(UroToday.com) On Thursday, August 15, 2024, during the WCET 2024, a plenary panel session was dedicated to discussing robotic radical prostatectomy and strategies to achieve better continence outcomes for patients undergoing the procedure. The session, moderated by Dr. Atsushi Takenaka, MD, PhD, opened with an emphasis on the critical importance of continence outcomes and their profound impact on patients' quality of life.
Dr. Takenaka presented data highlighting significant differences in physical functioning, role physical, body pain, social functioning, role emotional, and mental health between patients who achieved urinary continence and those who did not. These findings underscored the essential role that continence plays in both the physical and mental well-being of patients.
Dr. Takenaka then introduced the various factors that can predict continence outcomes, which he categorized into three main areas: preservation, reconstruction, and reinforcement. He explained that these elements work together to influence the surgical outcomes for patients. Preservation involves maintaining critical structures during surgery, such as the bladder neck, neurovascular bundle (NVB), puboprostatic ligament, pubo-vesical complex, and urethral length. Reconstruction focuses on techniques like posterior and anterior reconstruction and the management of the endopelvic fascia. Reinforcement includes methods like bladder neck plication and sling suspension to further support continence.
For the purpose of the plenary, the discussion then shifted towards preservation surgical approaches, particularly those that aim to maintain anatomical structures to improve continence outcomes. Dr. Cheol Kyu Oh, MD, PhD, was the first panelist invited to speak, and he focused on the Retzius-Sparing Approach. Dr. Oh emphasized that achieving better continence outcomes requires a combination of preservation, reconstruction, and reinforcement, with the Retzius-Sparing Approach being a preferred method due to its emphasis on preservation.
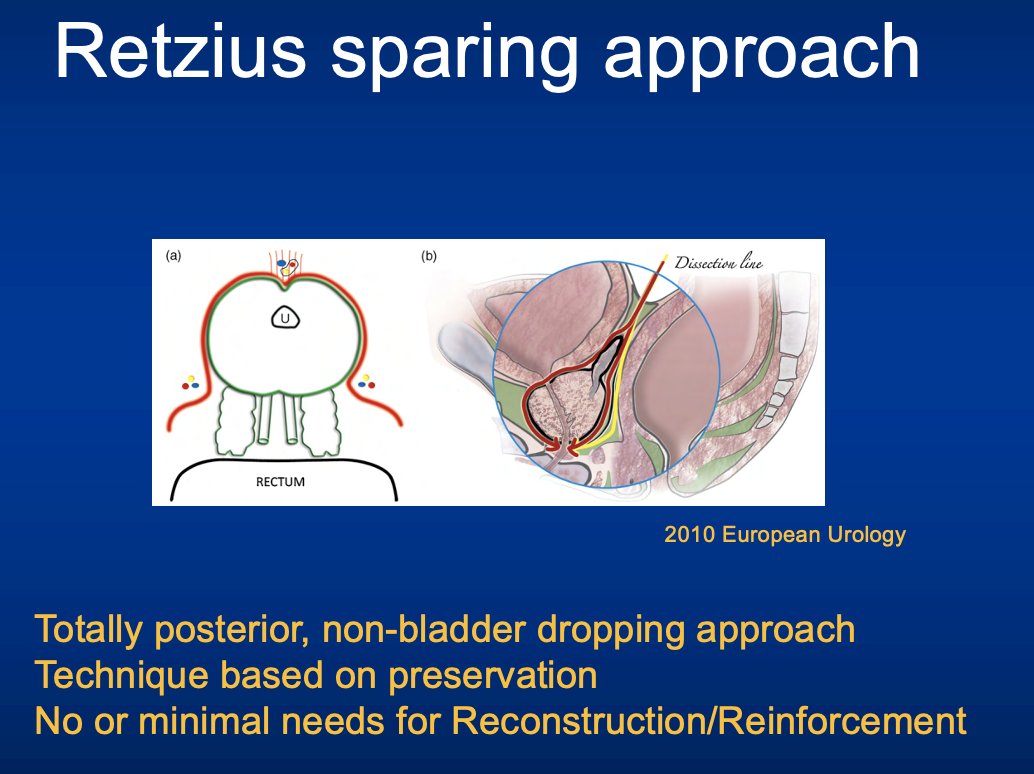
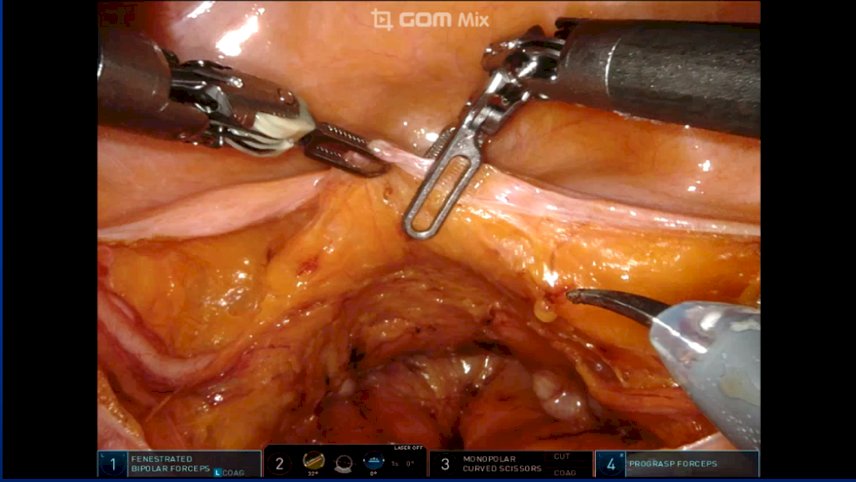
