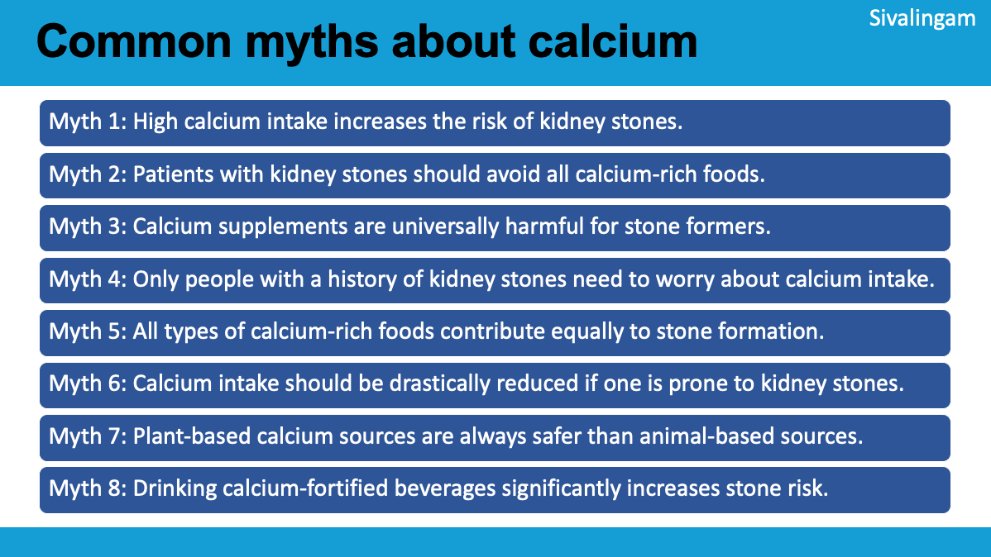
Dr. Sivalingam then addressed three major myths, among many, surrounding calcium and kidney stones. First, he tackled the belief that high calcium intake increases the risk of kidney stones, explaining that, in reality, patients with idiopathic hypercalciuria often excrete more calcium than they consume when placed on low-calcium diets. This restriction not only increases stone risk but also negatively impacts bone health, leading to decreased bone density and higher bone resorption. A randomized control trial, which compared normal (1200 mg/day) versus reduced (400 mg/day) calcium diets in hypercalciuric men, revealed that adequate dietary calcium intake lowers the risk of stone recurrence by 51%, highlighting the importance of physicians to avoid restricting calcium intake.
Moving to the second myth—that patients with kidney stones should avoid calcium-rich foods—Dr. Sivalingam clarified that low dietary calcium can elevate urinary oxalate levels since calcium naturally binds to phosphate and oxalate in the gut. He affirmed that an adequate calcium intake of 1000-2000 mg/day not only lowers oxalate levels but also reduces the recurrence of stones.
Finally, tackling the third myth—that calcium supplements are detrimental to kidney stone formers—he clarified that while supplements can raise stone risk if not taken with meals, they do not pose a risk when used correctly. Supplements consumed without meals lead to a rise in urinary calcium excretion without the benefit of oxalate binding, increasing the likelihood of stone formation by 20%.
