Endoscopic Approaches and Emerging Novel Treatments for Upper Tract Urothelial Carcinoma
Indications for Kidney Sparing/Endoscopic Management
- Imperative – patients with contraindications for radical surgery: (i) a solitary functioning kidney, (ii) bilateral upper tract urothelial cancer, (iii) baseline renal insufficiency, (iv) poor candidacy for hemodialysis or renal transplantation, (v) significant comorbidities
- Elective – patients with low-risk non-muscle invasive upper tract urothelial cancer. May be eligible for a partial nephrectomy, segmental ureterectomy, or endoscopic management
Ureteroscopic Management
Endoscopic evaluation, typically by ureteroscopy, is crucial for the initial diagnosis, risk stratification, and subsequent treatment planning for patients with upper tract urothelial cancer. Information from endoscopy helps assess tumor location, multifocality, architecture and allows the clinician to obtain a tissue diagnosis. However, ureteroscopic biopsies can be technically challenging given the limited ureteroscopic biopsy instruments that can traverse the small working channel. Some experts have advocated that the visual characteristics of the tumor may be able to predict disease aggressiveness, such as sessile-appearing tumors being more likely to be higher grade/stage .6 Several techniques for achieving a tissue diagnosis have been described, including multiple urine and washing samples and multiple quality biopsies to ensure sufficient tissue for pathological assessment; the most commonly used biopsy tools include the Piranha forceps (Boston Scientific, Marlborough, MA) and the BIGopsy forceps (Cook Medical, Bloomington, IN).2 For larger, papillary tumors, a stone basket (ie. nitinol) can be used for snaring and debulking the tumor.One of the benefits of a ureteroscopic approach is that a single procedure can be both diagnostic and therapeutic. When possible, use of a ureteral access sheath is ideal in that it allows atraumatic multiple insertions of the ureteroscope, especially important when encountered with a large tumor volume7. Following multiple biopsies for tissue diagnosis, a laser can be used both for additional tumor resection and fulguration (for hemostasis) of the tumor bed. The most commonly used lasers are the holmium:yttrium-aluminum-garnet (YAG) laser and the neodymium-doped (Nd):YAG laser. The holmium laser is typically better suited for smaller tumors, however, it requires contact with the tissue in order to be effective. The Nd: YAG laser has a smaller wavelength, is able to penetrate deeper (5-6 mm), and does not require direct tissue contact. Although less readily available, electrocautery resection is also possible with a 10-13Fr rigid ureteral resectoscope (Karl Storz Endoscopy, Tuttlingen, Germany); this scope allows resection of tumors similar to a loop used for transurethral resection of bladder tumors2.
Currently, there is no Level I evidence assessing oncologic outcomes of patients undergoing ureteroscopic management of upper tract urothelial cancer. Retrospective series to date are all limited to fewer than 100 patients. The largest retrospective series with more than two years of follow-up was published by Grasso and colleagues (n=82)8 noting 81% recurrence rate in the upper tract, 57% in the bladder, 19% of patients progressing to surgical resection, and a 74% and 87% overall and cancer-specific survival rate, respectively. Petros et al summarized these retrospective studies with the following outcomes:2
- Median follow-up: 24-58 months
- Upper tract recurrence rate: 65%
- Bladder recurrence rate: 44%
- Progression to surgical resection rate: 0-33%
- Overall survival rate: 35-100%
- Cancer-specific survival rate: 70-100%
Percutaneous Management
Antegrade percutaneous endoscopic treatment of upper tract urothelial carcinoma is typically reserved for patients with low-grade, large volume tumors that are either anatomically or technically challenging for ureteroscopic management, ie. lower pole tumors. This approach is particularly advantageous for patients that have had a prior cystectomy and urinary diversion. A major benefit of percutaneous management is the ability to use larger instruments that are able to fit through a nephroscope, including loop cautery for debulking large tumors. All of the laser biopsy instruments listed above for ureteroscopic management are also feasible for the percutaneous approach. The primary risk of percutaneous management of upper tract urothelial carcinoma (aside from those traditionally associated with percutaneous management of nephrolithiasis) is disruption of the urothelium, which may lead to a theoretically increased risk of tumor seeding into the retroperitoneum.2Similar to ureteroscopic management of upper tract urothelial carcinoma, oncologic outcomes have relied on retrospective studies of fewer than 100 patients. However, one study by Motamedinia et al.9 identified 141 patients who underwent percutaneous resection with a median follow-up of 66 months. They noted that recurrence occurred in 37% of low-grade patients and 63% of high-grade patients, with a median time to recurrence of 71.4 vs 36.4 months, respectively. On multivariable analysis, grade was the only predictor of recurrence (HR 2.12, p = 0.018) and radical nephroureterectomy was avoided in 87% of patients. Petros and colleagues2 summarized oncologic outcomes of percutaneous management among studies with a minimum 2-year follow-up (n=361):
- Median follow-up: 24-66 months
- Upper tract recurrence rate: 40%
- Bladder recurrence rate: 24%
- Progression to surgical resection rate: 6-50%
- Overall survival rate: 40-90%