The Retzius-Sparing Approach, as Dr. Oh explained, is a fully posterior technique that avoids bladder dropping, focusing entirely on preserving structures with minimal need for additional reconstruction or reinforcement. During Robotic-Assisted Radical Prostatectomy (RARP), this approach allows for the preservation of the bladder neck, Neurovascular Bundle (NVB), sphincter complex, and urethral length, which are all critical for optimal continence outcomes. Dr. Oh demonstrated the surgical technique through a step-by-step video of a robotic case, emphasizing key steps designed to enhance continence outcomes. The surgery began with a non-bladder-dropping approach and was followed by the preservation of seminal vesicle vessels, a crucial step that Dr. Oh identified as vital for maintaining continence. He also discussed the preservation of posterolateral structures, which can be achieved depending on the disease stage and preoperative assessments, including biopsy and MRI results. He showed how the NVB and lateral structures could be preserved, and how nearly all surrounding structures of the prostate, including the bladder neck and anterior/apical structures, can be carefully dissected and preserved.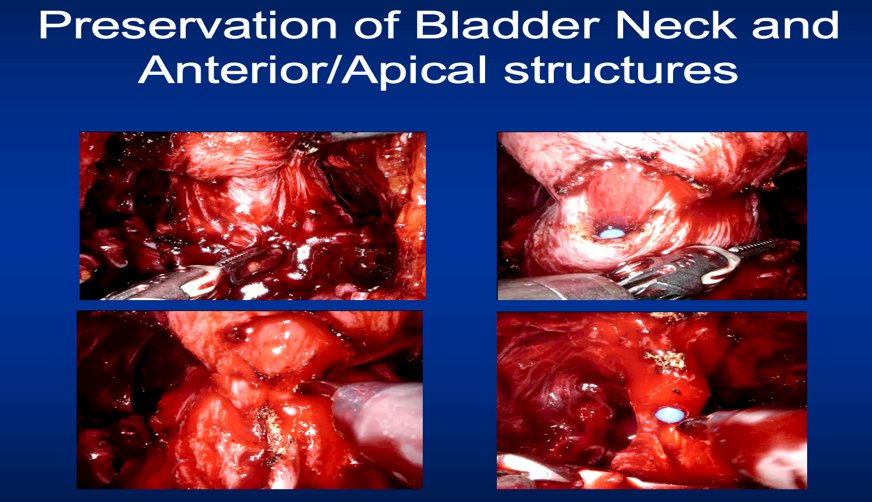
Moving on to the functional outcomes, Dr. Oh discussed the preservation of bladder function following the Retzius-Sparing Approach. He pointed out that after radical prostatectomy, common bladder dysfunctions, such as detrusor overactivity (DO), impaired contractility, and sphincter dysfunction, as well as urethral length shortening, can occur. However, there is a prevailing belief that continence outcomes are superior with the Retzius-Sparing Approach because bladder dysfunctions such as DO are either absent or minimal. Dr. Oh stressed the need for further studies to compare the Retzius-Sparing Approach with standard surgical techniques, especially with pre-and post-operative urodynamic assessments.
To support his presentation, Dr. Oh referenced a significant blind randomized controlled trial (RCT) published in 2017, which demonstrated that early recovery of continence was markedly better in patients who underwent the Retzius-Sparing Approach compared to those who received standard surgical care.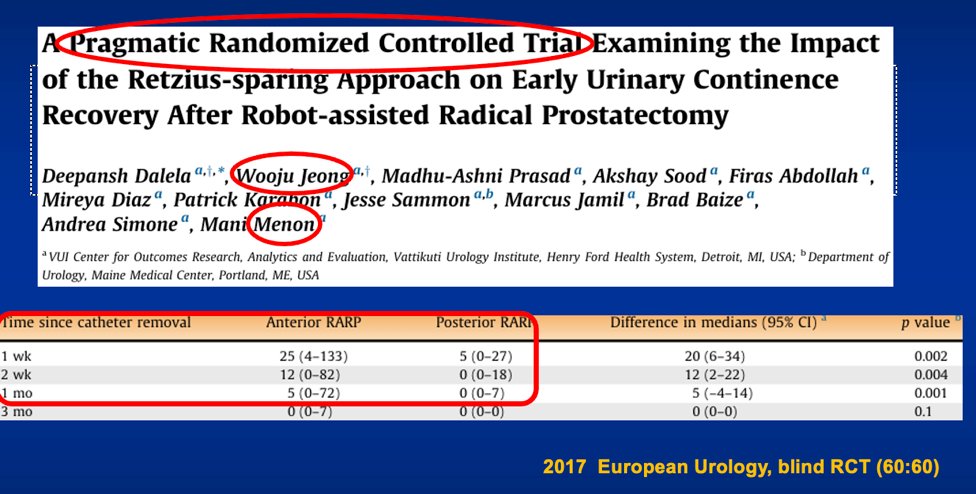
In conclusion, Dr. Oh affirmed that the Retzius-Sparing Approach is a highly effective technique for achieving superior continence outcomes through comprehensive preservation of anatomical structures, making it a valuable option for surgeons aiming to improve post-operative quality of life for their patients.