In conclusion, Dr. Sivalingam referred to the AUA and EAU guidelines, which recommend limiting sodium intake, ensuring a daily dietary calcium intake of 1000-1200 mg, and taking calcium supplements with meals. He emphasized that all three myths are false, advocating for proper calcium intake as part of effective stone prevention.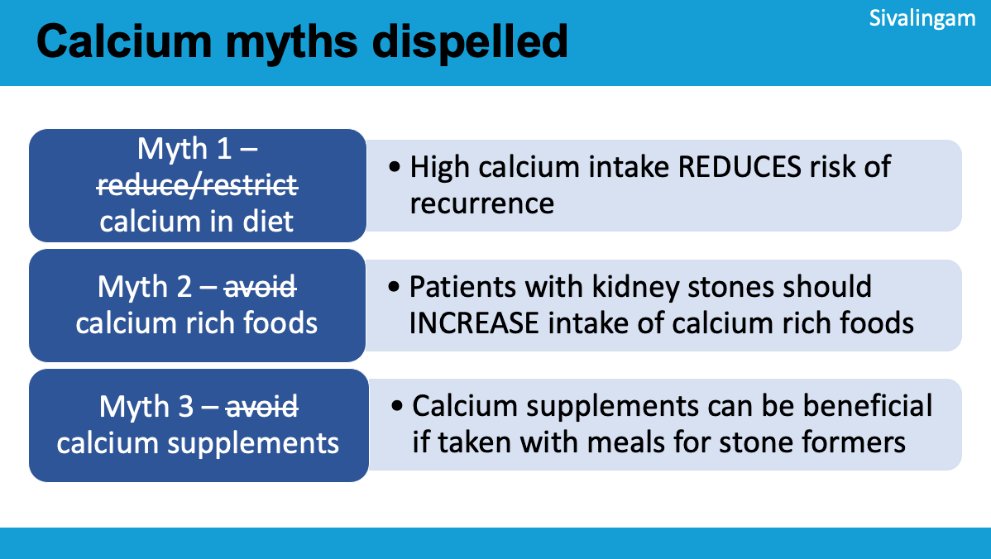
Part 2: Coffee and Tea
Dr. Tae Heon Kim's presentation focused on the debated role of coffee and tea in kidney stone formation. He began by acknowledging that coffee and tea, high in caffeine, are often thought to increase oxalate levels and calcium excretion in the urine, potentially leading to hypercalciuria and a higher risk of kidney stones.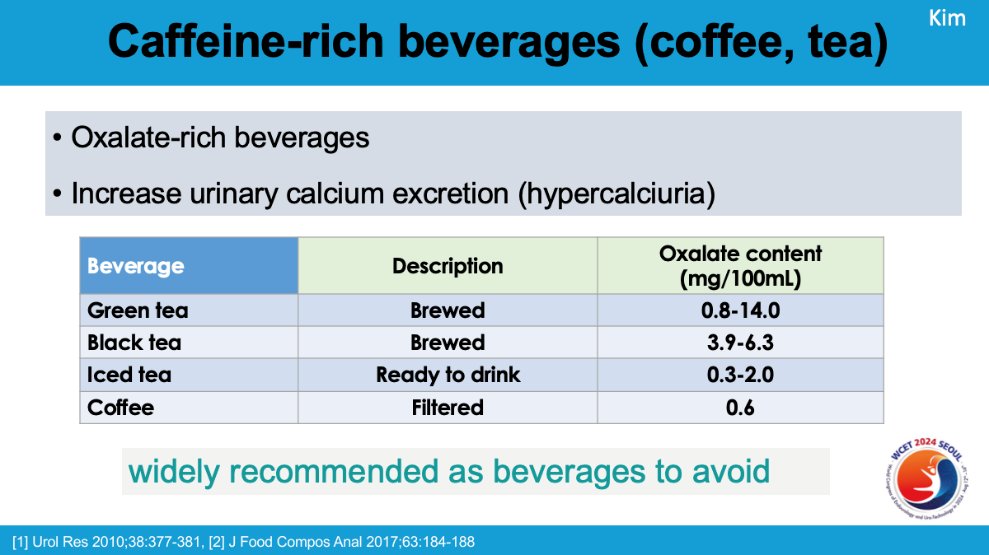
However, Dr. Kim highlighted research suggesting the opposite—that caffeine and coffee might contribute to the prevention of stone formation due to their diuretic effects. Caffeine increases urine flow by affecting adenosine receptors in the kidneys and can also reduce the adhesion of calcium oxalate crystals to kidney cells. Additionally, coffee contains citric acid, which is known to inhibit stone formation, and both regular and decaffeinated coffee offer similar protective benefits.