- Cancer-specific survival rate: 75-100%
Emerging Novel Treatments
Several new and exciting treatments are under development with regards to minimally invasive treatment of upper tract urothelial cancer. As highlighted above, the recurrence rate for endoscopic management is high (40-65% on pooled analysis)2 and these approaches are not well suited to treatment of multifocal disease or carcinoma in situ. Thus, much research has been directed for improving the deliverability of topical agents to the upper tracts. One of the challenges is difficulty concentrating therapeutic levels of these agents in the upper tract for more than a brief period of time secondary to ureteral peristalsis rapidly draining topical treatment from the pelvis and ureter. Specifically, mitomycin C exposure time to the urothelium is critical for efficacy.10 RTGel™ is a reverse-thermal hydrogel composed of a combination of polymers that allows it to exist as a liquid at cold temperatures but solidifies to a gel state at body temperature.11 This product was developed to address the constraints of the upper urinary tract, where continuous urine production and ureteral peristalsis prevents drug retention in the upper tract. Subsequently, MitoGel Ôwas developed as a novel formulation of RTGel combined with mitomycin C. The hypothesis for MitoGel is that upon delivery to the upper urinary tract, MitoGel would gelatinize and urine would produce a slow dissolution of the gel, allowing a sustained release of mitomycin C into the upper tract allowing prolonged exposure to the urothelium. Using a preclinical swine animal model (n=23), Donin et al,11 noted that after antegrade instillation of MitoGel, the product remained visible in the pelvicalyceal system on fluoroscopic and computed tomography imaging for 4-6 hours after instillation. Furthermore, on necropsy, they noted that mitomycin C plasma levels were well within acceptable safety thresholds and that there was no evidence of urinary obstruction, acute kidney injury, sepsis, or myelosuppression. Donin and colleagues subsequently confirmed these safety results in a study assessing six once-weekly unilateral retrograde instillations of Mitogel.12The OLYMPUS study (NCT02793128) is a prospective single-arm ongoing clinical trial designed to assess the efficacy, safety, and tolerability of MitoGel in patients with low grade, noninvasive upper tract urothelial cancer. Eligible patients are treated with MitoGel once weekly for a total of six times in a retrograde fashion; patients demonstrating a complete response are treated with MitoGel once monthly for a total of 11 instillations as maintenance, or until the first recurrence. The primary outcomes are complete response rate defined as the percent of patients with complete response at the primary disease evaluation visit (~11 weeks), and adverse event rates (over ~2 years). Secondary outcomes include:
(i) Long-term durability of complete response (12 months)
(ii) Complete response rates at 3, 6, and 9 months
(iii) Partial response to treatment (~11 weeks)
(iv) Mitomycin C level in blood plasma
The target recruitment goal is 71 patients with an estimated study completion date of February 2020.
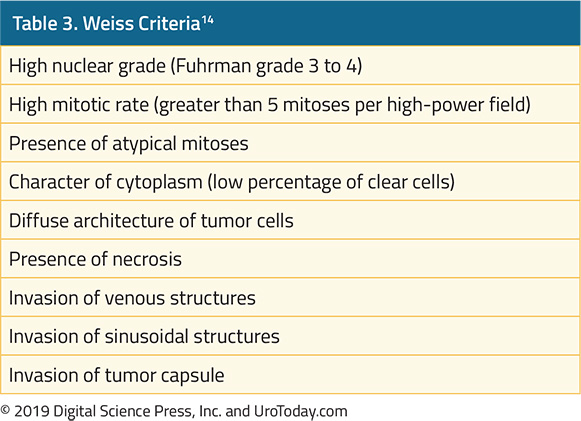
Previous studies assessing differential gene expression between upper tract and bladder urothelial carcinoma using microarray data suggest that upper tract tumors tend to have high expression of genes associated with a luminal subtype.13 Furthermore, one particular gene highly expressed in upper tract tumors is SLITRK6, an integral membrane protein known to have high levels of expression in certain carcinomas, but low levels in the majority of other tissues.14 An antibody to SLITRK6 protein has been developed and linked to a cytotoxic agent called monomethyl auristatin E (AGS15E), a microtubule-disrupting agent.15, 16 ASG-15C was chosen among seven anti-SLITRK6 antibodies and monomethyl auristatin E was chosen due to its efficacy in tumor inhibition and regression. Upon binding to SLITRK6, ASG-15ME is rapidly internalized and trafficked to lysosomes and early endosomes. An ongoing Phase I dose escalation trial of AGS15E in patients with metastatic urothelial carcinoma presented initial interim trial results at the ESMO 2016.17 This trial includes patients previously treated with ≥ 1 prior chemotherapy regimens; SLITRK6 expression was determined by immunohistochemistry. Disease assessments were performed every 8 weeks using RECIST v 1.1 criteria and ASG-15ME was administered IV weekly for 3 out of every 4 weeks until no further benefit. Six dose levels were assessed: 0.1, 0.25, 0.5, 0.75, 1, and 1.25 mg/kg. At the time of analysis, 51 pts were enrolled and 93% were SLITRK6 positive. Of 42 evaluable patients at doses considered active (doses ≥0.5 mg/kg), one had a complete response and 13 had a partial response (ORR =33%). Adverse event rate was high (91%) and the most common treatment-related adverse event was fatigue (44%). Serum concentrations of ASG-15ME decreased multi-exponentially and half-life was 3.1 days. In heavily pre-treated individuals, novel antibody-drug conjugates continue to be explored for therapeutic benefit.
Conclusions
Endoscopic management of upper tract urothelial cancer is technically feasible but associated with high rates of recurrence and non-insignificant rates of progression necessitating radical surgical treatment. Endoscopic management should be reserved for low-grade tumors and patients that have contraindications to radical nephroureterectomy. Research is ongoing, particularly for improving delivery of topical agents to decrease recurrence rates.Published Date: April 15th, 2019