Following Dr. Oh’s comprehensive talk, the podium was passed to Dr. Jihad Kaouk, MD, FACS, FRCS, who discussed the Single-Port Robotic Radical Prostatectomy with a focus on the Transvesical Approach. Dr. Kaouk began by highlighting some of the remarkable features of the Single-Port (SP) Robotic Platform, which has been in use since 2018. This platform is purpose-built, featuring a narrow profile cannula with a diameter of just 2.5 cm, double articulating instruments, a floating docking technique, and improved maneuverability in limited surgical working spaces. Dr. Kaouk emphasized that the SP platform is not about simply having one incision or replacing the multi-port robot; rather, it is about regionalizing surgery to the relevant anatomy, allowing for more precise and effective procedures.
Dr. Kaouk then introduced his initial publication on the Single-Port Transvesical Approach from 2019. This approach involves direct percutaneous access into the bladder, and to date, Dr. Kaouk and his team have performed over 400 cases, including both radical and simple prostatectomies. The continence outcomes from these procedures were notably better than initially expected.
What makes the Single-Port Transvesical Access procedure is that it is performed with the patient in a supine position, as this approach does not require entry into the peritoneal space. A 4 cm midline suprapubic incision is made, similar to the procedure for suprapubic tube insertion, followed by bladder identification confirmed by urine aspirate. Once suprapubic access is established, the single-port robotic access kit is attached, as shown in the accompanying figures.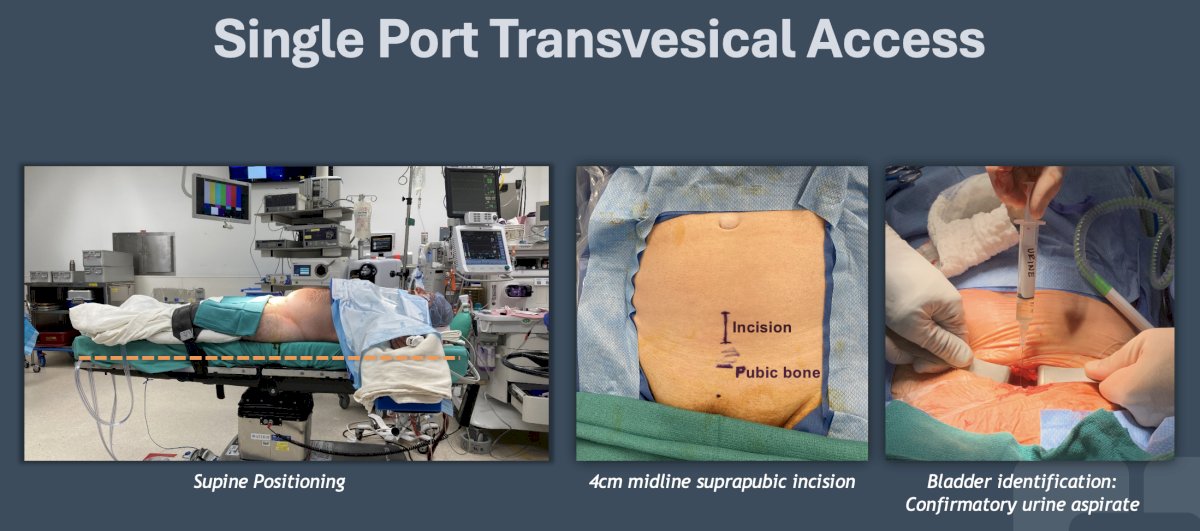
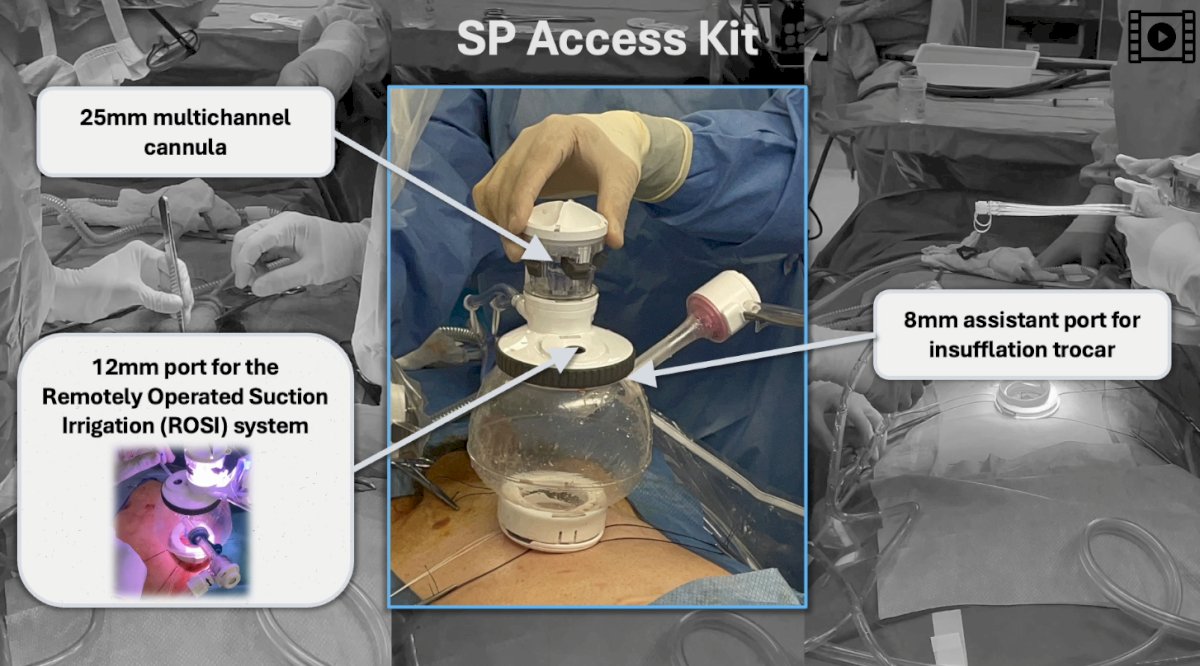
Dr. Kaouk emphasized that the access kit is composed of two rings: one inserted into the bladder and the other at the skin level. He then showcased a video of one of his cases, highlighting key aspects of the procedure. Dr. Kaouk pointed out that upon insertion of the robotic arm, the prostate becomes visible even in patients with a high Hostile Abdomen Index (HAI), which indicates multiple surgeries with significant scar tissue. These scars are not visible because they are located posterior to the bladder, making this approach particularly advantageous.