Dr. Kim presented conflicting data from clinical studies. While some research indicates that caffeine increases calcium excretion and may raise the risk of stone formation, larger studies, such as the National Health and Nutrition Examination Survey, show a correlation between higher caffeine intake and increased stone recurrence.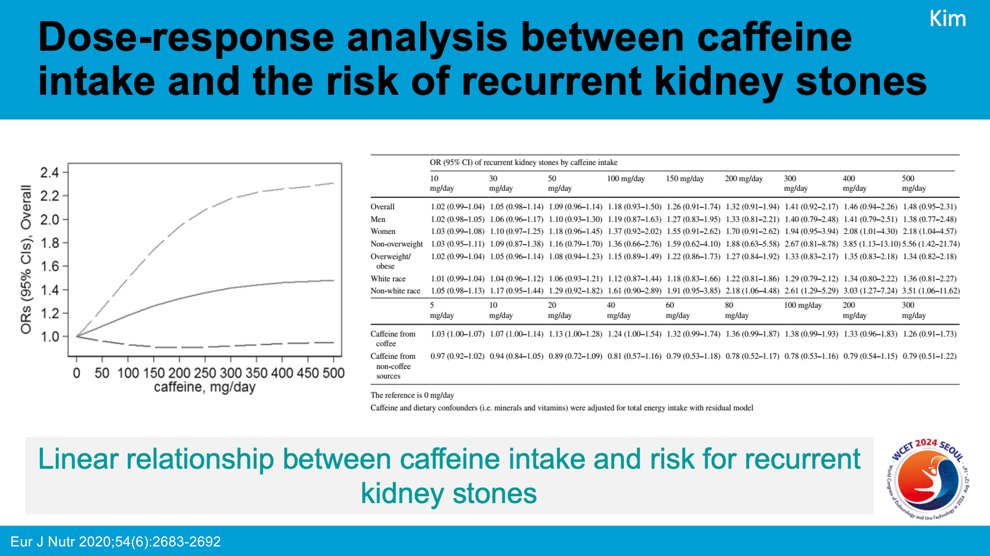
On the other hand, multiple cohort studies suggest that increased caffeine intake decreases the risk of kidney stones, presenting a complex picture.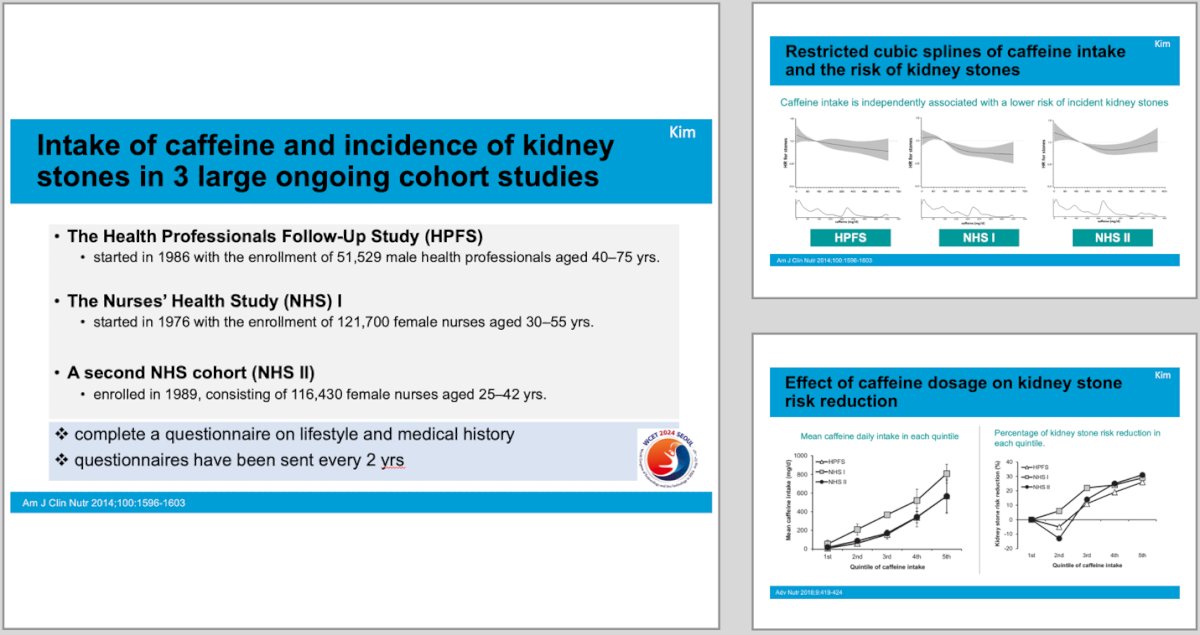
To resolve these contradictions, Dr. Kim referenced a Mendelian randomization study, which used genetic data to explore the causal link between coffee consumption and kidney stones. This study found that even small increases in coffee intake significantly reduced the risk of kidney stones, with just one extra cup of coffee per day lowering the risk by 19%.