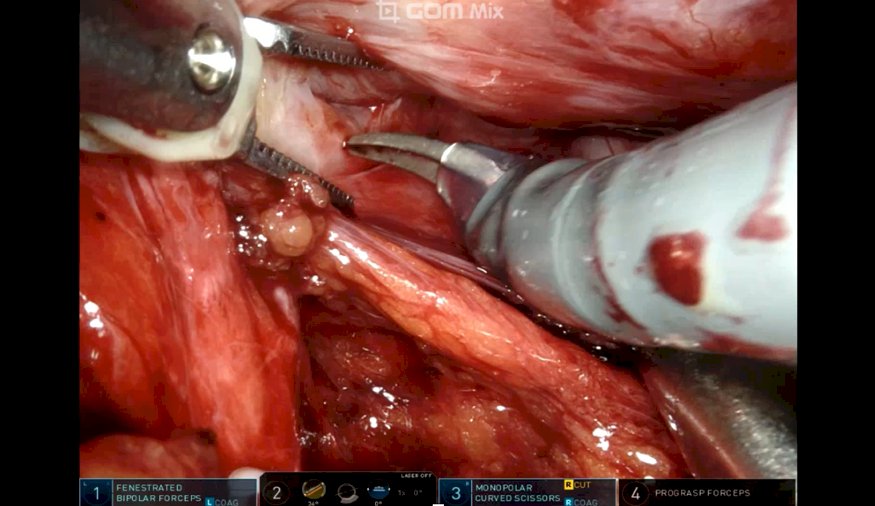
Another significant benefit of this access method is that the bowel and other gastrointestinal organs are neither touched nor visible during the procedure, allowing patients to have a meal on the day of surgery. The surgical steps begin with a posterior bladder neck dissection, performed with a "smiley face" incision. The surgeon remains outside the capsule, proceeding with vas deferens and seminal vesicle dissection. Dr. Kaouk noted that he prefers not to change the camera position during the procedure, maintaining a consistent visual field.
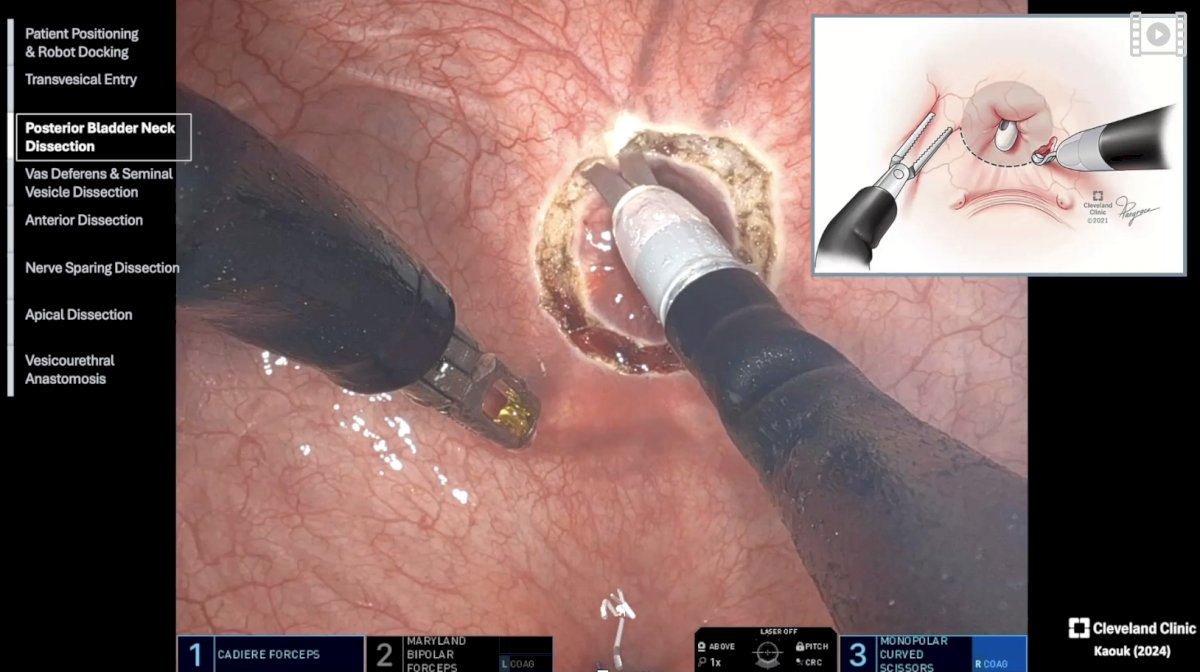
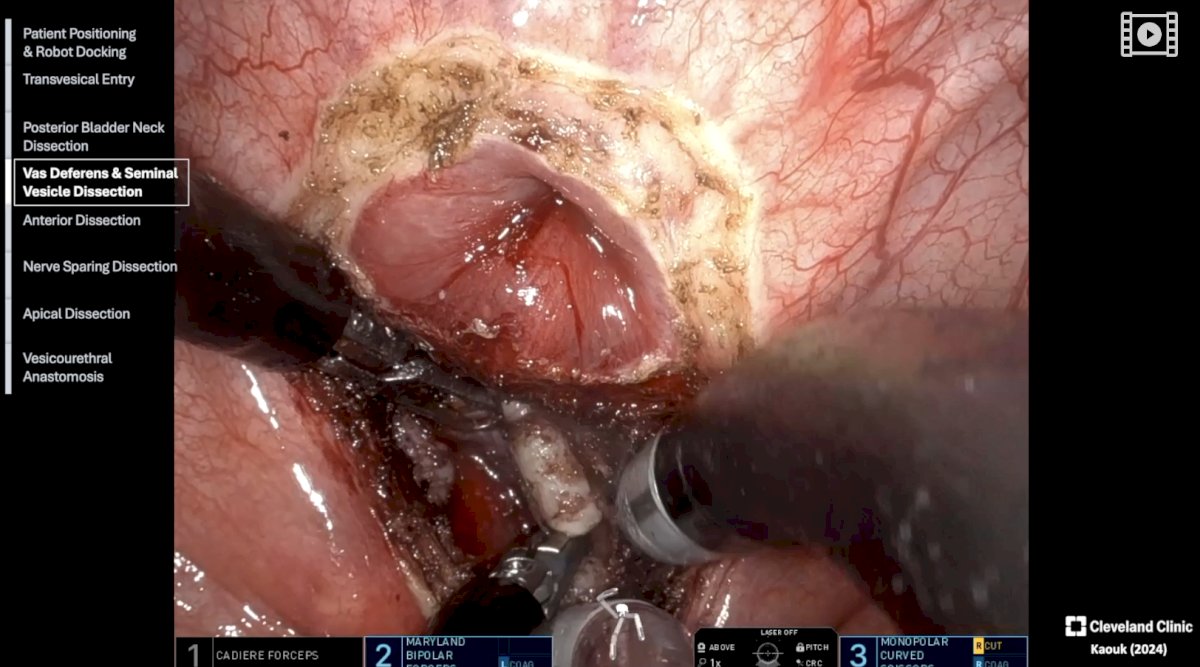
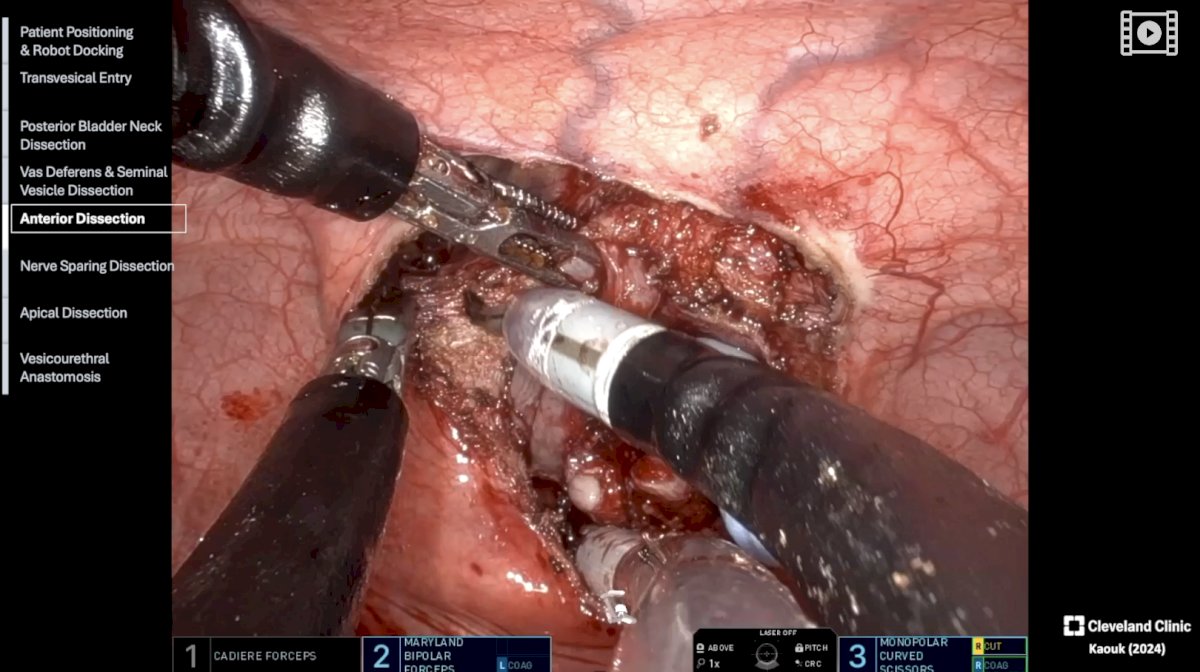
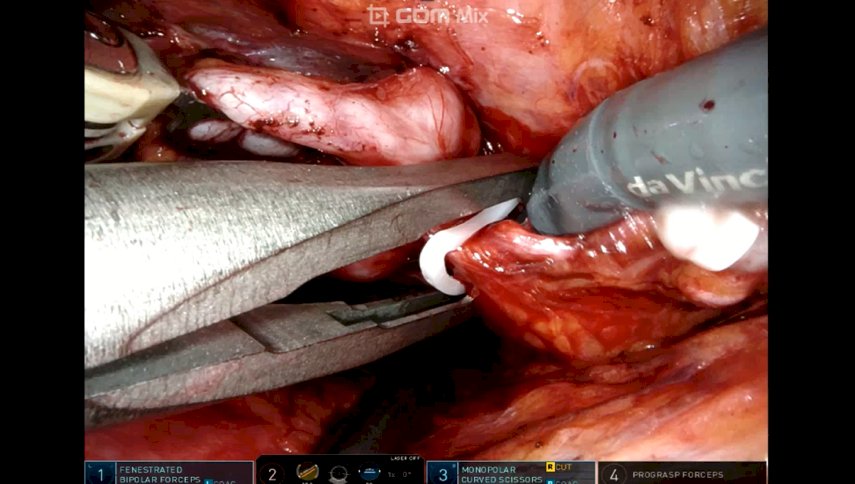
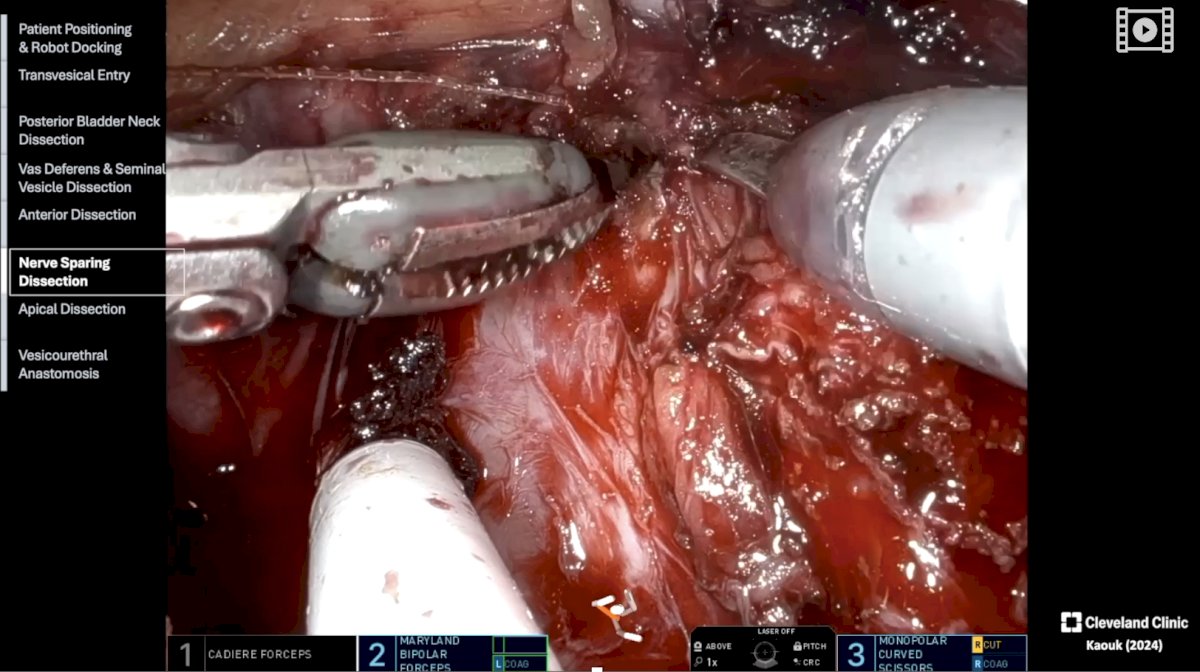
In terms of instrumentation, Dr. Kaouk uses scissors on the left, a bipolar device at the 6 o'clock position, and a grasper in the right hand. He then moves on to anterior dissection and sutures the dorsal vein, while keeping the interpelvic fascia intact and "unplugging" the prostate gland from its location. This technique preserves the nerves and neurovascular bundles, which remain in a hammock-like shape rather than being flattened against the body. The apical dissection follows, allowing for the easy release and removal of the prostate gland.

Dr. Kaouk also mentioned that the simplicity of the single-port system allows for the use of less experienced bedside assistants, ranging from medical students to fellows. The final step in the procedure is the vesicourethral anastomosis.

Following the procedural video, Dr. Kaouk's presentation focused on functional outcomes, particularly comparing single-port versus multi-port robotic prostatectomy with respect to the return to continence. A key finding was that 40% of patients experienced immediate urinary continence postoperatively, with only four days of Foley catheterization required.