In conclusion, Dr. Kim noted that while results on this topic remain inconsistent, a combination of high-quality observational studies and genetic evidence suggests that higher coffee and tea intake may reduce the risk of kidney stones, rather than increasing it.
Part 3: Oxalate
Dr. Roshan Patel's presentation explored the intricacies of oxalate and its connection to kidney stone formation. Oxalate, a compound naturally occurring in plants and excreted primarily by the kidneys, easily binds with calcium to form calcium oxalate (CaOx) crystals, which are a leading cause of kidney stones.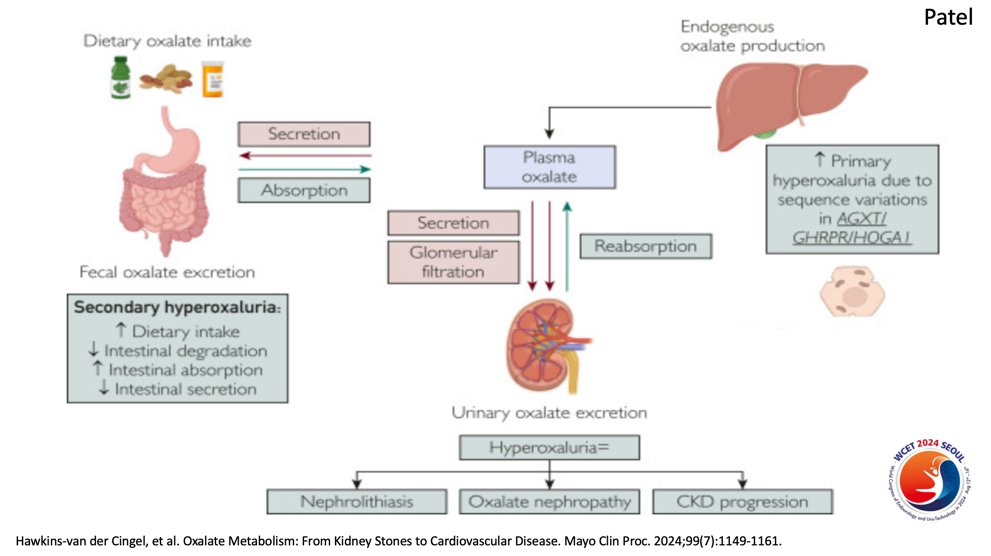
Patel explained that hyperoxaluria—excessive oxalate in the urine—can stem from both dietary and endogenous sources, contributing not only to kidney stones but also to oxalate nephropathy and the progression of chronic kidney disease (CKD), as calcium oxalate is practically insoluble and crystallizes in the renal tubules. He humorously noted that while people often assume something like a green smoothie is healthy because it's plant-based, it’s not always that simple when it comes to oxalate content.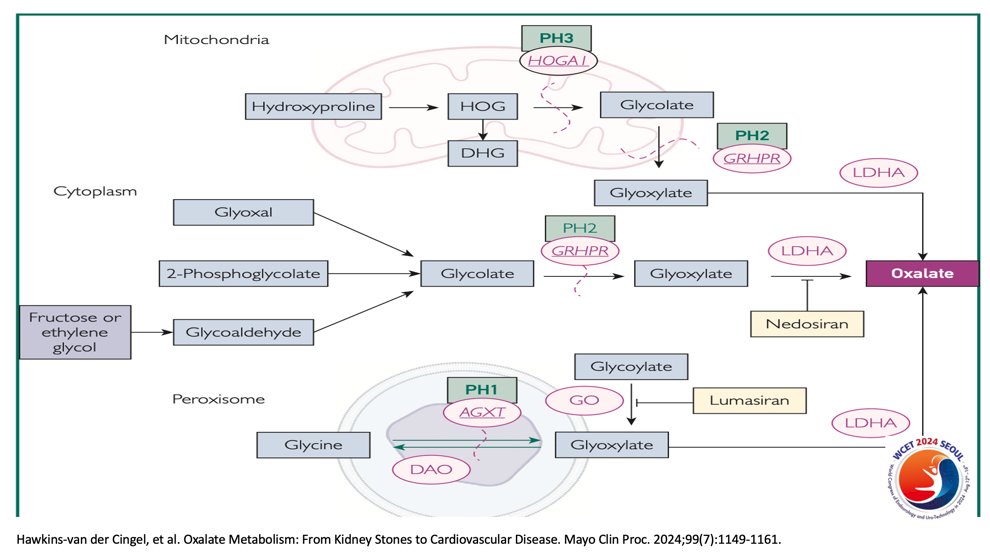
Patel discussed emerging therapies like Lumasiran and Nedosiran, which target oxalate production in the liver, showing promise in reducing oxalate levels in patients with primary hyperoxaluria. He also highlighted data from studies showing that a low-oxalate diet can reduce kidney stone recurrence, though the efficacy depends on the composition of the stones, particularly if they contain significant amounts of CaOx crystals.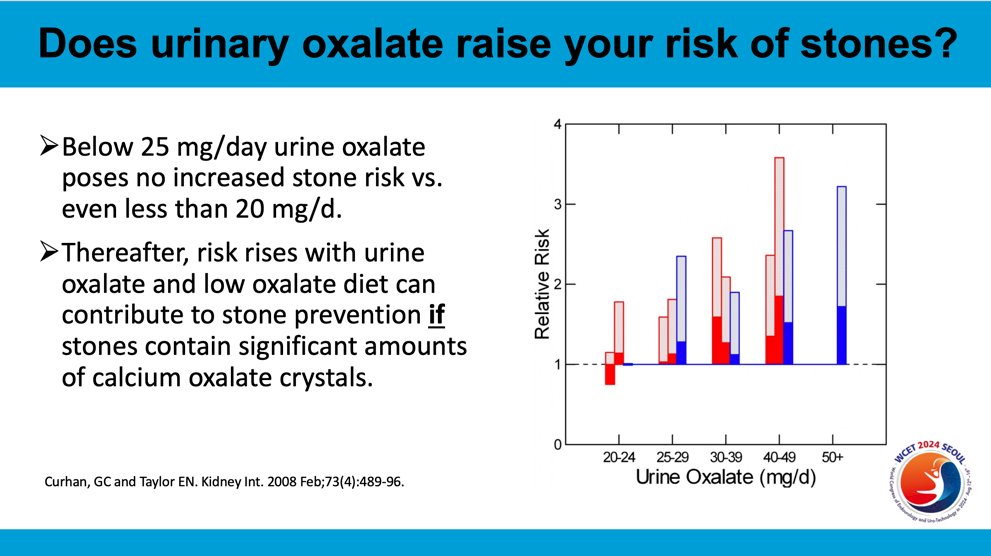
Regarding oxalate-rich foods, Patel emphasized that a "low oxalate diet" has no universal definition, as oxalate content in foods varies due to factors like soil composition, plant maturity, and cooking methods. Some high-oxalate foods include spinach, rhubarb, and almonds, which should be limited in patients with CaOx stones. Rather than overwhelming patients with lists, Patel recommended focusing on avoiding these high-oxalate foods while ensuring adequate calcium intake to reduce oxalate absorption in the gut.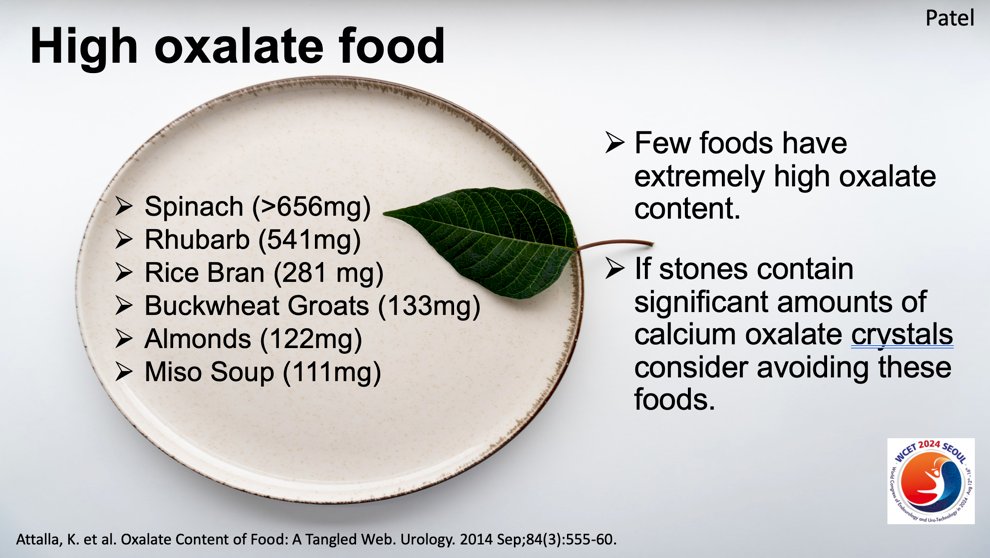