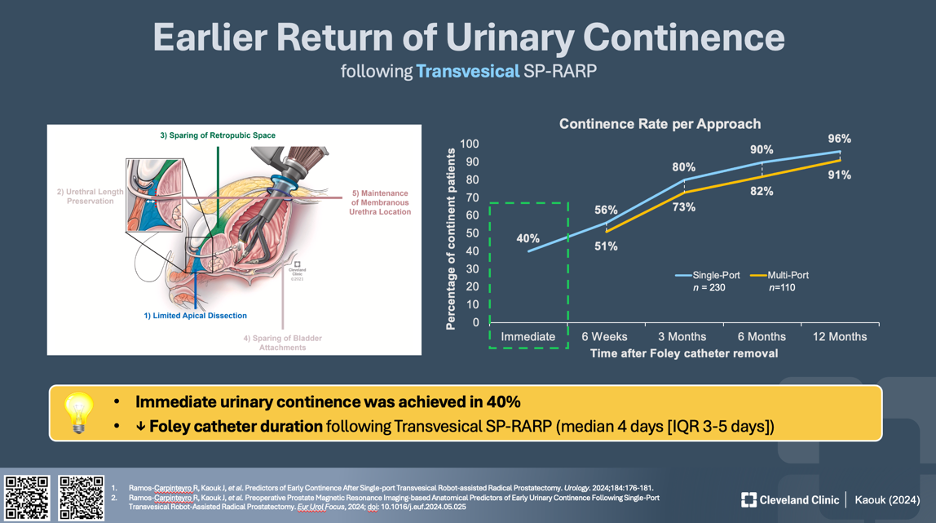
In conclusion, Dr. Kaouk summarized the key advantages of the Single-Port Transvesical Approach, noting the benefits of supine positioning, which enhances ventilation and facilitates surgery in patients with a hostile abdomen. He highlighted the reduction in postoperative pain, with 92% of patients being opioid-free, the potential for outpatient surgery with just a four-hour hospital stay, and the shorter duration of Foley catheterization. Additionally, the approach led to an earlier return of urinary continence, with 40% of patients being pad-free immediately, and allowed for a return to full activity within two weeks, reducing the risk of incisional hernia.
The final panelist of this plenary session was Dr. Sung Gu Kang, MD, PhD, Director of the Robotic Urologic Section at KSER and Professor in the Department of Urology at Korea University School of Medicine, who gave a thorough presentation on Minimal Apical Dissection (MAD) during robotic-assisted radical prostatectomy (RARP). Dr. Kang addressed the ongoing challenge of achieving better continence outcomes following RARP, noting that while the Retzius-sparing technique is recognized for its superior continence results, it is less commonly used and carries concerns about positive surgical margins, particularly in high-stage and high-risk cases.

Dr. Kang then introduced the concept of Modified Apical Dissection (MAD), an anterior approach that preserves anterior structures while minimizing the extent of apical dissection. This approach, sometimes referred to as the "Hood Technique," aims to balance the preservation of key anatomical structures with the need for effective cancer control, especially in high-stage disease.
Citing various studies, Dr. Kang presented data showing that the immediate continence rates following Retzius-sparing RARP ranged from 38% to 91% in non-comparative studies. Comparative studies showed that Retzius-sparing RARP offered better continence outcomes than standard RARP (S-RARP) at various follow-up points, including 1, 3, 6, 9, and 12 months postoperatively. This advantage was most pronounced in the early months following surgery.

Dr. Kang emphasized that careful apical dissection is critical for preserving quality of life (QOL) outcomes, particularly in terms of continence and erectile function. He pointed out that the cavernous erectile nerves swing anteriorly near the prostate apex, making this area particularly vulnerable to injury during surgery. Additionally, the pudendal nerve branches to the striated sphincter can be as close as 3-5 mm to the apex, further underscoring the need for precision during apical dissection.
The MAD technique involves minimal dissection at the apex while preserving the lateral prostatic fascia and other critical structures. Dr. Kang presented data from his research, showing that among 2168 patients who underwent RALP between 2017 and 2019, those who received MAD had significantly better continence recovery within the first six months compared to those who underwent conventional RALP techniques. Propensity score matching was used to ensure comparability between the groups.

A meta-analysis of eight studies further supported these findings, revealing that patients treated with MAD were four times more likely to regain continence at initial follow-up compared to those treated with conventional techniques. This trend continued with marked improvements at 1, 3, and 6 months postoperatively.