He underscored that dietary calcium—ideally 1,000 to 1,200 mg/day from food—plays a crucial role in controlling urinary oxalate levels. Additionally, lowering dietary sodium can reduce urinary calcium excretion, further decreasing stone risk. Patel cautioned against the overemphasis on oxalate reduction, as a diet too low in plant-based foods can lead to poor nutrition, with detrimental effects on overall health, including the loss of essential antioxidants and fiber.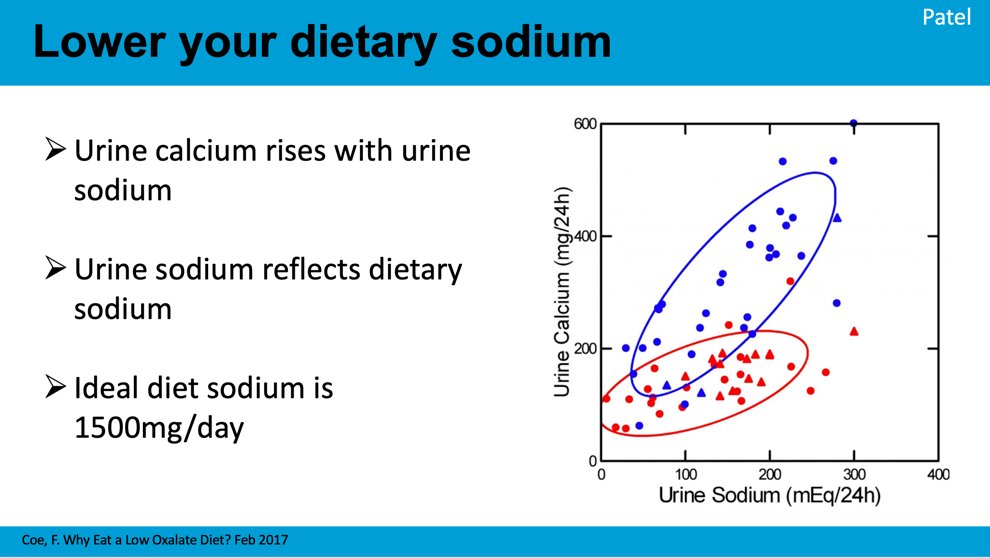
In conclusion, Dr. Patel stressed that therapeutic dietary changes must be sustainable, evidence-based, and tailored to each patient’s stone composition and risk factors. A balanced diet rich in fruits, vegetables, and adequate calcium, coupled with lower sodium intake, is key to reducing kidney stone recurrence. His final note encouraged moderation, humorously advocating to "go for that green smoothie" approach to a healthy, oxalate-conscious diet.
Dr. Roswitha Siener focused on fluid intake and its impact on kidney stone prevention, emphasizing that increased urine volume reduces the risk of stone formation. She recommended a urine output of at least 2.0 to 2.5 liters per day and raised the question of whether sodas are suitable beverages for achieving this. While some systematic reviews found no link between soda consumption and stone formation, more recent studies suggest high soda consumption may increase the risk of nephrolithiasis.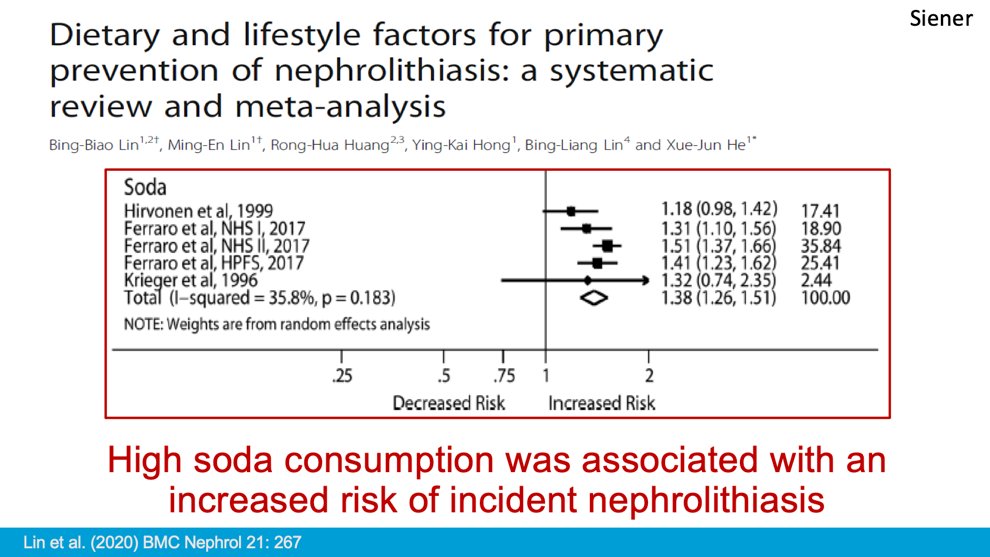
The inconsistency, she explained, could stem from the broad definition of "soda," which includes a wide range of carbonated beverages with varying ingredients, such as sugar, artificial sweeteners, and phosphoric acid.
One key finding was that cola consumption, particularly those containing phosphoric acid, posed a greater risk for kidney stone recurrence. In a study with four volunteers consuming three quarts of cola per day, unfavorable changes in urinary risk factors for calcium oxalate stone formation were observed. On the other hand, diet cola, citrus soda, and mineral water did not significantly alter urinary risk factors, likely due to their low citrate content.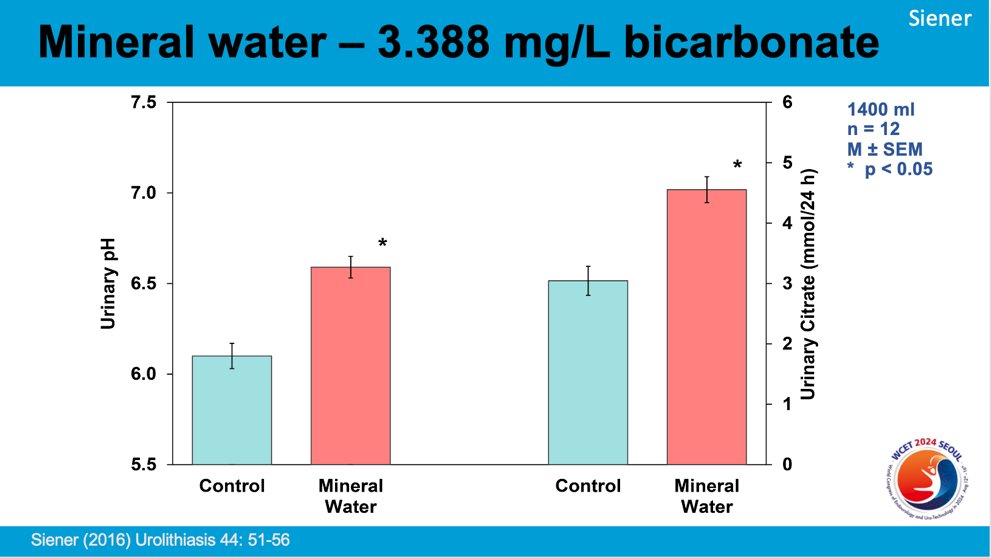
Dr. Siener also highlighted the benefits of bicarbonate-rich mineral water, which was shown to increase urinary pH and citrate excretion, both of which are protective against stone formation. In a study with 34 calcium oxalate stone formers, significant increases in urinary pH were observed after consuming 1.5 liters of bicarbonate-rich water daily compared to low-bicarbonate water.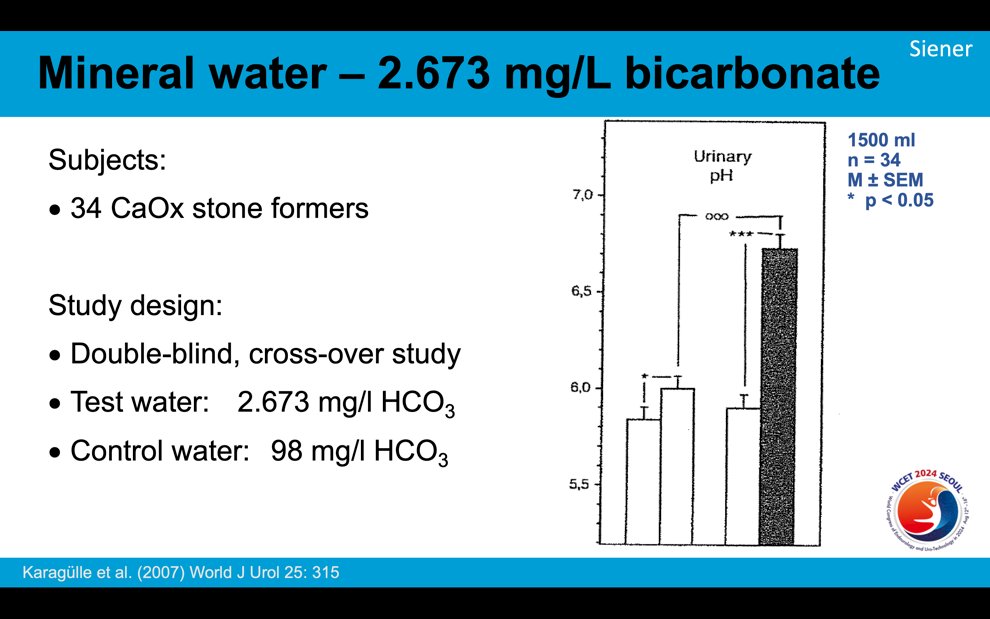