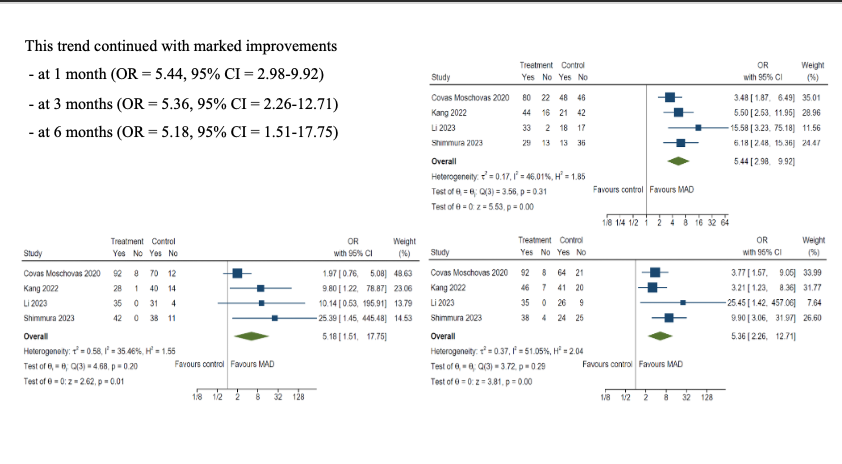
In conclusion, Dr. Kang asserted that the MAD technique offers a familiar and intuitive approach for surgeons, with similar early continence outcomes to the Retzius-sparing technique. Moreover, the MAD technique is applicable even in high-stage disease, including cases with anterior tumors, making it a versatile option for surgeons aiming to balance cancer control with functional preservation.
Presented by:
- Atsushi Takenaka, MD, PhD, Chairman, Professor of Clinical Urology, Tottori University, Tottori, Japan
- Cheol Kyu Oh, MD, PhD
- Jihad Kaouk, MD, FACS, FRCS, Professor & Zegarac-Pollock Endowed Chair in Robotic Surgery - Director, Center for Robotic and Image-Guided Surgery - Vice Chair of Research and Innovations
- Sung Gu Kang, MD, PhD - Director, Robotic Urologic Section of KSER - Professor, Department of Urology, Korea University School of Medicine - Director, Department of Urology, Korea University Anam Hospital - Director, Robotic Surgery Center, Korea University Anam Hospital
References:
- Kimura Y, Takenaka A, et al. Submitted (pending publication per authors).
- Cambio AJ, Evans CP, Shinghal R. Anatomic basis for surgical decisions in testicular cancer. Eur Urol. 2006;50(5):927-936.
- Kojima Y, Hayashi Y, Tozawa K, et al. Real-time elastography for the diagnosis of prostate cancer: Evaluation of elastographic moving images in patients with elevated PSA. Int J Urol. 2013;20(8):784-792.
- Rosenberg JE, Jung JH, Edgerton Z, Lee H, Lee S, Bakker CJ, Dahm P. Retzius-sparing versus standard robotic-assisted laparoscopic prostatectomy for the treatment of clinically localized prostate cancer. Cochrane Database Syst Rev. 2020 Aug 18;8(8): CD013641.
- Lenfant L, Kaouk J, Bertolo R, et al. Floating docking technique: A simple modification to improve the working space of the instruments during single-port robotic surgery. World J Urol. 2020;38(7):1631-1637.
- Ramos-Carpinteyro R, Kaouk J, Shoag J, et al. Predictors of early continence after single-port transvesical robot-assisted radical prostatectomy. Urology. 2024;184:176-181.
- Ramos-Carpinteyro R, Kaouk J, Shoag J, et al. Preoperative prostate magnetic resonance imaging-based anatomical predictors of early urinary continence following single-port transvesical robot-assisted radical prostatectomy. Eur Urol Focus. 2024; doi:10.1016/j.euf.2024.05.025
- Chierigo F, Kaouk J, Shoag J, et al. Long-term oncologic outcomes of single-port robot-assisted radical prostatectomy: A prospective, single-arm study. World J Urol. 2024;42(1):385.
- Hussein AL, Awan M, Gill I, et al. Variation in the use of active surveillance for low-risk prostate cancer across the United States: Results from a nationwide cancer database. Front Oncol. 2021;11:644885.
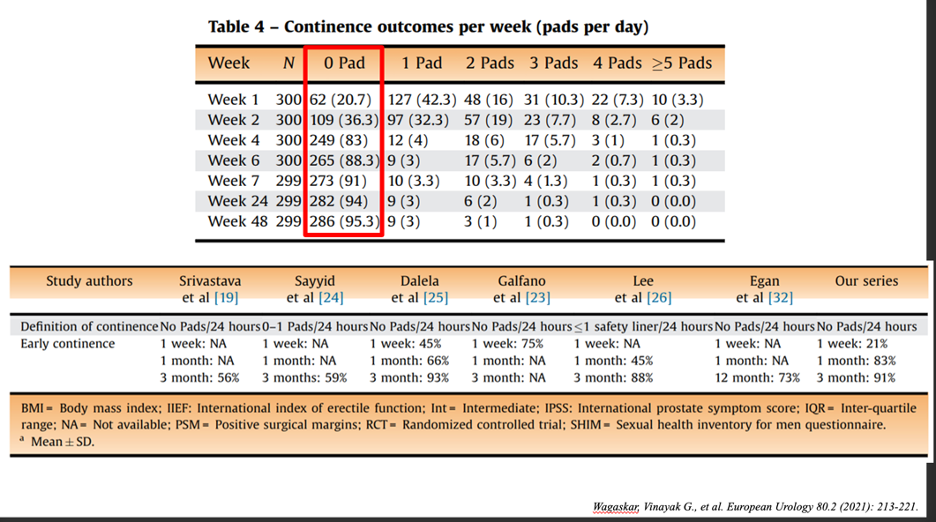
- Wagaskar VG, Mottrie A, Buffi N, et al. Single-port versus multiport robot-assisted radical prostatectomy: A propensity score-matched analysis of perioperative outcomes. Eur Urol. 2021;80(2):213-221.