In conclusion, Dr. Siener recommended avoiding cola to reduce the risk of stone recurrence and suggested bicarbonate-rich water as a promising option for stone prevention. However, she noted that further research is needed to understand the long-term effects of other sodas on kidney stone formation.
This plenary panel session, led by Dr. Penniston, featured insightful talks from four experts, each addressing common misconceptions in diet and stone prevention. Dr. Sivalingam debunked myths about calcium, emphasizing that adequate dietary intake lowers stone risk and that calcium supplements are safe when taken with meals. Dr. Kim discussed the controversial relationship between caffeine and kidney stones, suggesting that while high caffeine intake can increase stone risk, moderate consumption of coffee and tea may reduce it. Dr. Patel unpacked the complexities of oxalate, underscoring the importance of managing dietary calcium to lower oxalate levels rather than relying solely on low-oxalate diets. Finally, Dr. Siener highlighted the impact of fluid intake, advocating for the avoidance of cola and suggesting that bicarbonate-rich water may help reduce stone recurrence. Together, their talks called for personalized, evidence-based approaches to dietary kidney stone prevention.
Presented by:- Sri Sivalingam, MD, FRCSC, Cleveland Clinic, Cleveland, OH @ssivalingammd
- Tae Heon Kim, MD, PhD, CHA University, Pocheon, South Korea
- Roshan M. Patel, MD, University of California, Irvine, Irvine, California @roshanpatel_md
- Roswitha Siener, PhD, Universitäs Klinikumbonn, Bonn, Germany
Moderated by: Kristina L. Penniston, PhD, RDN, FAND, University of Wisconsin-Madison, Madison, WI @urologyRDN
Written by: Seyed Amiryaghoub M. Lavasani, B.A., University of California, Irvine, @amirlavasani_ on Twitter during the 2024 World Congress of Endourology and Uro-Technology (WCET) Annual Meeting, August 12 -16, 2024, Seoul, South Korea


